Translate this page into:
Nail–Patella Syndrome: A Rare Cause of Nephrotic Syndrome in Pregnancy
Address for correspondence: Dr. I. N. Aboobacker, MIMS Hospital, Kozhikode - 673 016, Kerala, India. E-mail: ferozaziz@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Nail–Patella syndrome (NPS) is an inherited disease with characteristic nail, limb, and renal anomalies. While almost all patients manifest classical skeletal and nail abnormalities, renal involvement is seen in only 40% of patients. Asymptomatic proteinuria is the most common renal presentation. Although a substantial number of patients can progress to nephrotic range proteinuria, development of end-stage kidney disease is rare. Pathological abnormalities are appreciable only by electron microscopy. Our patient who had not been diagnosed with NPS previously presented with new-onset proteinuria during the second trimester of her first pregnancy. The characteristic physical and radiological features confirmed the diagnosis of NPS. Her clinical course was complicated by nephrotic syndrome with fetal loss at 22 weeks and postpartum renal vein thrombosis. Nephrotic state improved after termination of pregnancy. She was managed with angiotensin receptor blocker and anticoagulation. At the end of 2 years of follow-up, she has normal glomerular filtration rate with minimal proteinuria.
Keywords
Nail–Patella
nephrotic
thrombosis
Introduction
Nail–Patella syndrome (NPS) is a disease of autosomal dominant inheritance with nail, limb, and renal abnormalities.[1] Common causes of proteinuria during pregnancy are pregnancy-induced hypertension and primary glomerular disease. We present a rare cause of proteinuria in pregnancy, diagnosed by classical physical examination findings and radiological features.
Case Report
A 31-year-old primigravida was referred to our hospital at 20 weeks of pregnancy with newly detected proteinuria, normal blood pressure (BP), and anasarca. Antenatal follow-up at her primary center had been uneventful until 16 weeks when she was noted to have proteinuria. She had no symptoms to suggest systemic lupus erythematosus or vasculitis. Her medical history was significant for recurrent falls in childhood and corrective surgery for fixed flexion deformities in elbows, but no renal disease was reported. There was no history of delay in developmental milestones or history of consanguinity. Family history was unremarkable for renal disease.
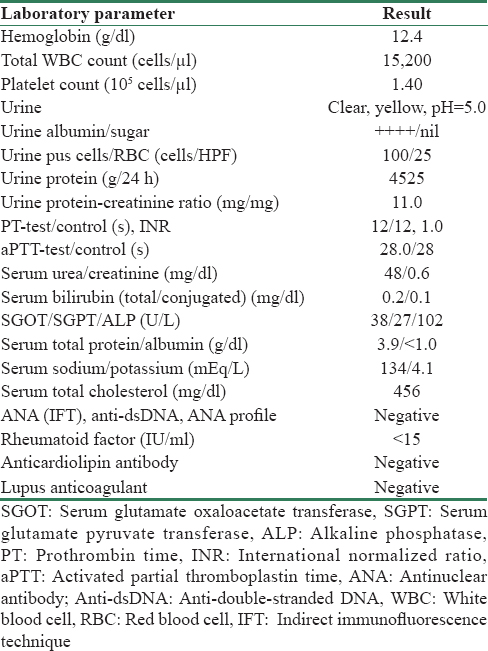
Examination revealed bilateral pedal edema and ascites with uterus of 20 weeks size. Fixed flexion deformities were evident in both elbows. She had flexion and hyperextension abnormalities of interphalngeal joints of both hands causing swan-neck deformity [Figure 1b] She had pitting of the nails in upper and lower limbs, which were more marked on the radial side [Figure 1a and 1c]. Her patellas were not palpable bilaterally. X-rays showed hypoplastic patella [Figure 1e], subluxation of the radial head at elbow [Figure 1f], and symmetrical bilateral iliac horns [Figure 1d]. Laboratory investigations are shown in Table 1. Antinuclear antibody, C3 and C4 complement, rheumatoid factor, and anticardiolipin antibody were negative. With documented hypoalbuminemia, hypercholesterolemia, and 11 g/day proteinuria, nephrotic syndrome complicating pregnancy secondary to NPS was diagnosed. Ultrasound showed normal unobstructed kidneys and intrauterine fetal demise of gestational age 22 weeks. Spontaneous expulsion of the fetus occurred after 48 h.
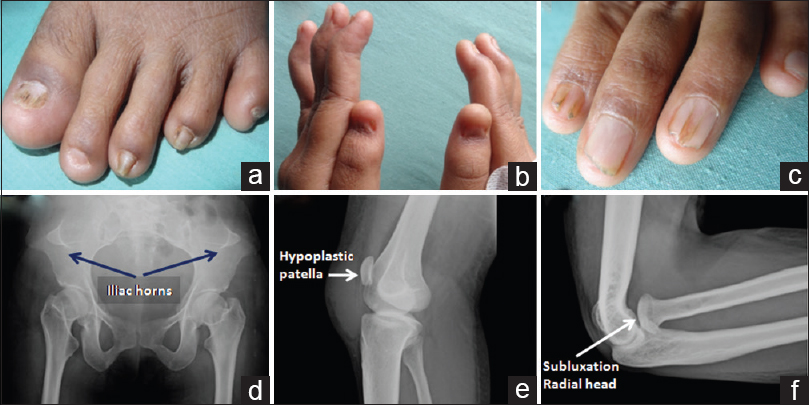
- (a and c) Dystrophic nails with abnormal ridging and splitting; (b)- flexion and hyperextension abnormalities of interphalangeal joints causing swan-neck deformity; (d) X-ray showing bilateral iliac horns arising from iliac crest; (e) X-ray showing hypoplastic patella; (f) X-ray of elbow joint showing posterior subluxation of radial head
Renal biopsy was deferred with ultrasound work-up for abdominal pain showing bulky left kidney with thrombosis of the left renal vein and the inferior vena cava 4 days after abortion. Anticoagulation was instituted. Serum creatinine was 0.8 mg/dl at discharge and remained normal throughout. Serum albumin improved from 1.1 g/dl at discharge to 2.4, 2.8, and 3.2 g/dl at 4, 12, and 24 months, respectively. Proteinuria reduced gradually reaching 700 mg/day at 2 years. Follow-up Doppler showed resolution of renal vein thrombosis.
