Translate this page into:
Nephrology Services in Telangana
Corresponding author: Manisha Sahay, Department of Nephrology, Osmania Medical College and General Hospital, Hyderabad, Telangana, India. E-mail: drmanishasahay@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sahay M, Guditi S, Yadla M. Nephrology Services in Telangana. Indian J Nephrol. doi: 10.25259/IJN_456_2024
Abstract
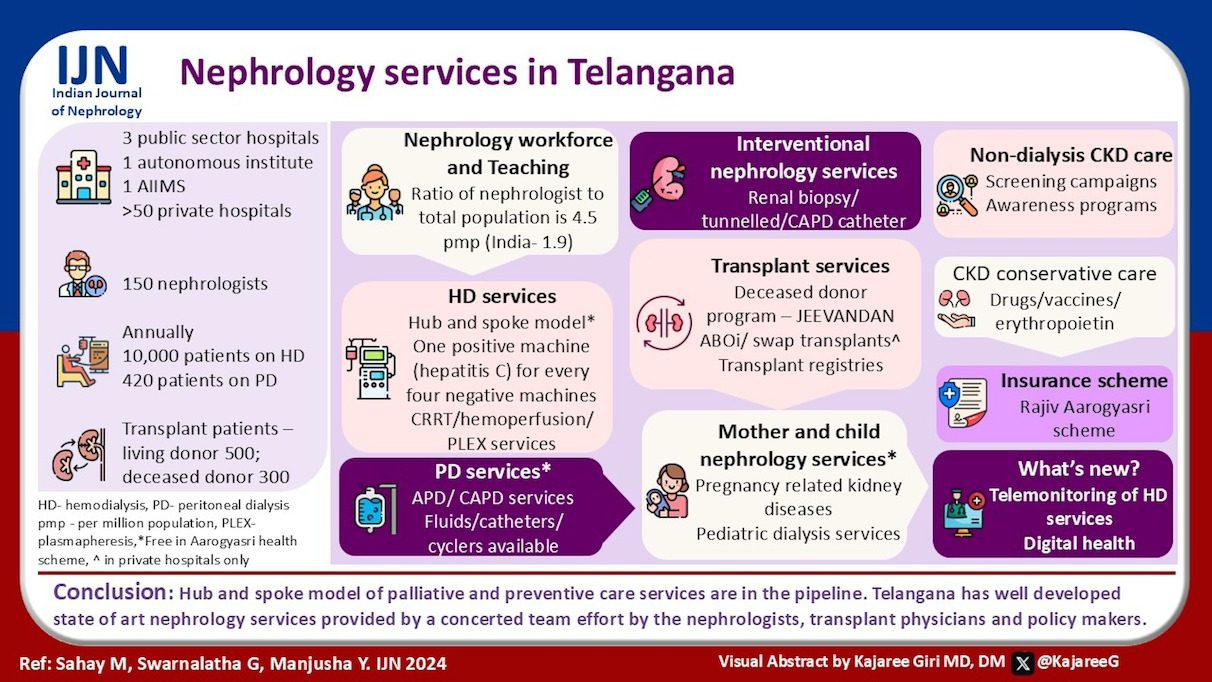
Telangana has well-developed state-of-art nephrology services. The state boasts of a unique hub-and-spoke model of hemodialysis and an active deceased donor program called “Jeevandan.” The state was one of the first to initiate the public-private model of kidney care under the cashless “Aarogyasri” scheme. Digital health has made easy access to lab investigations for the doctors as well as patients. Telemonitoring of remote dialysis units is another policy undertaken by the Telangana government that has immensely improved the dialysis quality. This review describes the various nephrology services available, current state of renal care services in the state.
Keywords
Telangana
Nephrologists
Aarogyasri scheme
Hemodialysis
Kidney transplantation
Introduction
Telangana was a part of the erstwhile united Andhra Pradesh until June 2014, when it became the 29th state of India. Telangana has an area of 1,12,077 sq. km, with a population of 39.64 million (61% rural) and population density of 307/sq. km. The state has 33 districts [Figure 1]. The per capita GDP is ₹383,426 (2023–2024), and the sex ratio is 988 females per 1000 males. Agriculture is the chief source of income for the state’s economy.1

- Telangana state districts.
