Translate this page into:
Nephrology in Karnataka
Corresponding author: Attur Ravindra Prabhu, Department of Nephrology, Kasturba Medical College, Manipal, Manipal Academy of Higher Education, Manipal, Karnataka, India. Email: ravindra.prabhu@manipal.edu
-
Received: ,
Accepted: ,
How to cite this article: Rao IR, Janardhana AY, Prabhu AR. Nephrology in Karnataka. Indian J Nephrol. doi: 10.25259/IJN_142_2024
Abstract
Karnataka, a southern Indian state, exhibits a vibrant cultural and economic landscape. This paper provides an overview of nephrology services in Karnataka, drawing on government data, a literature review, and a survey of 147 dialysis centers and hospitals. The inception of nephrology in Karnataka dates to the early 1970s. Kidney care services have remained primarily centered in the capital city of Bengaluru. There are around 200 nephrologists and 300 dialysis centers (168 under the Pradhan Mantri National Dialysis Program), with hemodialysis being the predominant modality. Transplant services are offered in 69 centers, most in the capital city. Nephrology training is offered at 20 centers. Challenges remain, including the uneven distribution of services, fluctuating dialysis costs, and restricted access to peritoneal and home dialysis. There is a lack of comprehensive epidemiological data, necessitating the establishment of a statewide CKD registry.
Keywords
Chronic kidney disease
India
History
Dialysis
Kidney transplant
Nephrology
Karnataka
Introduction
Located in South India, Karnataka is renowned for its rich history, vibrant culture, delicious cuisine, and advancements in information technology (IT). The state boasts a diverse geography, ranging from coastal regions along the Arabian Sea to the lush Western Ghats and the arid Deccan Plateau. Its population of 6.41 crores with an area of 191,791 km2, makes it the eighth-most populous and the sixth largest state in India.1 Its capital, Bengaluru, is a bustling metropolis and a global IT hub, earning it the moniker “Silicon Valley of India.” Home to some of the leading educational institutions in India, the state has a literacy rate of 75.6%, which is above the national average.1 Driven by agriculture, IT, and manufacturing sectors, it is the fifth largest in India in terms of economy, with a gross domestic product (GDP) of INR 20.5 trillion (USD 260 billion) and a per capita income of INR 301,673 (USD 3,634).2
The Indian Council of Medical Research–India Diabetes (ICMR-INDIAB) study recently reported that approximately one in ten individuals in Karnataka had diabetes mellitus (DM), while one in three had hypertension.3 The precise burden of chronic kidney disease (CKD) in the state is unclear due to the absence of a registry, but it is expected to rise with the growing prevalence of diabetes and hypertension. We present the evolution and the current state of nephrology services in Karnataka based on data from the following sources: (a) websites of government and state health departments, news articles, and other relevant sources, (b) PubMed literature search, and (c) a survey conducted by the authors, in which data from 147 dialysis centers and hospitals in the state were collected.
History of nephrology in the state and important milestones
Nephrology services in Karnataka started in Bengaluru with the establishment of the Bangalore Kidney Foundation (BKF) on February 5, 1979, headed by Dr. Nandakishore Chintamani Talwalkar. Subsequent years witnessed a steady growth of services, mostly localised to the capital city [Figure 1].4,5 The first dialysis unit in a state government-run hospital was established in 1986 at Victoria Hospital with Dr. K.S. Siddaraju at its helm. Dr. Talwalkar formed an informal association of nephrologists, which included Dr. K.D. Phadke, Dr. K.S. Siddaraju, Dr. H.D. Balaji, Wing Cdr S.J. Singh Khurana, Dr. Srinivasa N.S., Dr. Shivakumar K.A., and Dr. K.S. Ramprasad.4 In 1986, comprehensive kidney care services were established by Dr. Sundar at M.S. Ramaiah Medical College, Bengaluru, and in 1991 at Manipal Hospital, Bengaluru, by Dr. H. Sudarshan Ballal. Dr. K.C. Gurudev established a full-fledged kidney care services at Mysuru and Dr. V. Narayanan Unni at Manipal, Udupi, around the same time, marking the spread of nephrology services outside of Bengaluru. North Karnataka was relatively devoid of nephrology services till 1995 when Dr. Jagadish Jamboti established the department at KLE Hospital in Belgaum.
