Translate this page into:
Metachromatic Leukodystrophy and Infantile Onset Nephrotic Syndrome: A Rare Confluence
Corresponding author: Nitish Kumar, Department of Pediatrics, Rani Hospital, Ranchi, Jharkhand, India. E-mail: doctornitishkumar@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kumar N, Kumar R, Kumar PR. Metachromatic Leukodystrophy and Infantile Onset Nephrotic Syndrome: A Rare Confluence. Indian J Nephrol. doi: 10.25259/IJN_52_2025
Dear Editor,
More than 58 monogenic variants have been associated with steroid-resistant nephrotic syndrome (SRNS).1 This is a novel case of SRNS linked to PKHD1 and ARSA variations.
A 2-year-old male presented with persistent generalized swelling for 3 months and regression of developmental milestones at one year of age. The child was born to non-consanguineous parents and had severe acute malnutrition along with nephrotic-range proteinuria. Six weeks of daily steroids showed no remission. Sanger sequencing confirmed heterozygous variants on exons 66 and 2 of PKHD1 and ARSA genes, respectively [Figure 1]. It is difficult to attribute causality between our findings and the clinical presentation. No abnormalities were found in auditory, ophthalmologic, or family screening. The child was prescribed tacrolimus and ACE inhibitor and is in complete remission with height and weight gain after 4 months.
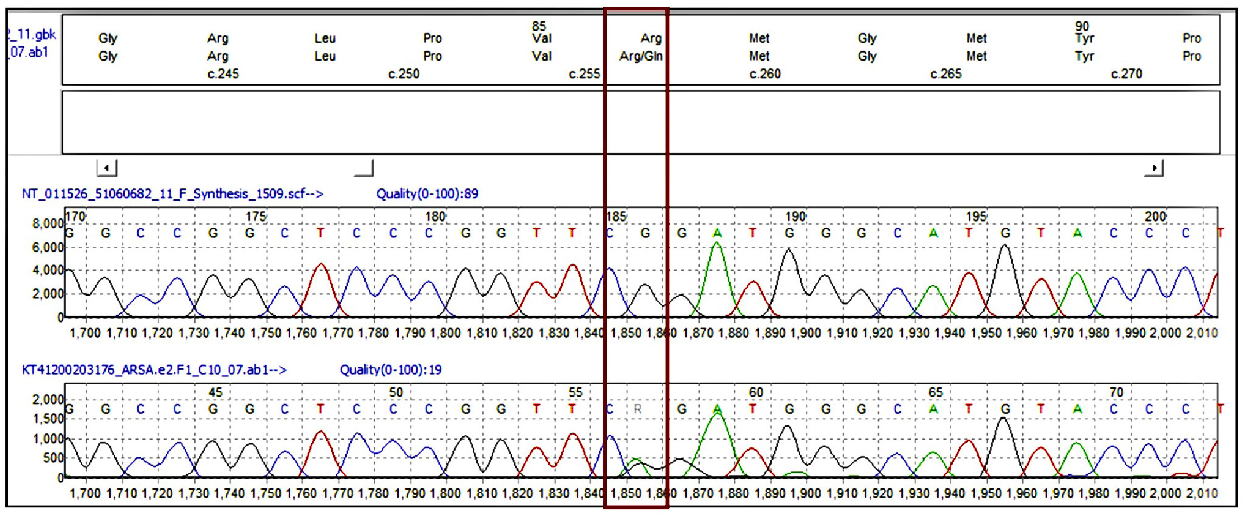
- Sanger sequencing data (electropherogram) showing nucleotide change at chr22: c.257G>A, (p.Arg86GIn) in the ARSA gene. Red, green, black, and blue color peaks show thymine, adenine, guanine, and cytosine bases, respectively. The red box highlights the specific nucleotide change at chromosome 22: c.257G>A, which results in the amino acid substitution p.Arg86Gln in the ARSA gene.
Metachromatic leukodystrophy (MLD) caused by ARSA mutations, is a lysosomal storage disorder characterized by sulfatide accumulation. Although rare, sulfatide deposition in glomerular podocytes can disrupt filtration and protein homeostasis.2 Podocytes, highly sensitive to lysosomal dysfunction, may exhibit structural and functional impairments in SRNS. Data on renal involvement in MLD remains limited with previous reports including two MLD cases with renal tubular acidosis (proximal in 1978, distal in 2024).3,4
This case expands MLD’s phenotypic spectrum, linking it to SRNS and highlighting the role of advanced genetic diagnostics in rare etiologies. It underscores the need for further research into the pathophysiological mechanisms linking MLD and renal dysfunction.
Acknowledgement
We thank all staff involved in the care of this patient.
Conflicts of interest
There are no conflicts of interest.
References
- Mutations in KIRREL1, a slit diaphragm component, cause steroid-resistant nephrotic syndrome. Kidney Int. 2019;96:883-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Podocyte pathology and nephropathy–sphingolipids in glomerular diseases. Front Endocrinol. 2014;5:127.
- [Google Scholar]
- Proximal renal tubular acidosis in metachromatic leukodystrophy. Helv Paediatr Acta. 1978;33:45-52.
- [PubMed] [Google Scholar]
- A rare clinical confluence: Metachromatic leukodystrophy and distal renal tubular acidosis. Indian J Nephrol. 2025;35:115.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]