Three large public sector hospitals, Osmania General Hospital (OGH), Gandhi Hospital (GH), and Mahatma Gandhi Memorial Hospital (MGMH) in Warangal; an autonomous institute, Nizam Institute of Medical Sciences (NIMS), a newly established All India Institute of Medical Sciences (AIIMS) at Hyderabad, and more than 50 private hospitals currently provide nephrology services in the state [Table 1].
| Number of hospitals providing kidney care services |
Hyderabad 2-state government AIIMS, Bibi Nagar 1 autonomous (NIMS) 55 private sector hospitals Khammam - 4 private hospitals Karimnagar - 6 private hospitals Mancherial - 1 private hospital Mehboobnagar - 1 private hospital Nizamabad - 1 private hospital Nalgonda - 1 private hospital Suryapet - 1 private hospital Warangal - 7 (1 government + 6 private) |
| Number of nephrologists | 150 out of which around 20 qualified nephrologists are in government sector |
| Number of transplant centers |
51 living donor transplant centers 40 deceased donor transplant centers |
| Number and range of nephrology training programs |
24 DM seats per year (19 in Hyderabad, 5 in Warangal) 16 DNB seats per year |
|
Number of nephrology trainees (total and passing out annually) |
Total no. of trainees: 90 out of which 55 are DM trainees DM trainees 24 per year DNB trainees 16 |
| Number of centers with intervention nephrology facilities | 50 |
| Number of patients on dialysis (In center HD, home HD, PD) |
In center, 4000 patients per month in hub-and-spoke model (PPP model data), approximately another 5000 in private sector Home hemodialysis - 15 (Nephroplus) Peritoneal dialysis - 420 Automated PD (home) - 50 (company data) |
| Number of transplanted patients (annual) |
Living donor 500 Deceased donor 250–300 |
| Current practice of HD and PD (frequency, adequacy) |
Thrice a week in most hub-and-spoke centers Number of hours and each dialysis session is captured Patients feedback taken Water quality monitored once in 3 months Single use dialysis Erythropoietin and iron provided free As per new system KT/V only will be mandatory for claims |
| Vascular access (% of patients getting dialysis through fistula/AVF) | 82% |
| Any kidney disease registry (CKD/Dialysis/Transplant) and the nature of data collected |
Deceased donor transplant data captured State deceased donor program - Jeevandan Organ donors 5323 (till Aug 23, 2024), 2112 kidneys retrieved from Jan 01, 2023 |
| Community engagement and involvement | On world kidney day |
| Research scenario | Multidisciplinary research units in Government medical colleges |
| Any specific policy initiatives |
Hub and spoke model of dialysis with 3 major hospitals as hub centers and each hub center with around 20-30 spoke centers in districts. Nephroflow for dialysis centers Teleconsultations between district and government hub hospitals Teleconsultation between hub-and-spoke centers Digital nephrology |
AIMS: All India Institute of Medical sciences, NIMS: Nizam’s Institute of Medical sciences, DM: Doctor of Medicine, DNB: Diplomat of national board, HD: Hemodialysis, PD: Peritoneal dialysis, AVF: Arteriovenous fistula, CKD: Chronic kidney disease.
History of Nephrology services
Dr. A. Gopal Kishen was the first nephrologist of the combined state of Andhra Pradesh. He completed his Commonwealth Fellowship (1974–1976) from Manchester, United Kingdom. In the 1970s, OGH acquired a Travelon coil dialyzer [Figure 2]. The Nephrology Department of Manchester Medical College, UK, gifted three Lucas machines and Kiil board dialyzers. The first hemodialysis was done in the Nephrology Department at OGH on Lucas machine donated by the Manchester Medical College. Kidney transplant services started at OGH in 1982, with the first kidney transplant on May 16, 1982. The donor and recipient are doing well after 42 years. The DM Nephrology course started in 1994 under the leadership of Dr. Girish Narayen and Dr. Anuradha Raman, who also established regular hemodialysis and acute peritoneal dialysis services. Maintenance dialysis was initiated in 2009 across the state under the then Director of Medical Education, Dr. T. Ravi Raju. Dr. Manisha Sahay, along with Dr. Ismal, initiated continuous ambulatory peritoneal dialysis (CAPD) and automated peritoneal dialysis (APD) programs in OGH and deceased donor transplantation program in 2013 and continuous renal replacement therapy (CRRT) in 2020. Dr. R. Rajmallaiah established the Department of Nephrology at GH, which grew under the leadership of Dr. Pradeep Deshpande and Dr. Manjusha Yadla.