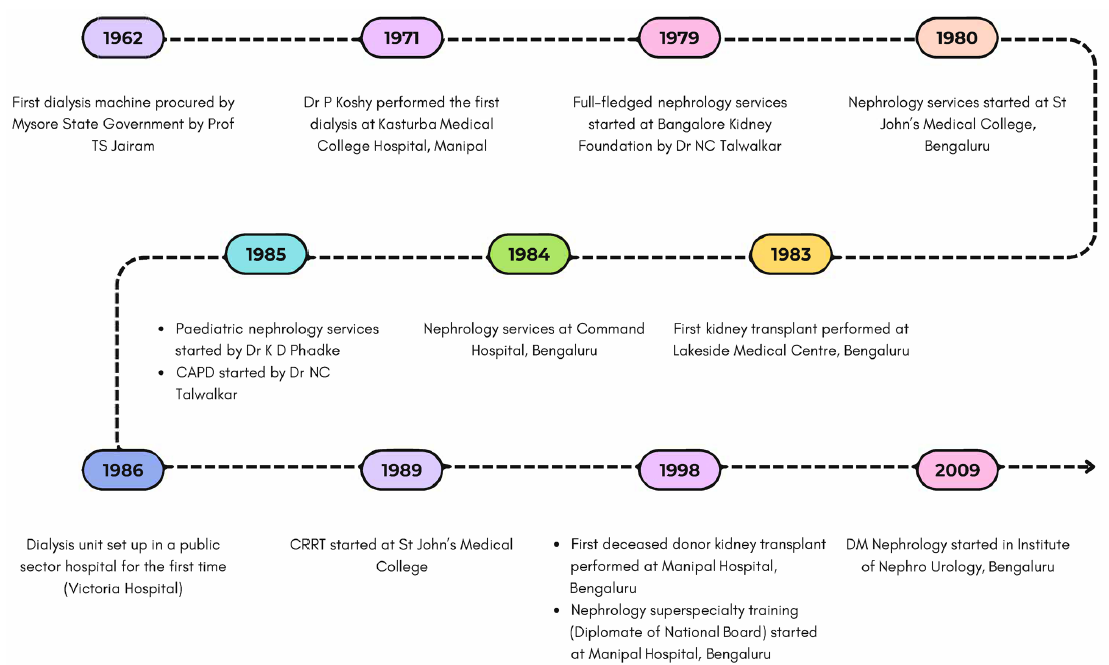
- A timeline of nephrology services in Karnataka. CAPD: continuous ambulatory peritoneal dialysis, CRRT: continuous renal replacement therapy, PD: Peritoneal dialysis, DM: Doctorate of Medicine.
Nephrology workforce in Karnataka
Our survey indicates that there are 203 nephrologists, or 3.3 per million population (pmp), in the state, which is higher than the national average of 1.9 pmp.6 Notably though, approximately half the workforce is concentrated in Bengaluru. There are 20 nephrology training programs, with an intake of 54 nephrology trainees per year [Table 1]. A one-year interventional nephrology fellowship program has recently launched in Bengaluru. There are 17 diploma and 29 undergraduate/postgraduate programs offering renal replacement and dialysis technology courses. No statistics are available for trained dialysis nurses, technicians, and renal dieticians.
