Translate this page into:
Lupus Nephritis with Coexistent Antiphospholipid Antibodies Associated Nephropathy: A Case Report and Literature Review
Address for correspondence: Dr. U. Anandh, Department of Nephrology, Yashoda Hospitals, Alexander Road, Secunderabad, Hyderabad - 500 014, Telangana, India. E-mail: patrickanusha@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Antiphospholipid syndrome (APS) associated nephropathy is a distinct clinical entity and can occur in patients with systemic lupus erythematosus (SLE) independent of or associated with lupus nephritis. Associated APS nephropathy in a patient with lupus predicts poor renal outcome, especially if left untreated. Recognizing a coexistent APS nephropathy in a patient with lupus nephritis is of utmost importance. Here, we present a patient with severe lupus nephritis with antiphospholipid antibodies (aPLs) who had no thrombotic manifestations of APS clinically. On renal biopsy, she was found to have APS nephropathy. Remission was achieved after 3 months of anticoagulation and immunosuppression. This case illustrates the importance of renal biopsy in a patient of SLE with aPLs. Renal biopsy often alerts a treating rheumatologist of the presence of thrombotic involvement in such patients, thereby altering the treatment of such patients.
Keywords
Antiphospholipid antibodies
renal biopsy
systemic lupus nephritis
Introduction
Renal manifestations in systemic lupus erythematosus (SLE) can be varied and can involve any compartment – glomeruli, tubulointerstitium, and vessels. Most common among them is lupus nephritis which affects 50%–60% of patients in the initial 10 years of illness. Other renal manifestations in lupus include thrombotic microangiopathy (TMA), primary or secondary to antiphospholipid syndrome (APS), interstitial nephritis, vasculitis, arteriosclerosis, or lupus vasculopathy.[1]
SLE and APS can involve the kidney independent of each other or simultaneously. Distinguishing renal involvement due to APS versus SLE is of utmost importance to plan further management. Here, we describe a patient with SLE and APS with renal involvement due to lupus nephritis and APS nephropathy. This case report is followed by a short literature review on APS nephropathy in lupus.
Case Report
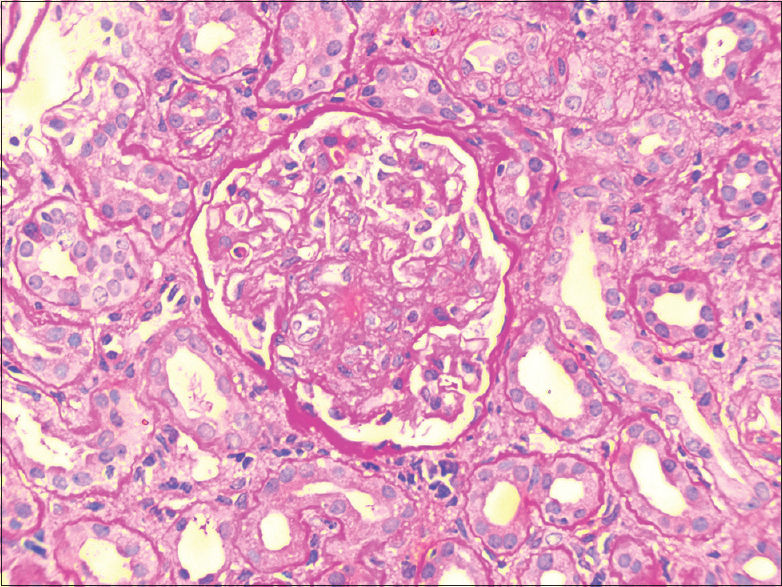
A 25-year-old female presented to us with 1-week history of fever, malar rash, cough, streaky hemoptysis, and worsening breathlessness. Her history was significant for an intrauterine death 8 months back due to severe preeclampsia with positive anticardiolipin antibodies (aCL IgG = 60 GPL units) and then with no further evaluation following the pregnancy. Examination revealed hypertension, multiple petechiae, nonscarring alopecia, bilateral lung crepitations, and wheeze. Her blood picture showed normocytic normochromic anemia with normal reticulocyte count and normal bilirubin, leukopenia, and thrombocytopenia. She had 2.7 g proteinuria with an active urinary sediment and serum creatinine of 2 mg/dl [Table 1]. Chest X-ray showed bilateral diffuse infiltrates with computed tomography chest showing evidence of multiple areas of consolidation in both lung fields. Sputum culture grew Klebsiella. Antinuclear antibody was positive with anti-Sjögren Syndrome A, anti-ribonucleoproteins, and anti-ribosomal P being positive on immunoblot. Serum complement levels were low. Her activated partial thromboplastin time (APTT) was abnormal (patient 126 s, control 28 s) with a normal prothrombin time.