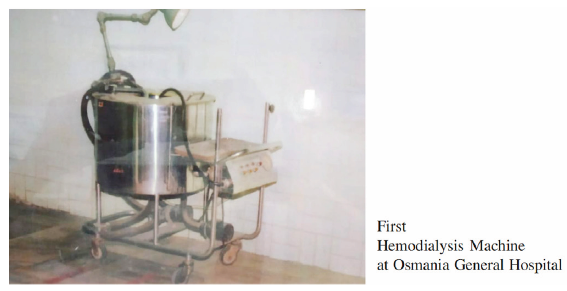
- Travelon coil dialyzer at Osmania General Hospital.
Nizam Institute of Medical Sciences is an autonomous institute. Professor BVR Murthy established nephrology services at NIMS in 1987. In 1998, Prof KV Dakshinamurthy joined the department and started the DM Nephrology program. He and Dr. Neela Prasad contributed to the growth of nephrology services. Subsequently, Dr. Sree Bhushan Raju, Dr. T. Gangadhar, and Dr. G. Swarnalata are spearheading the nephrology services at NIMS.
The private sector hospitals have also seen phenomenal growth, with several state-of-the-art nephrology units, such as the Apollo, Yashoda, KIMS, Care, AINU, AIG, and Virinchi hospitals. Hemodialysis, CRRT, and transplant services are available in all major hospitals [Table 1].
Nephrology Workforce and Teaching
Telangana has 4.5 nephrologists per million of the population, which is better than the national average of 1.9 per million population. Telangana has 14 medical colleges. In addition to the existing nephrology departments in Hyderabad, new nephrology units are being sanctioned in the district hospitals. DNB courses are offered in multiple private hospitals.2 There is an active Hyderabad Nephrology Forum, which holds monthly meetings, CMEs, workshops, and mock exams for postgraduates. It has an active website and a newsletter.
Hemodialysis
Hemodialysis (HD) services were initiated under a cashless government scheme (Aarogyasri) in erstwhile Andhra Pradesh in 2009.3 This was a unique initiative in the country. At the time of bifurcation in 2014, seven centers in the Telangana were providing dialysis under this scheme. With the innovative concept of the hub-and-spoke dialysis model in 2017, 3 hub hospitals, Osmania, Gandhi, and NIMS, with 36 spoke centers were established, which later increased to 46 centers. Each hub hospital has a large dialysis unit and is the monitoring center for the connected spoke hospitals.4 Telangana has a policy of single use of dialyzers. The Aarogyasri scheme, currently provides a reimbursement of Rs. 18,500 per month for 10–12 dialysis sessions [Table 2].5 Centers are expected to provide intravenous iron and erythropoietin, generally administered at 4000 units twice a week. Iron sucrose, and ferric carboxymaltose are available in the government sector, while darbepoietin and CERA are unavailable. Till now, 5000 hemodialysis patients are registered to receive an Aasra pension of Rs. 2000 per month to help cover their healthcare expenses. Patients with kidney ailments also receive free bus passes to travel to the nearest dialysis facility. Several private hospitals are a part of network hospitals under Aarogyasri and provide free services, while most major corporate hospitals provide paid nephrology services. Hepatitis B vaccination and antiviral treatment for hepatitis C infection are provided free of cost in government hospitals.
| Package name | What is included in the package? | Amount (INR) |
|---|---|---|
| Medical management of AKI | 19,710 | |
| Medical management of nephrotic syndrome | Basic investigations, renal biopsy, serology, Immunosuppression | 16,890 |
| Medical management of rapidly progressive renal failure | Includes basic tests, renal biopsy, serology, Immunosuppression | 30,766 |
| Medical management of chronic renal failure 1 | Includes basic investigations, dialysis disposables | 30,870 |
| Maintenance hemodialysis for CRF | Dialysis disposables | 18,500 |
| Live donor kidney transplant | transplant surgical equipment | 161,100 |
| Deceased donor kidney transplant | transplant surgical equipment | 161,100 |
| Induction therapy and first month post-cadaver transplant | Basiliximab or ATG | 100,000 |
| Maintenance immunosuppression per month for the initial 6 months | Tacrolimus, MMF, and steroids and tacrolimus level | 21,000 |
| Maintenance immunosuppression post-transplant per quarter after initial 6 months | Tacrolimus, MMF, and steroids and Tac level | 28,500 |
AKI: Acute kidney injury, CRF: Chronic renal failure, MMF: Mycophenolate mofetil, ATG: Anti thymocyte globulin
Continuous renal replacement therapy is performed free of cost in the public sector hospitals. Hemoperfusion for poisoning cases is done free of cost in the government sector. Plasmapheresis is also available and is usually done by machine under the nephrology unit. Hemodiafiltration (HDF) was available in NIMS and private sector in the past. A new HDF package was included for state government hospitals, along with several others in July 2024 [Table 3].
