Translate this page into:
Monascus purpureus Went rice in nephrotic hyperlipidemia
Address for correspondence: Dr. Osama Gheith, Consultant of Nephrology, Urology and Nephrology Center, Mansoura University, Mansoura, Egypt. E-mail: ogheith@yahoo.com
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Nephrotic dyslipidemia is a risk factor for the development of systemic atherosclerosis; and may aggravate glomerulosclerosis and enhance progression of glomerular disease. We aimed to assess the efficacy and safety of Monascus purpureus Went rice vs. fluvastatin therapy in the management of nephrotic dyslipidemia.
Materials and Methods:
Seventy-two patients with persistent idiopathic nephrotic syndrome (NS) with secondary dyslipidemia were included. They were randomly allocated into three age and sex-matched groups. The first group comprised 20 cases and were given M. purpureus Went rice in a dose of 600 mg twice/day for 1 month then once daily, the second group comprised 30 cases were given fluvastatin in a daily dose of 20 mg. The remaining 22 received no antidyslipidemic therapy and constituted a control group. All of these patients were subjected to thorough laboratory investigations including renal function tests and lipogram. Moreover, the neuromuscular status was evaluated with electromyography and nerve conduction velocity.
Results:
Our results showed that both fluvstatin and M. purpureus Went rice were well tolerated with no evidence of significant side effects including neuromuscular functions. Both of them significantly reduced cholesterol after 6 months and 1 year.
Conclusion:
Monascus purpureus Went rice is safe, effective, and economic treatment strategy for nephrotic dyslipidemia.
Keywords
Glomerulonephritis
Monascus purpureus
nephrotic syndrome
neurotoxicity
statin
Introduction
Nephrotic hyperlipidemia is a risk factor for the development of systemic artherosclerosis, and may aggravate glomerulosclerosis and enhance the progression of glomerular disease.1
Diet intervention should be the first-line of treatment, but it only partially corrects hypercholesterolemia in such patients.2 The greatest and the most consistent reductions in low-density lipoprotein (LDL)-cholesterol is seen with 3-hydroxy-3-methylglutaryl-coenzyme A reductase (HMG-CoA reductase) inhibitors. Many studies have shown that M. purpureus Went rice contained HMG-CoA reductase inhibitors, large quantities of unsaturated fatty acids, beta-sitosterol, campesterol, and stigmasterol.3–5 These components are effective in reducing serum lipid.6
The lipid-lowering effects of M. purpureus - rice food flavor in China and Japan - have been shown in several animal models of hyperlipidemia.7 One study showed that M. purpureus Went rice significantly reduced LDL-C, total cholesterol, triglycerides, and apolipoprotein B levels, and was well tolerated in patients with hyperlipidemia.89
However, the long-term safety and efficacy of these lipid-lowering strategies are lacking in patients with renal disease.10 Treatments of nephrotic dyslipidemia in steroid resistant NS have resulted in a considerable benefit not only for the hyperlipidemia, but also for the nephrotic state.11
Prospective controlled studies are needed to evaluate the long-term safety of statins in a large patient population and assess whether reduction in cholesterol decreases the risk for atherosclerosis and inhibits the progression of glomerular disease in patients with NS.12 Although statin therapy was considered to be safe in treating nephrotic dyslipidemia on the short-term follow-up studies considering electromyography (EMG),1213 long-term studies are lacking for this costly regimen.
We aimed to assess the efficacy and safety of M. purpureus Went rice vs. fluvastatin therapy in the management of nephrotic dyslipidemia.
Materials and Methods
Out of 450 patients with idiopathic nephrotic syndrome screened, 72 were recruited from the nephrology clinic of the Urology and Nephrology Center, Mansoura University for inclusion in this prospective, randomized controlled study for a planned duration of 1 year.
The patients were recruited with the following inclusion criteria: steroid resistant, steroid dependent, and frequently relapsing idiopathic nephrotic syndrome, hypercholesterolemia with no response to an appropriate diet for at least 4 weeks, serum creatinine < 2 mg/dl, recent renal biopsy proved focal segmental glomerulosclerosis (FSGS) or membranoproliferative glomerulonephritis (MPGN). We excluded patients with hepatic disease, muscle disease, history of familial dyslipidemia, diabetes mellitus and those on statins.