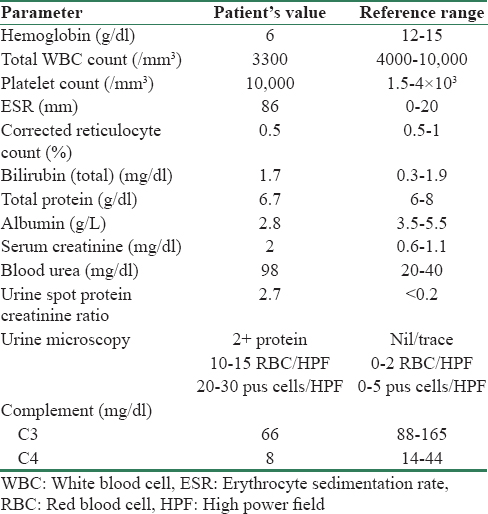
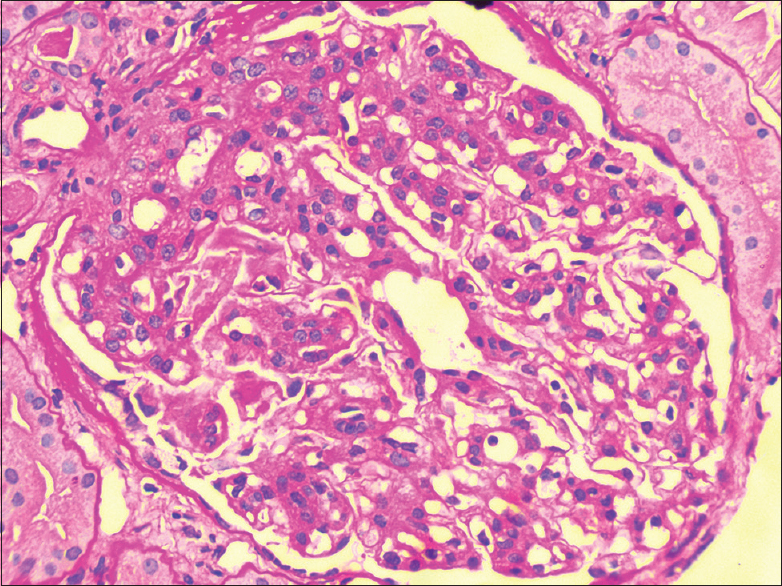
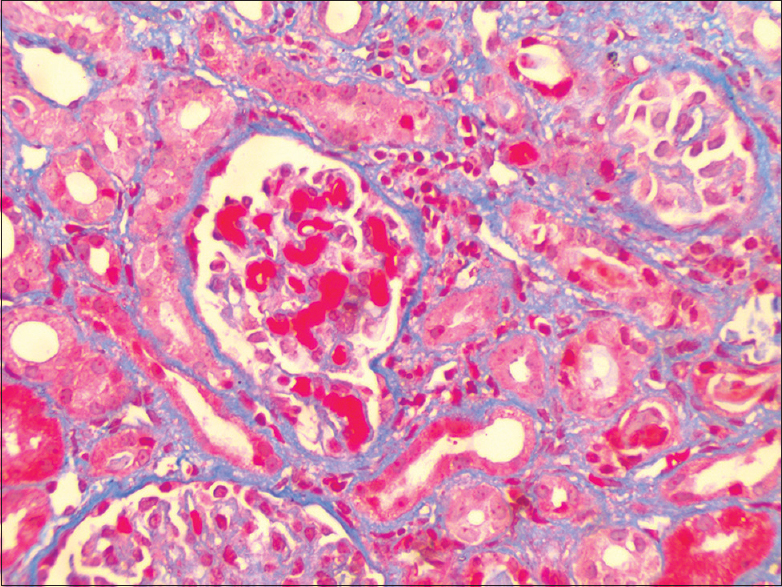
A diagnosis of SLE with APS was made with cutaneous, hematologic and renal involvement. At the time of diagnosis, the patient was suffering with bronchopneumonia. The patient was started on methyl prednisolone pulse (1 g/day for 3 days) followed by 1 mg/kg prednisolone along with appropriate antibiotics and antihypertensives (amlodipine, furosemide, prazosin extended release). She was planned for plasma exchange or intravenous immunoglobulin if clinical condition worsened. Her blood counts improved, creatinine normalized, and lung infiltrates recovered in the next 1 week. Telmisartan was added. A renal biopsy was done after her platelet count rose and APPT normalized. Renal biopsy showed enlarged, hypercellular glomeruli with increase in mesangial and endocapillary cellularity [Figure 1], neutrophilic infiltration, and mesangiolysis [Figure 2]. Intracapillary fibrin thrombi [Figure 3], ischemic wrinkling of a glomerulus with mild tubular atrophy, interstitial fibrosis were also noted with one small artery showing intimal endothelial cell swelling and near-total luminal occlusion. The pathological diagnosis was consistent with Class IV lupus nephritis with APS nephropathy. Based on this biopsy report, besides steroids, mycophenolate mofetil and warfarin were also added. Three months after starting her treatment, the patient is in complete remission.