| Ambulatory peritoneal dialysis (APD) | 34,500 |
| Tunneled or Non-tunneled catheter insertion | 30,000 |
| Peritonitis infectious complications and catheter removal | 44,000 |
| Continuous renal replacement therapy in AKI | 2,25,000 |
| CAPD catheter insertion | 40,000 |
| CKD/ESRD complications | 44,000 |
| Nephrotic syndrome complication (fluid overload) | 44,000 |
| Catheter-related blood stream infections (CRBSI) code | 44,000 |
| CT venogram/Fistulogram | 5,520 |
| Fistuloplasty | 48,700 |
| Unspecified medical package (for all departments) | 50,000 |
| Donor evaluation code (Pretransplant evaluation/brain dead patient workup) | 70,000 |
|
Rare/genetic disease Evaluation/pediatric CAKUT evaluation |
Upto 50,000 |
|
Pretransplant live and cadaver Recipient evaluation through Experts Committee approval |
50,000 |
| HDF/high-flux HD through Experts Committee approval | 25,000 per 10 sessions per month |
| Hemoperfusion/hemadsorption for organ failure cases due to illness and accidental drug overuse (suicide attempts excluded) | 50,000 |
AKI: Acute kidney injury, CAPD: Continuous ambulatory peritoneal dialysis, CKD: Chronic kidney disease, ESRD: End stage renal disease, CT: Computerised tomography, CAKUT: Congenital abnormality of kidneys and urinary tract, HD: Hemodialysis, HDF: Hemodiafiltration
Peritoneal Dialysis
Acute peritoneal dialysis (PD) is available predominantly in government hospitals, and is usually reserved for young patients and those with hemodynamic instability. The disposables and fluids are provided free of cost under the Aarogyasri scheme. Government hospitals cater to PD services in HIV patients. Continuous ambulatory peritoneal dialysis (CAPD) is supported by the government. CAPD bags required for a month’s time (90–120 bags) are issued to all the patients. Centrally sponsored schemes such as ESI and CGHS also cover PD. New packages have been developed for automated PD and CAPD catheterization. Cyclers are available in the government sector and are used during the break-in period or when patients are hospitalized. Home cyclers are, however, not provided. The growth of PD is suboptimal, however, with 420 patients on CAPD in Telangana.
Interventional Nephrology
Renal biopsy, central catheterizations including tunneled catheter placement, CAPD catheter insertions, percutaneous are performed regularly in the major private sector hospitals and the five major government hospitals. Free vascular access centers for creation of AV fistula under the Aarogyasri scheme are available in OGH, GH, and NIMS. The number of surgeries for vascular access however are more in private sector hospitals.
Kidney Transplantation
Kidney transplantation is available in two government hospitals (OGH and GH), at NIMS and in around 40 private hospitals. The state follows the AP Transplant Act of 1995, and adopting new rules is under consideration. Every year, around 500 living donor kidney transplants are conducted in Telangana.
The deceased donor program of Telangana is recognized as one of the best in the country.6 The number of deceased organ donors in Telangana in 2022 was 194, the highest in the country, followed by Tamil Nadu (156), Karnataka (151), Gujarat (148), and Maharashtra (105). A total of 716 organs (263 kidneys) were transplanted followed by Tamil Nadu (553), Karnataka (435), Gujarat (399), and Maharashtra (305). The deceased donor program, initiated in 2010, called Jeevandan utilizes an online platform developed by the National Informatics Center (NIC).7 The state also conducts deceased donor felicitation programs for the families of deceased donors. ABOi and swap transplants are limited to private hospitals. Efforts are underway to develop a live donor, swap transplant, and ABOi registry. Telangana is a hub for transplant tourism, with 70 foreign nationals transplanted in 2023.
