Translate this page into:
Life-threatening Wunderlich Syndrome in a Patient with Solitary Kidney Successfully Managed by Nephron-sparing Approach
Address for correspondence: Dr. Praveen Kumar Etta, Department of Nephrology and Renal Transplantation, Asian Institute of Nephrology and Urology, Hyderabad - 500 082, Telangana, India. E-mail: drpraveen85@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
A 50-year-old man with chronic kidney disease (CKD) and left solitary kidney presented with sudden-onset severe pain in the left loin region, nausea and vomiting for the past 5 days. There was no history of fever, chest pain, hematuria, and lower urinary tract symptoms. He denied any abdominal trauma. He had undergone right nephrectomy elsewhere 14 years ago for an episode of massive retroperitoneal bleed from the right kidney. On examination, he had severe pallor; pulse rate was 96/min and his blood pressure was 100/60 mmHg. He also had characteristic facial skin lesions of angiofibromas, causing cosmetic disfigurement [Figure 1]. Laboratory findings revealed hemoglobin of 6.2 g/dl, blood urea of 46 mg/dl, and serum creatinine of 2.2 mg/dl with estimated glomerular filtration rate [eGFR] by Modification of Diet in Renal Disease study [MDRD] equation was 32 ml/min/1.73m2 body surface area [BSA]). His urine examination showed trace albumin, 8–10 RBC/hpf, and 6–8 pus cells/hpf. On further evaluation, he was found to have a large perinephric hematoma surrounding the solitary left kidney with multiple angiomyolipomas (AMLs) and renal cysts [Figure 2]. Wunderlich syndrome from a ruptured AML lesion was diagnosed. In view of multiple angiofibromas over the skin, renal AMLs, and renal cysts, a definitive diagnosis of tuberous sclerosis (TSC) was made, although genetic testing was not done.[1] In view of compromised total renal mass with underlying CKD, we managed him by nephron-sparing surgery with left partial nephrectomy and open hematoma drainage. At 3 months of follow-up after surgery, his renal functions remained stable with eGFR of 29 ml/min/1.73m2 BSA (serum creatinine of 2.4 mg/dl).

- Facial angiofibromas (adenoma sebaceum) causing cosmetic disfigurement in the patient with tuberous sclerosis
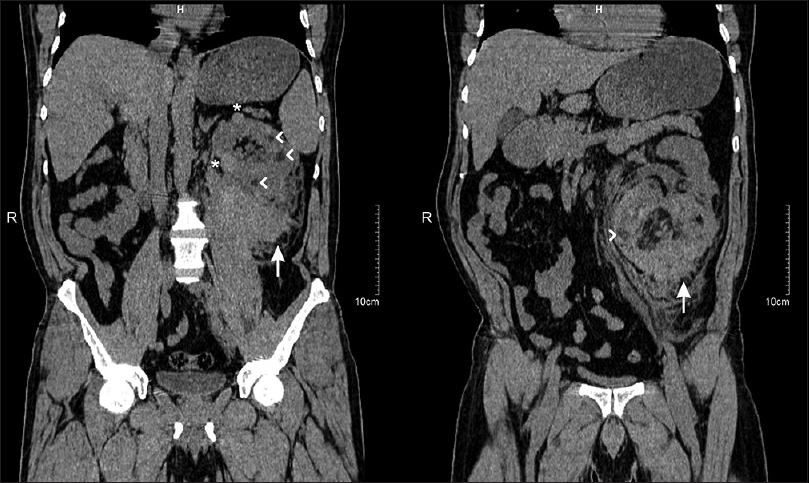
- Plain computed tomography (CT) coronal images showing solitary left kidney with multiple renal cysts (*), multiple AMLs (arrow heads) with large extracapsular left perinephric hematoma (arrows) extending up to iliac fossa
TSC, also known as Bourneville syndrome, is a neurocutaneous disorder with autosomal dominant inheritance, with an incidence of approximately 1 in 5000 to 10,000 live births. TSC2 (tuberin, on chromosome 16) mutations produce more severe phenotype than TSC1 (hamartin, on chromosome 9) mutations. TSC is associated with development of a variety of benign tumours in multiple organs, including the brain, heart, skin, eyes, kidney, lung, and liver. The common skin lesions include hypopigmented macules (ash-leaf spots), facial angiofibromas (adenoma sebaceum), and Shagreen patches. The classic diagnostic triad of seizures, mental retardation, and facial angiofibromas (Vogt triad) occurs in less than one-third of the patients. The diagnostic criteria of TSC is based upon genetic testing results and/or clinical findings.[1] The renal manifestations include AMLs, renal cysts, and rarely, renal cell carcinoma. Their prevalence increases with age, ultimately affecting up to 80% of the patients. AML is the most common renal lesion; they are more numerous and reach a larger size in women than in men. Most AMLs are asymptomatic, but they may present with symptoms related to hemorrhage, hypertension, renal insufficiency, and mass effect. Wunderlich syndrome is a life-threatening, nontraumatic renal hemorrhage most commonly occurring due to rupture of renal AMLs. Increased vascularity (as seen in pregnancy), larger aneurysms within the AML (>5 mm), and larger AMLs (>4 cm) are associated with an increased risk of rupture.
In cases of life-threatening hemorrhage caused by a ruptured AML, total nephrectomy has been considered in the past for complete cure and to save the life of the patient. Because of the frequent bilaterality of renal lesions in TSC, nephron-sparing interventions should be performed whenever possible. These include surgery (partial nephrectomy or enucleation), selective renal artery embolization, and radiofrequency or cryoablation.[2] These are especially preferred and useful in cases of compromised renal mass with CKD, as in our patient, to prevent rapid progression to end-stage renal disease.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- International Tuberous Sclerosis Complex Consensus Group. Tuberous sclerosis complex diagnostic criteria update: Recommendations of the 2012 International Tuberous Sclerosis Complex Consensus Conference. Pediatr Neurol. 2013;49:243-54.
- [Google Scholar]






