Translate this page into:
Methemoglobinemia due to quinine causing severe acute kidney injury in a child
Address for correspondence: Dr. Sidharth Kumar Sethi, Kidney and Urology Institute, Gurgaon - 122 001, Haryana, India. E-mail: sidsdoc@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Congenital methemoglobinemia is a rare condition resulting from a deficiency of nicotinamide adenine dinucleotide-cytochrome b5 reductase. Acquired methemoglobinemia may result due to certain drugs, chemicals and food items. Information on epidemiological determinants from India is sparse. This report describes methemoglobinemia in a 4-year-old child after parenteral administration of quinine causing acute kidney injury. This case emphasizes the need of awareness of potential adverse events of antimalarial drugs. Prompt management of methemoglobinemia is essential to avoid potential life-threatening complications.
Keywords
Acute kidney injury
methemoglobinemia
quinine
Introduction
Under normal conditions, iron molecule in haem is present in the ferrous state. Ferrous form is essentially needed for its oxygen transportation function. Under certain conditions, there is a loss of electron and formation of ferric molecule, which in turn results in formation of methemoglobin. In healthy individuals too, there is a small proportion of methemoglobin (2-3%).[1] Methemoglobin cannot bind with oxygen.[12]
This disorder is typically seen in three settings: endemic methemoglobinemia; in individuals of consanguineous unions; or in compound heterozygous cytochrome b5 reductase deficiency, which is primarily seen in sporadic cases.[2] In hereditary form, there is a deficiency of enzyme-cytochrome b5 reductase (deficiency of reduced nicotinamide adenine dinucleotide [NADH]). In normal individuals, cytochrome b5 receives an electron from NADH. This reaction needs enzyme cytochrome b5 reductase. It leads to a reduction of iron to the ferrous form. In the deficiency of this enzyme, methemoglobin cannot be converted back to normal haem.[3]
Acquired methemoglobinemia is known to occur due to reduction of hemoglobin to methemoglobin and is commoner than the congenital variety. It may occur due to drugs such as benzocaine, lidocaine, flutamide, dapsone, nitrites, phenazopyridine, amiodarone, amyl nitrite, primaquine, chloroquine, quinones, sulfonamides acetaminophen, hydrogen peroxide, disulfiram, ibuprofen, and metoclopramide.[456789] This may be due to aniline ring observed in drugs such as acetaminophen and sulfa drugs. Chemicals such as aniline dyes,[10] gasoline,[4] and food items, for example, spinach can produce similar reactions.
Information on epidemiological determinants from India is sparse. Cases have been reported from Karnataka in infants <6 months old due to high nitrite content in drinking water and a case from North India in a child who worked with malaria, in aniline dye factory.[1112] This article describes methemoglobinemia in a child after parenteral administration of quinine-an anti-malarial drug, causing a severe acute kidney injury (AKI) in a young child.
Case Report
A 4-year-old male child hailing from North India, and born out of nonconsanguineous marriage presented to emergency with chief complaints of high grade fever with chills and rigors since 8 days, vomiting since 3 days, and dark red colored urine since last 2 days. Prior to hospitalization, the child was treated in a private clinic where injection quinine was given for suspected malaria (though there was no laboratory evidence of malaria). There was no history of blood in the stool or vomitus. Past medical history and family history was insignificant.
On examination, child was conscious, alert, febrile (temperature 101°F), pulse was 120/min, respiratory rate was 34/min, and blood pressure was 122/94 mm Hg. Pallor was present. There was no evidence of icterus, edema, cyanosis, clubbing, and lymphadenopathy. Anthropometry was normal for age (WHO standards). Systemic examination was within normal limits.
Complete blood count showed hemoglobin 8.2 g/dl, hematocrit 33.1%, platelet count 405 × 103/μl with methemoglobinemia (9.6%). There was elevated total leucocytes count (26,000). Pulse oximetry showed oxygen saturation of 80% with an arterial pO2334 mm Hg, with a chocolate brown blood on exposed to air. Renal functions were deranged with blood urea 183 mg/dl; serum creatinine level 4.4 mg/dl. There was evidence of hepatic dysfunction (serum bilirubin 4.2 mg/dl; serum glutamic oxaloacetic transaminase 694 U/L, serum glutamate pyruvic transaminase 113 U/L). Serum level of lactate dehydrogensase was 1200 IU/L. Hemoglobin electrophoresis showed no hemoglobinopathies. Direct Coomb's test was found to be negative. Tests for malaria, dengue, and leptospirosis were negative. His blood was negative for Heinz bodies, and there was no glucose-6-phosphatase deficiency. All the cultures were found to be sterile. Urine was dark colored, no RBCs on light microscopy, haem positive.