Telangana runs a training program for transplant coordinators that is one of its kind in the country. Faculty from different specialties and hospitals hold teaching sessions for these coordinators to train them in all aspects of organ transplantation, including grief counseling, organ packaging, transport, and post-donation care of the family. Awareness programs about organ donation are conducted regularly across schools, colleges, and other organizations.
Kidney transplantation is free under Aarogyasri, and patients who have undergone transplantation under this scheme are provided with a lifelong free supply of life-saving medicines [Table 2]. A state-of-the-art State Organ Transplant Center (SOTC) would soon be operational in one of the major government hospitals.
Mother and Child Nephrology Services
Pregnancy-related nephrology services are given predominantly in government hospitals. Surveillance and treatment of pregnancy-related kidney diseases (acute or chronic) are available under cashless schemes in government hospitals. Pregnant acute kidney injury (AKI) patients are given diverse extracorporeal treatments including hemodialysis, CRRT, peritoneal dialysis, and HDF services depending on the indication. Nephrology care for children is available in major government hospitals and few private hospitals. Interventions such as pediatric catheter placement for dialysis, vascular access creation, biopsy, and transplantation are also available.
Non-dialysis CKD care
Packages are available under the Aarogyasri scheme for management of nephrotic syndrome [Table 2]. New packages have been added for genetic testing as well [Table 3]. Multiple activities are performed to mark prominent health days, such as World Kidney Day, World Hypertension Day, and World Diabetes Day in public and private sector hospitals. Packages are being proposed for non-dialysis chronic kidney disease (CKD) care to detect kidney disease early and institute measures to retard progression.
Conservative Care
Patients visit the district hospitals, primary health centers (PHCs), and tertiary hospitals, where they are provided dietary advice and free medicines such as RAASi and other medicines for non-dialysis kidney care. SGLT2i (Sodium Glucose transporter 2 inhibitor) (dapagliflozin), iron injections, and erythropoietin are currently available only at tertiary care centers. Vaccinations such as hepatitis B are provided free of cost. These are supplied under the stage budget. Darbepoietin, HIF-PHIs (hypoxia inducible factor - prolyl hydroxylase inhibitors), Finerenone, and Empagliflozin are currently unavailable in the government sector.
Insurance and Out-of-pocket expenditure
Rajiv Aarogyasri Scheme is a unique community health insurance designed to eliminate out-of-pocket expenditure by providing financial protection to families living below the poverty line as enumerated and photographed in Food Security card and available in Civil Supplies Department database. A total of 1672 treatments are covered under the converged scheme (kidney care packages are mentioned in Tables 2 and 3). All transactions are cashless. All PHCs, the first points of contact, area or district hospitals and network hospitals, are provided with help desks manned by AAROGYA MITHRAs to guide the patients. The merger of Telangana government’s Aarogyasri Health Scheme and the Center’s Ayushman Bharat Scheme has increased the maximum health protection from ₹2 lakh to ₹5 lakh per year.8
Other insurance schemes include the employment-linked employee’s health scheme for state government employees and pensioners and dependent family members, CGHS, ESIS, Railways, RTC, Aarogya Bhadratha of the Police Department, and Aarogya Sahayatha of the Prohibition and Excise Department.
Diagnostic Services
The Telangana Diagnostics Program, which started in January 2018, provides a range of diagnostic services at subsidized rates: Complete blood picture (CBP), urine examination, serum creatinine, electrolytes, liver function test, and blood sugar. It is coupled with T-Diagnostic smartphone application that allows patients to view and download their medical reports. In addition, the diagnostic services in major government hospitals of OGH, GH, and NIMS are digitalized under the CDAC program with digital reports available to doctors.9
New policy initiatives
Telangana Health Profile is another recently launched technology-driven healthcare initiative. This involved surveying 5,20,301 individuals at Mulugu and Siricilla, collecting their physical details and blood samples for conducting a battery of tests, leading to the creation of individual health records.10
Telemonitoring of dialysis services: This is a new initiative where the hub dialysis centers situated at OGH, GH, and NIMS can supervise all the spoke dialysis centers under them on a daily basis, and the nephrologists can interact with the patients and dialysis technicians and nurses as well as the in-charge dialysis doctors. This helps with troubleshooting as well as the monitoring dialysis quality. Physical visits are also undertaken once in 3 months or more frequently if required.
