Translate this page into:
Myeloma Cast Nephropathy an Unusual Association with HIV Infection Presenting with Renal Dysfunction
Address for correspondence: Dr. Bheemanathi H. Srinivas, Department of Pathology, JIPMER, Puducherry - 605 006, India. E-mail: srinivas.bh@gmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Human immunodeficiency virus (HIV)-associated renal disease is a pan-nephropathy, causing glomerular, tubular, and interstitial changes. The common lesion is the collapsing variant of focal segmental glomerulosclerosis. Multiple myeloma presenting as light chain cast nephropathy in an HIV-positive patient is very rare. A 45-year-old female retropositive patient presented with one episode of hematuria. Kidney biopsy was performed with a clinical diagnosis of acute interstitial nephritis (AIN). Biopsy showed unremarkable glomeruli. Tubules were dilated and showed a few periodic acid–Schiff (PAS) positive and many PAS-negative fractured casts surrounded by histiocytic reaction. Immunofluorescence and immunohistochemistry (IHC) showed lambda restriction by the casts. Bone marrow aspirate showed an increase in plasma cells, and the biopsy showed nodular aggregates of atypical plasma cells, which showed lambda restriction by IHC. PAS-negative fractured tubular casts are known to be associated with HIV-related nephropathy and need detailed hematological workup to rule out an associated plasma cell dyscrasia.
Keywords
HIV
myeloma cast nephropathy
renal dysfunction
Introduction
Human immunodeficiency virus (HIV)-associated renal disease is a pan-nephropathy, causing glomerular, tubular, and interstitial changes. The glomerular lesion is the collapsing variant of focal segmental glomerulosclerosis;[12] the tubular abnormalities include cellular degeneration and necrosis as well as cystic dilatation, and the interstitium is edematous and often infiltrated by lymphocytes.[3] Myeloma-like cast nephropathy is known to occur in HIV patients, but they are polyclonal, which are precipitate of plasma proteins that characteristically fill the lumina of tubules in all segments of the nephron staining pale or negative with periodic acid–Schiff (PAS).[34] Multiple myeloma presenting as cast nephropathy in HIV-positive patients is very rare and has been sparsely described in the literature.
Case History
A 45-year-old female, retropositive patient presented with history of fever, vomiting, and diarrhea with fever for 6 months and history of one episode of hematuria. On examination, she was found to have pallor, no edema, and her blood pressure was 110/80 mm Hg. On investigation, she was found to have serum creatinine of 7 mg/dl. Urine albuminuria was 1+, with 1–2 RBC/HPF, and 5–6 pus cells/HPF. Hemoglobin was 8.2 g/dl, and total count was 5610/cmm with normal differential count and platelet count of 2,48,000/cmm. ESR was 150 mm Hg. Considering the clinical history of an HIV patient presenting with vomiting and diarrhea with an episode of hematuria, presence of WBC in urine, and rise in creatinine, kidney biopsy was performed with a clinical diagnosis of AIN. Biopsy showed unremarkable glomeruli. Tubules were dilated and showed a few PAS-positive and many PAS-negative fractured casts surrounded by histiocytic reaction [Figure 1]. Interstitium showed moderate infiltration by lymphocytes and plasma cells. Blood vessels were unremarkable. Immunofluorescence [Figure 2a, b] and IHC showed lambda restriction by the casts, thus correlating with light microscopy and IF, the possibility of myeloma cast nephropathy was suggested. Further bone marrow aspiration and biopsy were performed which confirmed the diagnosis of myeloma cast nephropathy. Bone marrow aspirate showed an increase in plasma cells, and the biopsy showed nodular aggregates of atypical plasma cells [Figure 2c, d], which showed lambda restriction by IHC. The patient was treated symptomatically and referred to medical oncology for myeloma treatment.