| Statistics for the state | |
|---|---|
| Number of nephrologists | 203 |
| Number of nephrology training programs |
DM Nephrology: 11 DM Pediatric Nephrology: 1 DNB Nephrology: 8 |
| Annual intake of nephrology trainees |
DM Nephrology: 34 DM Pediatric Nephrology: 2 DNB Nephrology: 18 |
| Dialysis centers | Approximately 300 (168 under PMNDP) |
| Transplant centers | Sixty-nine centers (44 in Bengaluru) |
| Number of patients on dialysis |
HD: Approximately 7500 (3750 under PMNDP) PD: Approximately 326 |
| Transplanted patients |
Total to date: Over 7000 Annually: Approximately 850 in 2023 |
| Modality of KRT | HD: 95.3%, PD: 4.7%7 |
| Frequency of HD |
Three-week: 59.3%7 Two-week: 35.3% Other/irregular: 3.4% |
| PD exchanges per day |
Four-day: 81.7%7 Three-day: 18.3% APD: 5.7%7 |
| Vascular access |
Initial: Temporary catheter in 72%7 Long term: AVF in 87.9% |
APD: automated peritoneal dialysis, AVF: arteriovenous fistula, HD: hemodialysis, KRT: kidney replacement therapy, PD: peritoneal dialysis, PMNDP: Pradhan Mantri National Dialysis Program, DM: Doctorate of Medicine, DNB : Diplomate of National board.
Kidney care services in Karnataka and funding
Hemodialysis (HD) is the preferred modality of kidney replacement therapy, and our survey indicated that 90–95% of patients with end-stage kidney disease (ESKD) were on HD and <10% on peritoneal dialysis (PD). Approximately 50% began maintenance HD with a dialysis catheter. In a multicentric cross-sectional study by the Nephrology Association of Karnataka, including 32 hospitals (representing 16% of all dialysis centers), Conjeevaram et al. found that the dialysis catheter was the initial vascular access in 75% of patients, of which <5% being a tunneled catheter [Table 1].7 Routine monitoring of Kt/V was not done.7
Based on a public-private partnership model, the Pradhan Mantri National Dialysis Program (PMNDP) has penetrated all 31 districts of the state.8 At present, there are 168 functioning dialysis centers (with 541 dialysis machines) empanelled under the PMNDP (146 in taluk hospitals and 22 in district hospitals), and an additional 50 dialysis centers are planned. While there is a lack of data on the total number of dialysis centers, we estimate that, including private hospitals/dialysis units, there are more than 300 dialysis centers in the state. Of the 147 dialysis centers that participated in our survey, 76% belonged to the private sector, while 6.8% were standalone. Conjeevaram et al. reported that dialyzer reuse was practiced in 90% of dialysis centers.7 The state government is currently in the process of making single-use dialyzers mandatory in all its dialysis units.
Under the PMNDP, weekly visits/teleconsultation by nephrologists has been mandated; however, it has been reported that nephrologists do not regularly supervise more than two-thirds of standalone dialysis centers in the state.9 Our survey found that 45% of the surveyed dialysis centers in the state had no full-time nephrologist, and 17% were managed by general physicians or dialysis technicians alone. Approximately half of ESKD patients pay out-of-pocket for dialysis, while 31.8% of patients were supported by a government subsidy, 13.6% by private health insurance, and 1.3% by charitable organizations.7
Procedures such as tunneled catheter insertions and kidney biopsies are performed widely. Nephrologist-driven interventional services, including arteriovenous fistula (AVF) surgery and endovascular procedures, are offered at four centers, with others relying on vascular surgeons, interventional radiologists, or cardiologists. Comprehensive conservative kidney care services are still fledgling. A supportive care program for ESKD and an end-of-life care policy have been introduced in one group of hospitals. Nephropathology services started in 2007 in Bengaluru and remain predominantly concentrated there, although they are available in some medical colleges. Facilities for treating patients with acute kidney injury are available in most centers.
There are 69 registered organ transplant centers, of which 60% are in Bengaluru. Data on live donor kidney transplantation are not available. Our survey found that about 850 kidney transplants were done in 2023, with 70% being living donor transplants. Approximately 7000 kidney transplants have been carried out in the state. Of the 6006 patients registered in the deceased donor kidney waiting list, 1418 have been transplanted. Transplant centers in the private sector constitute 95%. In 2019, the state government launched the free organ transplantation scheme for patients below the poverty line, with 73 kidney transplants done as of 2022.