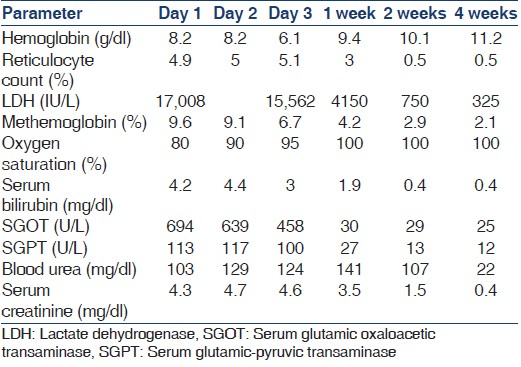
Diagnosis of methemoglobinemia with AKI was made after assessment. During admission, the child received supportive packed red blood cells, amlodipine for hypertension and antihyperkalemic measures. He remained nonoliguric during the course and hematuria was resolved. Patient's vital signs remained stable. Dialysis was not required during the course. Oxygen saturation returned to normal. Methylene blue was not required to be given in this patient. Methemoglobin level gradually decreased, and at a time of discharge its level was 2.9% [Table 1]. Patient continued to improve until the day of his discharge.
At the time of last follow-up, 2 months after discharge, the child has normal renal and hepatic functions with a serum creatinine of 0.6 mg/dl.
Discussion
Clues that methemoglobinemia is present include the development of cyanosis in the presence of a normal arterial pO2or the presence of “chocolate brown blood” in the videoscopic field.[23] In acquired methemoglobinema, level of cytochrome b5 reductase is found to be normal. Concentration of methemoglobin is elevated. Co-oximetry can be used for confirmation of diagnosis.[234]
Prognosis is very good once the causative agent is removed. This stops the ongoing formation of methemoglobin. In lesser degrees of methemoglobinemia (i.e., an asymptomatic patient with a methemoglobin level <20%), no therapy other than discontinuation of the offending agent (s) may be required. If the patient is symptomatic, or if the methemoglobin level is >20%, which is often the case in deliberate or accidental overdoses or toxin ingestion, specific therapy with methylene blue is indicated.[13] We did not give methylene blue in our case, since he was improving on removing the offending quinine.
Quinine has a wide range of adverse events including mild events such as tinnitus, dizziness, disorientation, nausea, hypoglycemia, visual changes, and auditory deficits to life-threatening complications such as renal failures, cardiac arrhythmias, and black water fever. There have been very few publications, which mention hemolysis and severe methemoglobinemia due to quinine.[141516]
We still cannot rule out an underlying genetic etiology in this child, as a risk factor for acute acquired methemoglobinemia is the asymptomatic heterozygous state for cytochrome b5 reductase deficiency. The classic description of acute toxic methemoglobinemia in United States military personnel receiving malarial prophylaxis in Vietnam demonstrated for the first time that heterozygotes for this autosomal recessive disease can, under certain conditions, develop a disease state that is more clinically significant than their asymptomatic homozygous peers.[17]
This is the first case in a young child, with a severe form of AKI following quinine ingestion and acquired methemoglobinemia. This is a learning case emphasizing greater awareness of potential adverse events of antimalarial drugs; especially in the pediatric population.
Source of Support: Nil
Conflict of Interest: None declared.
References
- A comparision of the effect of menadione, methylene blue and ascorbic acid on the reduction of methemoglobin in vivo. Nature. 1964;202:607-8.
- [Google Scholar]
- Dyshemoglobinemias. In: Steinberg M, ed. Disorders of Hemoglobin: Genetics, Pathophysiology, and Clinical Management (2nd ed). Cambridge: Cambridge University Press; 2009. p. :607.
- [Google Scholar]
- Congenital methemoglobinemia with a deficiency of cytochrome b5. N Engl J Med. 1986;314:757-61.
- [Google Scholar]
- Acquired methemoglobinemia following benzocaine anesthesia of the pharynx. Am J Crit Care. 2000;9:199-201.
- [Google Scholar]
- Methemoglobinemia from hydrogen peroxide in a patient with acatalasemia. Anesthesiology. 2004;101:247-8.
- [Google Scholar]
- Toxic methemoglobinemia due to Ibuprofen: Report of a pediatric case. J Emerg Med. 2010;39:216-7.
- [Google Scholar]
- Metoclopramide-induced methemoglobinemia in a patient with co-existing deficiency of glucose-6-phosphate dehydrogenase and NADH-cytochrome b5 reductase: Failure of methylene blue treatment. Haematologica. 2001;86:659-60.
- [Google Scholar]
- Acquired methemoglobinemia and hemolytic anemia following excessive pyridium (phenazopyridine hydrochloride) ingestion. Clin Pediatr (Phila). 1971;10:537-40.
- [Google Scholar]
- The blue baby syndrome: Nitrate poisoning in infants. Humanit Soc Sci Law. 2003;8:20-30.
- [Google Scholar]
- Death in an adolescent girl with methemoglobinemia and malaria. J Trop Pediatr. 2012;58:154-6.
- [Google Scholar]
- Treatment of nitrite-induced methemoglobinemia with hyperbaric oxygen. Proc Soc Exp Biol Med. 1971;138:137-9.
- [Google Scholar]
- Clinical features and management of poisoning due to antimalarial drugs. Med Toxicol Adverse Drug Exp. 1987;2:242-73.
- [Google Scholar]
- Methaemoglobin levels in soldiers receiving antimalarial drugs. Med J Aust. 1971;1:473-5.
- [Google Scholar]
- Methemoglobinemia provoked by malarial chemoprophylaxis in Vietnam. N Engl J Med. 1968;279:1127-31.
- [Google Scholar]