This protocol met the requirements of local ethical committee. Upon enrollment, patients were randomly assigned to one of the three treatment groups. The first group comprised 20 cases and was given M. purpureus, the second group comprising of 30 cases was given fluvastatin, and the third group (n=22) served as control.
Information regarding the randomized treatment was concealed in sequentially numbered, sealed opaque envelopes. These were opened in the absence of the patients immediately after obtaining informed written consent for participation in the study. The participant physicians were necessarily aware of the randomized treatment in all cases.
Patients were evaluated at start of treatment (control values) and monthly for 6 months (test values). The evaluation included thorough history taking and clinical examination, and following laboratory investigations: Complete urine analysis and 24-h urinary protein estimation, serum creatinine and creatinine clearance using Cockcroft and Gault formula; liver function tests; investigations to exclude secondary causes of glomerulonephritis such as blood sugar, anti-HCV, anti-CMV, anti-HIV, HbsAg, serologic tests for systemic lupus erythematosis rectal mucosal biopsy to exclude schistosomiasis; and total serum cholesterol.
Neurophysiological evaluation was done using the NIHON KOHDEN-evoked response recorder, model MEP-5200, for EMG14 and nerve conduction velocity.15
Electromyography
The following muscles were tested:
The biceps brachii and the rectus femoris as representative of the proximal muscles of the upper and lower limbs, respectively.
The abductor pollicis brevis of the thenar eminence and extensor digitorum brevis as representative of the distal muscles of the upper and lower limbs, respectively.
The electrical potentials were recorded by a bipolar EMG needle electrode (NW-120T). Resting and mild contraction activities were recorded at the interrupted speed and the interference pattern at continuous speed for each muscle.
The mean of at least 20 motor unit action potentials (MUPs), from different sites and depths, gave the duration and amplitude.
Nerve Conduction velocity
We chose the median nerve and the lateral popliteal nerve for estimating the conduction velocity. The median nerve was stimulated at the antecubital fossa and at the wrist, while the lateral popliteal nerve was simulated at the knee and ankle joints. A bipolar stimulating surface electrode (A-NM-4205) was applied over the nerve and the evoked potentials were recorded by a needle electrode from the abductor pollicis brevis in the upper limb and extensor digitorum brevis in the lower limb. The duration of the stimulus pulse was usually 0.5 ms and the stimulus voltage increased from zero to supramaximal to get the best M wave. A ground electrode was placed between the stimulating and the recording electrodes. Depending on the latency and duration of the evoked potentials, the time bases of the recordings were varied so that the whole pattern of potentials could be displayed on the sweep of the oscilloscope. Usually a time base of 10 ms/cm was needed.
The latency was measured from the start of the stimulus artifact to the onset of the muscle response. The same process was repeated twice, once at the proximal part of the nerve and the other at the distal part. The time difference between the two latencies in milliseconds was obtained.
The conduction velocity was calculated as follows:
Cv = Distance between the two points of stimulation in cm × 10.
Difference between the two latencies in milliseconds = m/sec (meters per second).
The first group received M. purpureus Went rice (600 mg twice/day for 1 month then once daily). The second group received oral fluvastatin in a daily dose of 20 mg. The third group received no additional therapy and ranked as a control. After 8 weeks, re-adjustment of the dose was performed according to patient's response (serum cholesterol) and patient's tolerance to the drug. Restriction of dietary cholesterol and proteins was illustrated to every patient by appropriate counseling and repeated reinforcement. Other supportive treatment including angiotensin converting enzyme inhibitor (ACEI) use was comparable in the two groups.
All patients were followed monthly for one year after which they were subjected to thorough clinical and laboratory evaluation.
Statistical analysis was done by an IBM compatible personal computer using the Statistical Package for Social scientists (SPSS) for windows 11.5 (SPSS Inc., Chicago, IL, USA). Qualitative data were displayed in cross tabulation and quantitative data were described in terms of arithmetic mean ± SD. A P-value of <0.05 was considered significant.