- Histopathology of kidney biopsy shows (a) dilatations of many tubules which are filled with casts. Glomerulus morphologically unremarkable (H&E × 100); (b) shows fractured casts with evidence of moderate degree of acute tubular necrosis (H&E × 200); (c) shows PAS negative tubular casts and occasional PAS-positive cast (PAS × 200); (d) Masson trichrome stain show fractured casts in violet color (MT × 200)
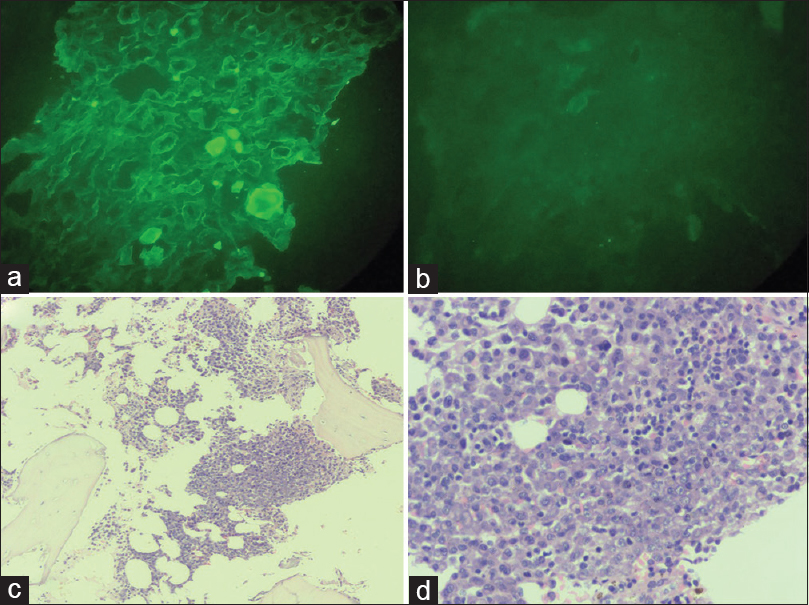
- (a and b) Immunofluorescence microscopy shows lambda chain restriction and Kappa chain negative in fractured tubular casts (Lambda and Kappa × 200); (c) Bone marrow biopsy nodular aggregates of plasma cells (H&E × 100); (d) Sheets of plasma cells admixed with scattered mature lymphocytes (H&E × 400)
Discussion
The incidence of plasma cell disorders in HIV-infected patients is increasing and can range from polyclonal hypergammaglobulinemia to aggressive multiple myeloma.[567] The possible mechanisms for the increasing frequency are attributed to antigen stimulation and immunodeficiency.[67] It is believed that HIV viral antigens or other antigens may act as super-antigens and stimulate the proliferation of B cells and the secretion of immunoglobulin without the help of T-cells.[6] Immunodeficiency due to HIV viruses can cause T-cell dysfunction, which may induce the activation of B-cells without the need for antigen stimulation.[7]
Though the incidence of plasma cell disorders is increasing among HIV-infected patients, renal diseases caused due to monoclonal proliferation are relatively sparse. The lesions of glomeruli in HIV patients are most typically, but not always, of the collapsing variant of focal segmental glomerulosclerosis.[1] Although FSGS is the predominant glomerular lesion in HIVAN, other reported glomerular lesions in patients with HIV include IgA nephropathy, cryoglobulinemia, amyloidosis, and a lupus-like immune complex glomerulopathy.[8]
About 60% of patients[8] with AIDS manifest with clinically significant kidney dysfunction due to acid-base or electrolyte disturbances or parenchymal damage. The lesions may be directly related to HIV infection of the kidney, some may be the result of immunologic responses to the virus, some may be indirect manifestations of viral infection not within the kidneys, still others evolve from the opportunistic infections and neoplasms that characterize AIDS, and others may be the consequences of various therapies or hemodynamic derangements.