Challenges to CKD management in the state and future directions
Nephrologists and kidney care services in the state are mainly concentrated in the capital city of Bengaluru and tier II cities. The cost of dialysis services varies among centers, ranging from INR 400 to INR 3000 (from USD 5.7 to USD 42.8) per session, and patients often start dialysis in private dialysis centers and later shifting to government-run centers or reduce the frequency of dialysis due to financial constraints.10 Most health insurance schemes cover only inpatient care and only some, including Employees’ State Insurance (ESI), cover outpatient dialysis costs. Several standalone units are managed solely by technical personnel and thus are not equipped to handle emergencies.10 PD is underutilized and remains a cost-prohibitive modality, with the state not yet including it under the PMNDP. Currently, government funding for PD is available only for a limited number of patients under nephrology care at the premiere government institute in Bengaluru (Institute of Nephro-Urology). Home HD facilities are practically nonexistent. Kidney transplants are heavily reliant on living donors, and although there has been a steady increase in the number of deceased donors from three in 2007 to 178 in 2023, the average waiting time is four years.
Epidemiological data from the state is sparse. Anupama et al. recorded a CKD prevalence of 6.3%; however, the results were limited to a small pocket in Central Karnataka and lacked generalizability.11 Notably, the study highlighted a significant prevalence of CKD even in the rural population. The authors found that the prevalence of CKD was higher than that of diabetes in the region and that 45% of CKD patients were non-proteinuric, raising the suspicion of CKD of unknown etiology.11 A subsequent case-control study in the region found no association between heavy metals and CKD.12
Conclusion
Despite the tremendous progress in nephrology services in the state over the last five to six decades, a number of challenges still need to be addressed. There is a need for a statewide registry, development of robust data collection systems, screening and patient education programs, and research which addresses the unique aspects of CKD in this region.
Acknowledgments
The authors wish to thank Dr. Rammohan Bhat and the members of the Nephrology Association of Karnataka for their valuable contributions to this paper.
Conflicts of interest
There are no conflicts of interest.
References
- Karnataka population census 2011, Karnataka religion, literacy, sex ratio – Census India. Available from: https://www.censusindia.co.in/states/karnataka [Last accessed 2024 February 26]
- Economic Survey 2021–22 – Planning, Programme Monitoring and Statistics Department. Available from: https://planning.karnataka.gov.in/info-4/Reports/Economic+Survey+2021-22/en [Last accessed 2024 February 26]
- The ICMR-INDIAB study: Results from the national study on diabetes in India. J Indian Inst Sci. 2023;103:21-32.
- [CrossRef] [Google Scholar]
- NAK. Home - NAK doctors. Available from: https://nakdoctors.com/ [Last accessed 2024 March 11]
- About BKF – Bangalore kidney foundation. Available from: https://www.bkfindia.in/about-us/about-bkf/ [Last accessed 2024 March 11]
- Global dialysis perspective: India. Kidney360.. 2020;1:1143-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Clinico-epidemiological profile of dialysis services in Karnataka, India – A multicentric exploratory study. Indian J Nephrol. 2022;32:223-32.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Home | Pradhan Mantri National Dialysis Programme. Available from: https://pmndp.mohfw.gov.in/en [Last accessed 2024 March 18]
- Yasmeen A. Foundation complains to human rights commission on absence of nephrologists in govt. dialysis centres. The Hindu. 2023; Available from: https://www.thehindu.com/news/national/karnataka/foundation-complains-to-human-rights-commission-on-absence-of-nephrologists-in-govt-dialysis-centres/article66409789.ece [Last accessed 2024 February 26]
- Accessibility and quality of haemodialysis services in an urban setting in South India: A qualitative multiperspective study. BMJ Open. 2022;12:e052525.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prevalence of chronic kidney disease among adults in a rural community in South India: Results from the kidney disease screening (KIDS) project. Indian J Nephrol. 2014;24:214-21.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Heavy metals and pesticides in chronic kidney disease – Results from a matched case–control study from a rural population in Shivamogga district in South India. Indian J Nephrol. 2019;29:402-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]