Results
The demographic characteristics of all patients were summarized in Table 1. There was no significant difference between the studied groups regarding patients' age, sex, body weight, smoking history, and renal histopathology.
| Fluvastatin (N = 30) | Control (N = 22) | Monascus purpureus (N = 20) | P value | |
|---|---|---|---|---|
| Mean age (Y) | 17.6 ± 7 | 19.7 ± 7 | 21.4 ± 14 | 0.19 |
| Sex (male/female) | 13/17 | 10/12 | 12/8 | 0.38 |
| Smokers | 3/27 | 4/18 | 3/17 | 0.92 |
| Occupation | ||||
| Student | 13 | 9 | 6 | 0.51 |
| Worker | 5 | 3 | 4 | 0.94 |
| Professional | 12 | 10 | 10 | 0.68 |
| Body weight | 51.3 ± 26 | 58.2 ± 25 | 55.2 ± 24 | 0.4 |
| Renal pathology | ||||
| FSGS | 24 | 14 | 18 | 0.58 |
| MPGN | 6 | 8 | 2 |
Fig. 1 shows the serial value of serum cholesterol in different study groups.
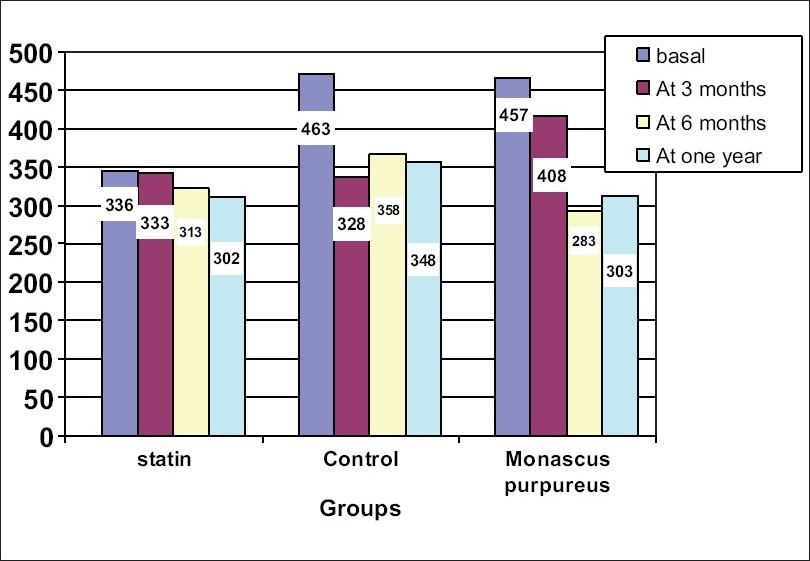
- Showed serum cholesterol levels in different groups along follow-up period
In comparison to baseline values, fluvastatin produced a significant and progressive reduction of serum cholesterol by 35, 38, and 42% at 3 months, 6 months, and after 1 year, respectively (P < 0.001). Similar reductions were observed in the M. purpureus Went rice group. After 1 year, we observed that serum cholesterol was significantly lower in statin and M. purpureus Went rice groups compared to the control group (P = 0.003) [Table 2].