Renal tubular and interstitial abnormalities include acute renal failure in 6%–30% of patients, often as the result of acute tubular necrosis, interstitial nephritis, or a combination of the two.[9] In a study by Zaidan et al.,[10] tubulointerstitial nephropathies accounted for 26.6% of renal diseases in HIV-infected patients which were due to drug toxicity, infection, and dysimmune syndromes. Tubular fractured casts in HIV-related nephropathy are mostly plasma proteins and are usually PAS-positive. PAS-negative casts are also described to be associated with HIVAN mimicking myeloma-like casts and are usually polyclonal.[34] Sheikh et al.[4] reported myeloma-like cast nephropathy in two HIV-positive patients which were polyclonal in nature.
In this case, the patient presented with vomiting and diarrhea with hematuria and increased creatinine; thus, the clinical possibility considered was acute tubular necrosis secondary to dehydration rather than HIVAN. Light microscopy showed casts, a few of which were PAS-positive; this could be due to dehydration as expected and a few were PAS-negative with fracture and histiocytic reaction resembling myeloma cast nephropathy, which also showed monoclonality by lambda restriction by IHC and IF. Further bone marrow study confirmed the diagnosis of light chain cast nephropathy.
In HIV-infected persons, the incidence of MGUS is reported to be around 2.5%, with an approximately 4.5-fold increased risk of multiple myeloma.[11] There are case reports of multiple myeloma seen in HIV patients but those were not associated with renal involvement.[12] There is sparse documentation on myeloma presenting as cast nephropathy causing renal dysfunction in HIV patients.
Conclusion
Plasma cell disorders in HIV-infected patients are increasing and can range from polyclonal hypergammaglobulinemia to aggressive multiple myeloma. However, multiple myeloma presenting as myeloma cast nephropathy and causing renal dysfunction in HIV patients is sparsely described in the literature. Suspicious tubular casts in HIV nephropathy need detailed workup by immunohistochemistry/immunofluorescence on renal biopsy and detailed hematological workup to rule out an associated plasma cell dyscrasia.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Accelerated development of collapsing glomerulopathy in mice congenic for the HIVAN1 locus. Kidney Int. 2009;75:366-72.
- [Google Scholar]
- Collapsing glomerulopathy: A clinically and pathologically distinct variant of focal segmental glomerulosclerosis. Kidney Int. 1994;45:1416-24.
- [Google Scholar]
- HIV-associated nephropathy: A unique combined glomerular, tubular, and interstitial lesion. Mod Pathol. 1988;1:87-97.
- [Google Scholar]
- Myeloma-like cast nephropathy in human immunodeficiency virus (HIV)-infected patients: Recognition of a new pattern in two cases. Am J Clin Pathol. 2013;140:A186.
- [Google Scholar]
- Human immunodeficiency virus (HIV) infection and the kidney. Ann Intern Med. 1990;112:35-49.
- [Google Scholar]
- Plasma cell disorders in HIV-infected patients: Epidemiology and molecular mechanisms. Biomark Res. 2013;1:8.
- [Google Scholar]
- Evidence of B cell clonal expansion in HIV type 1-infected patients. AIDS Res Hum Retroviruses. 2001;17:1507-15.
- [Google Scholar]
- In vitro infection with HIV enables human CD4+T cell clones to induce noncognate contact-dependent polyclonal B cell activation. J Immunol. 1991;146:3413-8.
- [Google Scholar]
- The spectrum of kidney diseases in patients with human immunodeficiency virus infection. Curr Opin Nephrol Hypertens. 1993;2:355-64.
- [Google Scholar]
- Tubulointerstitial nephropathies in HIV-infected patients over the past 15 years: A clinico-pathological study. Clin J Am Soc Nephrol 2013:930-8.
- [Google Scholar]
- Plasma cell disorders in HIV-infected patients: From benign gammopathy to multiple myeloma. AIDS Read. 2004;14:372.
- [Google Scholar]
- A unique presentation of multiple myeloma in an HIV patient. Indian J Med Res. 2013;137:815-6.
- [Google Scholar]







