Translate this page into:
Membranous Nephropathy in a Treatment Naïve Patient of Rheumatoid Arthritis
Corresponding author: Rahil Arora, Department of Internal Medicine, Armed Forces Medical College, Wanowrie, Pune, India. E-mail: rahilarora1992@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kumar S, Singh SK, Arora R, Kashif AW. Membranous Nephropathy in a Treatment Naïve Patient of Rheumatoid Arthritis. Indian J Nephrol. 2024;34:543-4. doi: 10.25259/IJN_40_2024
Dear Editor,
A 45-year-old woman presented with a one-month history of generalized body swelling Over the preceding month, she had gained 8 kg in weight, experienced reduced urine output, and reported easy fatigability. The patient also disclosed a two-year history of inflammatory polyarthritis affecting small joints in her hands and wrists, with no prior treatment. Clinically, she was afebrile, with normal vitals and her weight was noted to be 92 kg.
Evaluation revealed normocytic normochromic anemia (hemoglobin 9.3 g/dL), low serum albumin (1.2 g/dL), elevated serum cholesterol (333 mg/dL), hypertriglyceridemia (311 mg/dL), serum creatinine within normal limits (1.0 mg/dL), and an estimated glomerular filtration rate (eGFR) of 71 ml/min/1.73 m2. Urine analysis showed proteinuria (3+ on dipstick, 8 g/day on the 24-hour collection). Chest X-ray displayed blunting of bilateral costophrenic angles. While an ultrasound of the kidneys indicated normal size, her renal biopsy confirmed membranous nephropathy (MN).
Notably, the patient’s anti-cyclic citrullinated peptide antibody (Anti-CCP Ab) was highly positive (>500 U/ml), leading to a definite diagnosis of rheumatoid arthritis (RA) based on the 2010 ACR/EULAR criteria. Management involved diuretics, parenteral albumin, ACE inhibitors, steroids, anticoagulants, and septran prophylaxis. A percutaneous renal biopsy [Figure 1] confirmed MN, anti-PLA2R antibody was negative, and subsequent treatment with the anti-CD20 monoclonal antibody Rituximab was initiated. Conventional disease-modifying antirheumatic drugs (DMARDs) such as Methotrexate and Hydroxychloroquine were prescribed for RA.
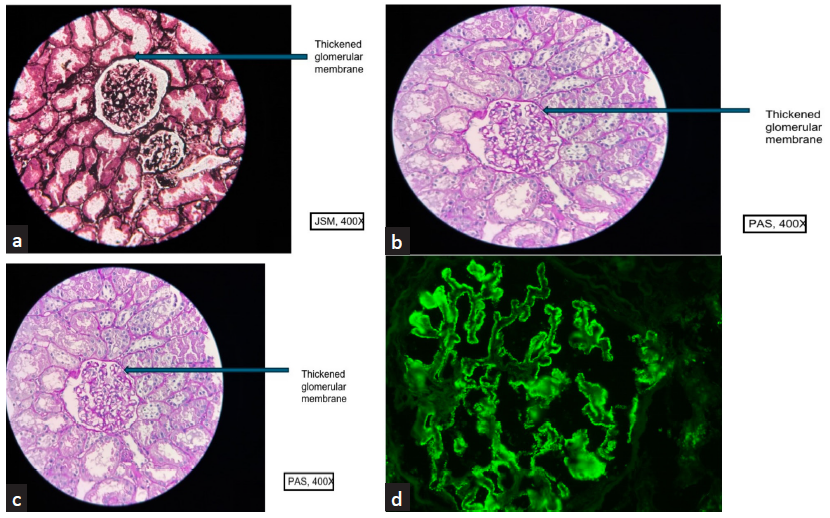
- (a and b) show thickening and stiffening of the glomerular capillary loop (400x, PAS and 400x JSM). (c) shows in addition to the thickened loops, there were pockets of lymphomononuclear inflammatory cell infiltrate in the cortical parenchyma and chronic mild inflammation (400x, PAS). (d) Direct immunofluorescence showed coarse granular deposits for anti sera specific against IgG (3+), Kappa (3+), Lambda (3+), C3 (1+) in the sub epithelial aspect of glomerular capillary loop. Rest of the panel IgA, IgM, C1q was negative, PAS: periodic acid schiff.
The patient responded well to the treatment (Rituximab and Methotrexate, Hydroxychloroquine), experiencing resolution of anasarca and albuminuria. Ongoing follow-up revealed sustained remission for both MN and RA.
MN is a significant cause of nephrotic syndrome in adults, comprising about 30% of cases, with 80% being primary (pMN) and 20% secondary (sMN).1 While the patient’s history and workup excluded causes of pMN, sMN, the positive response to RA treatment indicated a rare case of MN secondary to RA.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Reference
- Primary membranous nephropathy. Clin J Am Soc Nephrol. 2017;12:983-97.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]