| Statin (N = 30) | Control (N = 22) | Monascus purpureus (N = 20) | P value, Control vs Other groups | |
|---|---|---|---|---|
| Serum CR(mg/dl) | ||||
| Basal | 1.07 ± 0.4 | 1.2 ± 0.3 | 0.85 ± 0.3 | 0.06 |
| At 6 months | 1.03 ± 0.8 | 0.9 ± 0.6 | 0.98 ± 0.5 | 0.53 |
| At 1 year | 1.2 ± 0.8 | 0.99 ± 0.5 | 0.96 ± 0.3 | 0.62 |
| S. albumin (gm/dl) | ||||
| Basal | 1.6 ± 0.7 | 1.3 ± 0.3 | 1.67 ± 0.7 | 0.06 |
| At 6 months | 2.1 ± 0.9 | 1.7 ± 0.8 | 2.09 ± 1.2 | 0.56 |
| At 1 year | 2.3 ± 0.9 | 1.7 ± 0.8 | 2.5 ± 1.6 | 0.05 |
| Proteinuria (gm/day) | ||||
| Basal | 8.3 | 8.8 | 8.6 | 0.06 |
| At 6 months | 5.2 | 6.6 | 5.5 | 0.055 |
| At 1 year | 2.4 | 7 | 3.2 | 0.04 |
| Serum ALT (IU/L) | ||||
| Basal | 16 ± 9 | 19 ± 8 | 15 ± 6 | 0.5 |
| At 1 year | 15 ± 5 | 17 ± 4.5 | 17 ± 4 | 0.9 |
| S. cholesterol (mg/dl) | ||||
| Basal | 436 ± 102 | 463 ± 169 | 457 ± 232 | 0.31 |
| At 3 months | 333 ± 155 | 328 ± 158 | 408 ± 239 | 0.55 |
| At 6 months | 313 ± 185 | 358 ± 178 | 283 ± 208 | 0.31 |
| At 1 year | 302 ± 171 | 348 ± 184 | 303 ± 178 | 0.003 |
Serum albumin increased significantly in the statin, M. purpureus Went rice groups at 12 months compared to the control group and to the basal values (P = 0.05) [Table 2].
In our series, blood chemistry including liver enzymes, bilirubin, alkaline phosphatase, and creatine phosphokinase (CPK) were within normal ranges throughout the study. The mean of CPK showed no significant difference at the start of treatment, after 3 months and at the end of the study.
We observed no clinical evidence of myopathy or neuropathy in our patients who received statins or M. purpureus Went rice therapies compared to the basal evaluation.
The amplitude of the MUPs showed no significant changes in the distal muscles after 12 months of fluvastatin or M. purpureus Went rice therapies. On the other hand, there was a significant reduction in duration and amplitude of motor action potentials of proximal muscles. However, polyphasicity showed no significant change (P > 0.05) [Table 3]. Nerve conduction velocity and terminal latency of the median and lateral popliteal nerves showed no significant changes at 6 months compared to basal values (P > 0.05).
| Fluvastatin (N = 30) | Monascus purpureus (N = 20) | P value | |
|---|---|---|---|
| Amplitude (mv) | Amplitude (mv) | ||
| AMP biceps brachii | |||
| Basal | 1487 ± 1510 | 4250 ± 2500 | 0.031 |
| Last | 1257 ± 1075 | 3078 ± 1500 | 0.030 |
| P within groups | 0.078 | 0.078 | |
| AMP Q femoris | |||
| Basal | 1813 ± 900 | 3971 ± 2030 | 0.075 |
| Last | 1245 ± 840 | 4100 ± 2300 | 0.025 |
| P within groups | 0.075 | 0.075 |
Discussion
Hyperlipidemia of the nephrotic syndrome is a risk factor for the development of systemic artherosclerosis, also it may aggravate glomerulosclerosis and enhance the progression of glomerular disease.127
Pattern of dyslipidemia in our cases is matching with that reported by Wheeler16 and Warwick et al.17 who showed that total plasma cholesterol; TG, VLDL, and LDL were elevated, with variable HDL concentration.
We observed significant reduction of serum cholesterol by 28.8% and 30.2% at 6 months and at 1 year of M. purpureus Went rice, possibly due to its HMG-CoA reductase inhibiting properties.3–5 In contrast, there were no significant changes in serum cholesterol in the control group.
Similar findings were reported by Matzkies et al.18 who showed a reduction of total cholesterol by 31% and LDL by 29% after 2 months of initiation of fluvastatin treatment (40 mg/day). The relatively small number of cases (10 cases) as well as the large dosage of fluvastatin they used might explain the earlier reduction in LDL and cholesterol they observed. Also, our observation goes hand in hand with the degree of reduction in total and LDL cholesterol reported by Olbricht et al.19 on using simvastatin with nephrotic patients. Todd and Goa20 achieved a 25-30% reduction in plasma LDL within 4 weeks which was maintained with continued treatment by a daily dose of 20-40 mg fluvastatin. Jokubaitis21 reported similar findings by fluvastatin in a dose of 40 mg/day.
In this study, we succeeded in reducing cholesterol by the same degree after 6 months of fluvastatin (20 mg per day) and - for the first time in nephrotic patients - by M. purpureus (600 mg per day) therapies, without side effects and with relatively lower dosage.
