Translate this page into:
Isolated Renal Lymphoma Presenting with Hypercalcemia and Acute Kidney Injury: A Case Report
-
Received: ,
Accepted: ,
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Dear Editor,
Primary renal lymphoma (PRL) represents 1% of all extra nodal lymphomas.[1] Diffuse large B cell lymphoma (DLBCL) is the most common type of primary renal lymphoma.[2] The most common cause of unilateral exophytic renal mass is generally renal cell carcinoma (RCC). Thus, PRL is usually confused with RCC, and either computed tomography (CT)-guided biopsy or excision biopsy is the gold standard for its diagnosis.[3]
A 63-year-old woman presented with complaints of generalized weakness of three months, lower backache, loss of appetite, weight loss since one month, and altered sensorium since two days. She had no complaints of fever, vomiting, cough, seizure, blurring of vision, headache, or decreased urine output. She had hypertension and chronic bronchitis for eight to nine years. On examination, we found that she was afebrile, had a pulse rate of 80/min, blood pressure of 180/100 mmHg, and an oxygen saturation of 98% on room air with a respiratory rate of 18 breaths/min. On examining the nervous system, we noted that she was disoriented in terms of time, place, and person without any focal neurological deficits. Her cardiovascular and respiratory system examination were normal. Abdomen examination revealed a bimanually palpable, ballotable mass in the right lumbar region that moved with respiration. She had no other organomegaly. Laboratory investigations are given in Table 1.
| Investigation | Result | Investigation | Result | Investigation | Result |
|---|---|---|---|---|---|
| Hemoglobin | 9.8 g/dl | TSH | 5.02 µIU/ml | S. Calcium | 16.4 mg/dl |
| Total white blood cells | 10060 | TT3 | 0.992 ng/ml | iPTH | 8.6 pg/ml |
| Platelets | 2.84 lacs | TT4 | 32 units/L | Vit. D level | 58.6 ug/L |
| S. Urea | 65 mg/dl | ACE level | 15.9 | S. Proteins (total/albumin/globulin) | 6/3.5/2.5 g/L |
| S. Creatinine | 1.78 mg/dl | SGPT | 18 u/L | S. Phosphorous | 4.5 mg/dl |
| S. Sodium | 135 mmol/L | SGOT | 68 u/L | S. Magnesium | 2.2 mg/dl |
| S. Potassium | 3.6 mmol/L | VDRL | Negative | Urine routine | Protien+1, rest nad |
TSH: Thyroid stimulating Hormone. TT3: Total T3 level. TT4: Total T4 level. iPTH: Intact Parathyroid Hormone. ACE: Angiotensinogen Converting Enzyme. VDRL: Venereal Disease Laboratory Test. SGPT: Serum Glutamic Pyruvic Transaminase. SGOT: Serum Glutamic-Oxaloacetic Transaminase
Ultrasonography (USG) showed 11 × 12 × 15 cm exophytic heterogeneous mass lesion with internal vascularity suggestive of renal mass that was accompanied by encasement of the right renal artery. Fibroblast activation protein inhibitor (FAPI) positron emission tomography (PET) scan showed large, lobulated, heterogeneously enhancing lesion, peripherally tracer avid with central areas of necrosis arising from mid and upper pole of the right kidney and involving almost entire right hypochondrium. It measured about 15.2 × 15.3 × 17.7cm with encasement of right renal artery, infrahepatic inferior vena cava and bilateral renal vein without thrombosis or distant metastasis [Figure 1]. The mass was adjourned to be inoperable, and USG-guided biopsy showed the mass to be a malignant round cell tumor with immunohistochemistry (IHC) positive for LCA, CD20, and “BCL-2” and negative for “BCL-6”, CD10, CD99, “CMyc”, and CyclinD1 with a Ki67 proliferative index >90%, which was suggestive of high-grade B cell lymphoma of DLBCL type.
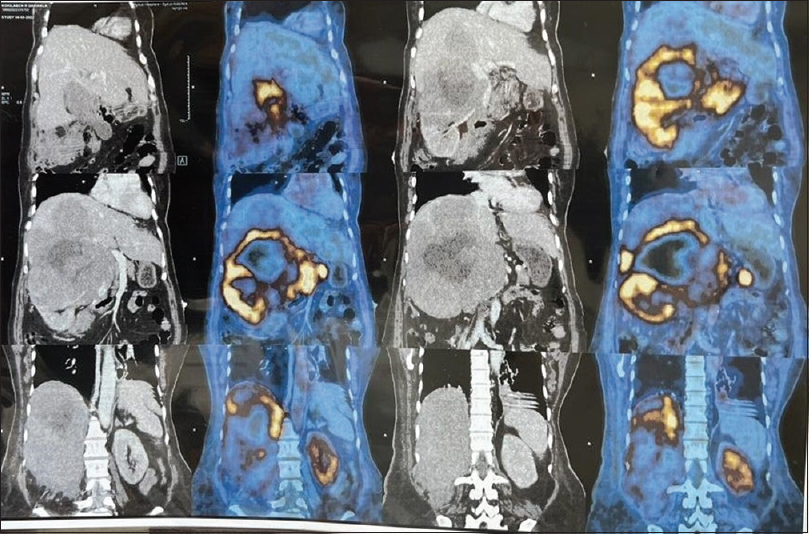
- FAPI PET CT scan showing a right renal mass lesion with vascular encasements (golden areas suggestive of metabolically active radiotracer uptake)
The patient was started on primary treatment for hypercalcemia with fluids and diuretics, calcitonin, denosumab, and steroids. She responded to it, became conscious and oriented, and her serum creatinine level came down to 1.1 mg/dl. Further treatment was advised in the form of rituximab and bendamustine.
Features that favor PRL over RCC are the absence of calcification, absence of renal vein thrombus, and absence of a mass effect on renal vessels and the pelvicalyceal system.[4] This was a very rare case of large right renal mass that was initially thought to be RCC, owing to its presentation of unilateral exophytic mass with vascularity. Her biopsy showed the lesion to be DLBCL, which presented as hypercalcemia-induced encephalopathy. Hypercalcemia was thought to be due to bony metastasis, but FAPI PET CT showed no bony involvement and the hypercalcemia was hence likely secondary to a parathyroid hormone–related protein (PTHrP) secretion by a tumor. DLBCL presenting with hypercalcemia has an aggressive course and poor prognosis.[5]
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Primary renal lymphoma mimicking renal cell carcinoma. Indian J Urol. 2010;26:441-3.
- [Google Scholar]
- Renal Lymphoma. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022. [Updated 2021 Dec 12]
- [Google Scholar]
- Imaging of renal lymphoma: Patterns of disease with pathologic correlation. Radiographics. 2006;26:1151-68.
- [Google Scholar]
- Prevalence and clinical significance of hypercalcemia at diagnosis in diffuse large B-cell lymphoma. Leuk Lymphoma. 2019;60:2922-6.
- [Google Scholar]