Discussion
NPS is a rare autosomal dominant disease with classical skeletal and nail abnormalities often associated with renal disease.[1] Furthermore, known as “hereditary osteo-onychodysplasia,” the disease occurs due to mutations in the LMX1B gene located in the long arm of chromosome 9.[2] LMX1B serves as a transcription factor for the LIM-homeodomain that plays an important role in the development of limbs and kidneys in vertebrates.[3]
Limb and nail anomalies are near universal in NPS.[4] Common limb and pelvic abnormalities include patellar aplasia or hypoplasia, posterior subluxation of the radial head, hypoplasia of the lateral epicondyle and capitellum, and prominence of the medial epicondyle. The deformities of the elbow may lead to limitations in elbow movements, cubitus valgus, and pterygia (webbing of the elbow).[5] Our patient had fixed flexion deformities in both elbows which required correction at a young age though not identified as part of NPS at that time.
Iliac horns are bilateral symmetrical bone formations arising from the anterior superior iliac spine. Present in 70%–80% of patients, they are pathognomonic of NPS.[6] When sufficiently large, these may be detected by clinical examination. This characteristic abnormality was seen in our patient as well.
Limb abnormalities include underdevelopment of the proximal musculature of extremities, hyperextensibility of large joints, talipes equinovarus, calcaneovalgus, pes planus, and tight Achilles’ tendon.[5]
Fingernails are involved more frequently than toenails, and the thumb is the most severely affected. The radial side fingernails are more severely affected than ulnar as in our patient [Figure 1a and c]. For each individual nail, the ulnar side is more severely affected.[7]
Renal manifestations occur in 30%–40% patients, typically as asymptomatic proteinuria.[8] The proteinuria may increase during pregnancy because of hyperfiltration. Some patients progress to nephrotic syndrome although end-stage renal disease is rare.[9] Light microscopy and immunofluorescence are normal in almost all patients. Electron microscopy reveals irregular and lucent rarefactions containing clusters of cross-banded collagen fibrils within the glomerular basement membrane, pathognomonic of NPS.
Our patient developed proteinuria at 16 weeks of pregnancy and nephrotic syndrome at 22 weeks leading to fetal demise. The more common causes of proteinuria including pregnancy-induced hypertension as well as primary and secondary glomerular diseases were excluded by normal BP and negative serologies. The classical physical and radiological features confirmed the diagnosis of NPS. Severe hypoalbuminemia and postpartum state caused the renal vein thrombosis.[10] Immunosuppressives were not administered as there was a progressive improvement in serum albumin and reduction in proteinuria on follow-up. Renin angiotensin aldosterone axis blockade was given. At 2 years, she has minimal proteinuria and normal kidney function.
Conclusion
NPS is a rare cause of nephrotic syndrome in pregnancy. Prompt diagnosis by clinical and radiological features can help avoid renal biopsy. Patients who carry a diagnosis of NPS with minimal renal involvement should be warned of the possibility of worsening proteinuria during pregnancy which can affect maternal and fetal well-being.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Disorders of the nails. In: Nelson Textbook of Pediatrics Vol 2. (20th ed). Philadelphia: Elsevier; 2016. p. :3197.
- [Google Scholar]
- Genetic counselling in hereditary osteo-onychodysplasia (HOOD, Nail-Patella syndrome) with nephropathy. J Med Genet. 1988;25:682-6.
- [Google Scholar]
- Loss-of-function mutations in the LIM-homeodomain gene, LMX1B, in Nail-Patella syndrome. Hum Mol Genet. 1998;7:1091-8.
- [Google Scholar]
- Nail-Patella syndrome: A review of the phenotype aided by developmental biology. J Med Genet. 2003;40:153-62.
- [Google Scholar]
- Nail-Patella syndrome: A review of 44 orthopaedic patients. J Pediatr Orthop. 1991;11:737-42.
- [Google Scholar]
- Bilateral accessory iliac horns: Pathognomonic findings in Nail-Patella syndrome. Scintigraphic evidence on bone scan. Clin Nucl Med. 2000;25:476-7.
- [Google Scholar]
- Nail-Patella syndrome. Overview on clinical and molecular findings. Pediatr Nephrol. 2002;17:703-12.
- [Google Scholar]
- Genotype-phenotype studies in Nail-Patella syndrome show that LMX1B mutation location is involved in the risk of developing nephropathy. Eur J Hum Genet. 2005;13:935-46.
- [Google Scholar]
- Hypercoagulability, renal vein thrombosis, and other thrombotic complications of nephrotic syndrome. Kidney Int. 1985;28:429-39.
- [Google Scholar]