In the same direction, Lin et al.8 reported short-term efficacy and safety of M. purpureus went rice in treating hyperlipidemia.
Interestingly, a significant reduction in proteinuria was observed in the statin and M. Went rice treated patients, but not in the control group. Matzkies et al.18 in a similar study - with statin failed to demonstrate such favorable effect. This may be explained by the fact that Matzkies' patients were of heterogeneous pathologic types while most of our patients were suffering from FSGS.
In the same direction, Hattori et al.22 reported that there was an improvement in renal function and proteinuria in drug resistant NS secondary to FSGS, by LDL apheresis combined with pravastatin. In placebo-controlled study performed in Hong-Kong over 2 years, it was suggested that despite no significant effect on proteinuria a decline in renal function was attenuated by lovastatin, particularly over the second year of the study.23 Chan et al.24 reported that in lovastatin-treated nephrotics with relatively good pretreatment renal function, glomerular filtration rate (GFR) increased at the end of 6 months treatment.
In contrast, Matzkies et al.18 reported a significant rise in serum creatinine in their patients despite using fluvastatin in a dose of 40 mg/day. Again, the heterogeneity of pathologic types of their patients explains the difference in their results.
In this study, the significant reduction of creatinine clearance among control group 6 months onward compared to the nonsignificant change of creatinine clearance in M. purpureus Went rice and statin-treated groups, both suggested the protective effect of lipid-lowering agents on kidney function. Also, the electromyographic data showed a significant decrease in the amplitude and duration of MUP in the proximal muscles only with statin treatment compared to basal values. These changes were not observed in M. purpureus. However, this reduction was not excessive and there was no other electromyographic evidence of myopathy. In addition, there were no clinical findings of myopathy or elevated serum CPK.
Peters25 similarly noted that drug-related myopathy and rhabdomyolysis have not been reported with fluvastatin on the basis only of clinical findings and elevated skeletal muscle enzymes. In the same direction, Jokubaitis21 found no notable increase in serum CPK or liver enzymes, and no cases of clinically evident myopathy. On the other hand, Careless and Cohen26 reported that statins and fibrates were associated with a variety of rheumatic problems including proximal myopathy, diagnosed on a clinical basis and confirmed by high serum CPK. Jacquet et al.27 also reported that the frequency of severe side effects such as myopathy amounted to 1 per 1000 prescriptions with cholesterol-lowering drugs in current use. De Pinieux et al. ascribed the myopathic side effects of statins to mitochondrial dysfunction as the blood lactate/pyruvate ratio is high.28 These reports regarding the safety of statins were based only on clinical data and muscle enzyme evaluation.
Jacobson et al.29 reported increase in liver enzymes while Olbricht et al.19 and Matzkies et al.18 reported satisfactory tolerance of statin in their nephrotics.
In agreement with what was reported by Lin et al.8, M. purpureus Went rice was well tolerated in patients with hyperlipidemia. Moreover, we found that M. purpureus Went rice was not only an efficacious modality of treatment that targeted the nephrotic dyslipidemia with the same potency like statin, but also achieved 50% cost reduction in comparison to fluvastatin. From this study, we can conclude that M. purpureus Went rice is safe, effective, and economic treatment strategy for nephrotic dyslipidemia.
The authors would like to thank Biopharma Co. for supplying Monascus purpureus Went rice in capsule form for one year to their patients.
Source of Support: Biopharma Co supplying Monascus purpureus
Conflict of Interest: None declared.
References
- Hyperlipidemia of the nephrotic syndrome - The search for a nephrotic factor. Nephrol Dial Transplant. 1995;10:314-6.
- [Google Scholar]
- Elevated plasma lipoprotein (a) in patients with the nephrotic syndrome. Ann Intern Med. 1993;119:263-9.
- [Google Scholar]
- Cholesterol-lowering effects of a proprietary Chinese red-yeast-rice dietary supplement. Am J Clin Nutr. 1999;69:231-6.
- [Google Scholar]
- Constituents of red yeast rice, a traditional Chinese food and medicine. J Agr Food Chem. 2000;48:5220-5.