Future directions
More focus needs to be directed toward the prevention of kidney diseases.11 Palliative care services for CKD need to be strengthened and supported by packages as has been done for oncology patients. The existing hub-and-spoke model for dialysis can be utilized for prevention of kidney diseases [Figure 3]11 and palliative care services. Vascular intervention suites need to be developed in public sector hospitals where vascular access dysfunction can be managed. The Telangana Government has planned for establishment of such Apex and spoke centers for vascular access. Strategies need to be in place for effective biomedical waste disposal from dialysis units12,13 [Table 4].
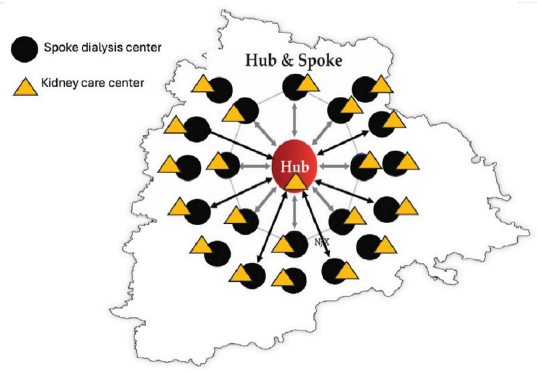
- Hub-and-spoke model of dialysis and kidney disease prevention.
| Need for preventive strategies | Utilizing the hub and spoke dialysis centers as centers for screening and prevention of CKD |
| Need for preventive care packages for CKD | Discussion with policy makers to have packages under Ayushman Bharat and various state schemes to create new packages for CKD screening and prevention |
| Need for palliative care packages for CKD | Palliative care packages under government schemes (like those existing for oncology) for CKD patients, such as palliative dialysis, package for symptom relief (pain medicines, relief of pruritis) |
| Need for vascular intervention suites in government sector | Discussion with stakeholders and establishment of vascular intervention units in public sector hospitals (already underway in Telangana) |
| Policies for biomedical waste reduction, reuse, and recycle | Recycling of dialyzers for road-laying, reuse of dialysis wastewater in toilets or for gardening, harnessing solar power |
CKD: Chronic kidney disease.
A concerted team effort by the nephrologists, transplant physicians and surgeons, and policymakers will go a long way in establishment of state-of-art nephrology services in the state and different parts of the country.
Conflicts of interest
There are no conflicts of interest.
References
- Available from: https://www.telangana.gov.in/about/state-profile/ [Last accessed on 2023 Aug 10].
- Available from: https://mbbscouncil.com/listing/ [Last accessed on 2023 Aug 10].
- Utilization, costs, and outcomes for patients receiving publicly funded hemodialysis in India. Kidney Int. 2018;94:440-445.
- [CrossRef] [PubMed] [Google Scholar]
- Hemodialysis at doorstep – “Hub-and-Spoke” model of dialysis in a developing country. Saudi J Kidney Dis Transpl. 2020;31:840-849.
- [CrossRef] [PubMed] [Google Scholar]
- Available from: https://rajivaarogyasri.telangana.gov.in/ASRI2.0/ [Last accessed on 2023 Aug 10].
- 333.1: A review of expanded criteria kidney donations and organ utilization in state run deceased donor transplantation program (Jeevandan) in India. Transplantation. 2019;103:S85-6. November 2019
- [CrossRef] [Google Scholar]
- Available from: https://jeevandan.gov.in [Last accessed on 2023 Aug 10].
- Available from: https://nha.gov.in/PM-JAY [Last accessed on 2023 Aug 10].
- Available from: https://tdiagnostics.telangana.gov.in/ [Last accessed on 2023 Aug 10].
- Available from: https://www.telangana.gov.in/ [Last accessed on 2023 Aug 10].
- Hub and Spoke Model for kidney care – From prevention to treatment. Indian J Nephrol doi: 10.25259/IJN_165_2024
- [PubMed] [Google Scholar]
- assessment of biomedical waste generation in dialysis units: A prospective observational study-is it time for “Green Dialysis”? J Assoc Physicians India. 2023;71:49-52.
- [CrossRef] [PubMed] [Google Scholar]
- Trends of biowaste generation in hemodialysis units under the hub-and-spoke model: act and save. J Egyptian Society of Nephrology and Transplantation. 2022;22:29-34.
- [Google Scholar]