- Renal biopsy showing diffuse mesangial and endocapillary hypercellularity
- Renal biopsy showing intraglomerular hyaline thrombi
- Renal biopsy showing mesangiolysis
Discussion
Thrombosis in any vessel is the main pathophysiology that underlies clinical manifestations of APS, with a histopathologic appearance of thrombotic occlusion of a vessel without inflammatory infiltrates in the vessel wall. Renal involvement in APS is a spectrum which includes renal artery stenosis and thrombosis, renal vein thrombosis, cortical infarcts, and TMA.[2]
APS nephropathy is a distinct entity defined histopathologically acutely by TMA and in chronic cases by the characteristic triad of fibrous intimal hyperplasia, focal cortical and tubular atrophy, and interstitial fibrosis in a patient with primary or secondary APS. Most cases of APS nephropathy are either asymptomatic or have hypertension with evidence of proteinuria and/or active urinary sediments and/or raised creatinine in varying combination. Seventy-one percent of patients with catastrophic APS present with renal involvement. ESRD however is a rare complication in APS nephropathy.[3] The present consensus from the International Task Force on APS suggests that APS nephropathy may be considered a clinical criterion for “definite” APS.[4]
TMA is characterized by the presence of fibrin thrombi in glomeruli with no inflammatory cells and immune deposits. TMA has been noted in 20% of patients with primary APS. Fibrous intimal hyperplasia is due to proliferation of myofibroblasts and intimal thickening of arterioles with consequent luminal narrowing. Focal cortical atrophy is characterized by wedge-shaped infarcts with atrophy of all renal parenchymal structures in the superficial cortex and changes in contour of renal capsule. Tubules are atrophic, are filled with eosinophilic casts, and are termed tubular thyroidization.[3] In certain cases, the histopathological changes may be subtle in the form of hyaline thrombi in intraglomerular capillaries and mesangiolysis as noted in our case.
Antiphospholipid antibodies (aPLs) were first described in patients with lupus. aPLs are found in 30%–40% of patients with lupus. However, 10%–15% of patients with SLE develop clinical manifestations of APS. The presence of aPLs itself independently predicts renal function deterioration in lupus nephritis.[5] Incidence of APS nephropathy in patients of lupus who have aPL positivity and undergo renal biopsy can be as high as 40% either independent of or in combination with lupus nephritis.[6] Patients with APS nephropathy are more likely to have hypertension and increased serum creatinine and have a poor renal outcome as compared to lupus nephritis without APS nephropathy.[5] A few studies contradict overall poor prognosis in APS nephropathy associated with SLE.[7] This highlights an additional importance of renal biopsy in a patient with lupus nephritis beyond just assigning the ISN/RPS class.
Renal biopsy is always essential in a patient with suspicion of APS nephropathy as it is difficult to distinguish clinically and by laboratory investigations APS nephropathy and lupus nephritis. There have been many publications on angiogenic and antiangiogenic factors in distinguishing lupus nephritis, APS nephropathy, and preeclampsia with no firm conclusions obtained.[8]
Treatment of APS nephropathy is predominantly extrapolated from the management of APS with no long-term observational studies. The present consensus suggests starting anticoagulation in all patients along with hydroxychloroquine, angiotensin-converting enzyme inhibitors, or angiotensin receptor blockers, and if there is no improvement, antiplatelets may be added or a higher international normalized ratio of 3–4 may be targeted with anticoagulation.[910]
Our case thus highlights an important comorbid renal condition that may be associated with lupus nephritis, the need for renal biopsy and for anticoagulation in addition to immunosuppression in such patients. Often, renal biopsy is not done because of thrombocytopenia and abnormal APTT in these patients. An adequate clinical suspicion and testing for aPLs when necessary are crucial in determining long-term renal prognosis in lupus patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- American College of rheumatology guidelines for screening, treatment, and management of lupus nephritis. Arthritis Care Res (Hoboken). 2012;64:797-808.
- [Google Scholar]
- Task force on catastrophic antiphospholipid syndrome (APS) and non-criteria APS manifestations (I): Catastrophic APS, APS nephropathy and heart valve lesions. Lupus. 2011;20:165-73.
- [Google Scholar]
- Antiphospholipid syndrome nephropathy in patients with systemic lupus erythematosus and antiphospholipid antibodies: Prevalence, clinical associations, and long-term outcome. Arthritis Rheum. 2004;50:2569-79.
- [Google Scholar]
- Antiphospholipid syndrome nephropathy (APSN) in patients with lupus nephritis: A retrospective clinical and renal pathology study. Rheumatol Int. 2014;34:535-41.
- [Google Scholar]
- The use of angiogenic and antiangiogenic factors in the differential diagnosis of pre-eclampsia, antiphospholipid syndrome nephropathy and lupus nephritis. Lupus. 2014;23:1299-301.
- [Google Scholar]
- Joint European league against rheumatism and European renal association-European dialysis and transplant association (EULAR/ERA-EDTA) recommendations for the management of adult and paediatric lupus nephritis. Ann Rheum Dis. 2012;71:1771-82.
- [Google Scholar]