- [Google Scholar]
- Multicenter clinical trial of the serum lipid-lowering effects of a Monascus purpureus Went rice (red yeast) rice preparation from traditional Chinese medicine. Curr Ther Res. 1997;58:964-78.
- [Google Scholar]
- Effects of dietary phytosterols on cholesterol metabolism and atherosclerosis. Am J Med. 2000;109:72-3.
- [Google Scholar]
- Hypolipidemic and anti-atherogenic effects of long-term Cholestin (Monascus purpureus-fermented rice, red yeast rice) in cholesterol fed rabbits. J Nutr Biochem. 2003;14:314-8.
- [Google Scholar]
- Efficacy and safety of Monascus purpureus Went rice Went rice in subjects with hyperlipidemia. Eur J Endocrinol. 2005;153:679-86.
- [Google Scholar]
- Efficacy of Monascus purpureus Went rice on lowering lipid ratios in hypercholesterolemic patients. Eur J Cardiovasc Prev Rehabil. 2007;4:438-40.
- [Google Scholar]
- Lipid abnormalities in the nephrotic syndrome: The therapeutic role of statins. J Nephrol. 2001;14:S70-5.
- [Google Scholar]
- Neuromuscular toxicity in nephrotic patients treated with fluvastatin. J Nephrol. 2002;15:690-5.
- [Google Scholar]
- Impact of treatment of dyslipidemia on renal function, fat deposits and scarring in patients with persistent nephrotic syndrome. Nephon. 2002;91:612-9.
- [Google Scholar]
- Clinical electromyography. In: Aminoff MJ, ed. Electrodiagnosis in clinical neurology (3rd ed). New York/Edinburgh/London/ Melborne/ Tokyo: Churchul Livingstone; 1992. p. :249.
- [Google Scholar]
- Nerve conduction studies. In: Aminoff MJ, ed. Electrodiagnosis in clinical neurology (3rd ed). New York/ Edinburgh/ London/ Melborne/ Tokyo: Churchul Livingstone; 1992. p. :283.
- [Google Scholar]
- Lipids - What is the evidence for their role in progressive renal disease. Nephrol Dial Transplant. 1995;10:14-6.
- [Google Scholar]
- Low-density lipoprotein metabolism in the nephrotic syndrome. Metabolism. 1990;39:187-92.
- [Google Scholar]
- Efficiency of 1-year treatment with fluvastatin in hyperlipidemic patients with nephrotic syndrome. Am J Nephrol. 1999;19:492-4.
- [Google Scholar]
- Treatment of hyperlipidemia in nephrotic syndrome: Time for a change? Nephron. 1992;62:125-9.
- [Google Scholar]
- Fluvastatin in combination with other lipid-lowering agents. Br J Clin Pract Symp Suppl Am. 1996;77:28-32.
- [Google Scholar]
- Treatment with a combination of low-density lipoprotein aphaeresis and pravastatin of a patient with drug resistant nephrotic syndrome due to focal segmental glomerulosclerosis. Pediatr Nephrol. 1993;7:196-8.
- [Google Scholar]
- Lovastatin in glomerulonephritis patients with hyperlipidemia and heavy proteinuria. Nephrol Dial Transplant. 1992;7:93-9.
- [Google Scholar]
- Cholesterol-lowering therapy may retard the progression of diabetic nephropathy. Diabetologia. 1995;38:604-9.
- [Google Scholar]
- Rheumatic manifestations of hyperlipidemia and antihyperlipidemic drug therapy. Semin Arthritis Rheum. 1993;23:90-8.
- [Google Scholar]
- A one year prospective and intensive pharmacovigilance of antilipemic drugs in hospital consultation for prevention of risk factors. Therapie. 1993;48:509-12.
- [Google Scholar]
- Lipid lowering drugs and mitochondrial function: Effect of HMG-COA reductase inhibitors on serum ubiquinone and blood lactate/pyrurate ratio. Br J Clin Pharmacol. 1996;42:333-7.
- [Google Scholar]
- Fluvastatin with and without niacin for hypercholesterolemia. Am J Cardiol. 1994;74:149-54.
- [Google Scholar]







