Translate this page into:
Nephrology Services in the Indian Armed Forces
Corresponding author: Prem P. Varma, Department of Nephrology, Primus Hospital, Chanakyapuri, New Delhi, India. E-mail: varmapp123@rediffmail.com
-
Received: ,
Accepted: ,
How to cite this article: Varma PP, Nair RK, Behera V. Nephrology Services in the Indian Armed Forces. Indian J Nephrol. doi: 10.25259/IJN_210_2024
Abstract
The Armed Forces Medical Services (AFMS) provide comprehensive medical care to Armed Forces personnel, veterans and their dependants. Nephrology services in the AFMS have grown into state-of-the-art facilities at 12 nephrology centers that provide >500 monthly haemodialysis, > 120 kidney transplant each year, and other aspects of nephrology care including latest interventions and critical care nephrology. The highlights of care provided by the AFMS include its free wholesome medical care to all dependant clientele, robust record keeping, and its emergence as torch bearer for peritoneal dialysis in the country, with >600 CAPD patients.
Keywords
Nephrology
Indian armed forces
Introduction
India has the fourth largest armed forces in the world, operating in varied terrains and climates. The Armed Forces Medical Services (AFMS) came into existence in 1948 to provide all-round medical care to the personnel of the Army, Navy, and Air Force across the country.1 Medical care and infrastructure have advanced significantly, and today the AFMS handles all medical issue.
AF workload and Ex-Servicemen Contributory Health Scheme (ECHS)
The 10 million serving personnel, veterans, and their dependents make up 0.7% of the Indian population.2 The AFMS has over 230 hospitals, of which 100 are located in field areas, and others are located in rest of the country. Nearly 50 of these hospitals (Tier 2) have specialist facilities while 10–12 (Tier 3-Tertiary) have super specialties, forming the ideal pyramidal referral-based healthcare network. Nephrology services are located in the tertiary care hospitals [Figure 1]. During war times, all establishments are focused on managing war casualties, utilizing excellent air and land-based evacuation system. It also has ambulance trains with functional operation theatre facilities and wards to hold patients.
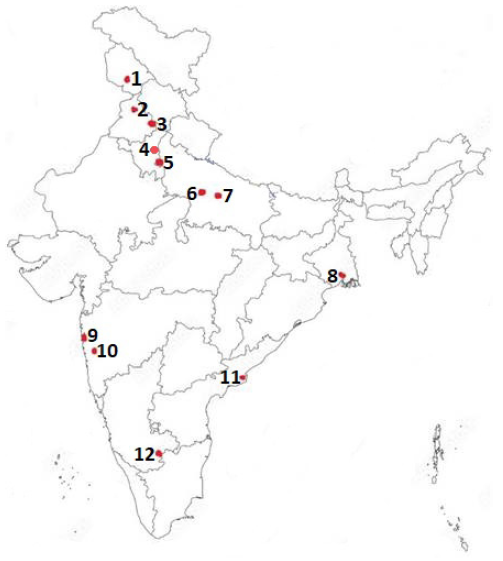
- 1. Command Hospital Northern Command (CHNC) Udhampur, 2. Military Hospital Jallandhar, 3. Command Hospital Western Command (CHWC) Chandimandir, 4. Army Hospital, Research and Referral, 5. Base Hospital Delhi (BHDC), 6. Air Force Hospital Kanpur, 7. Command Hospital Central Command (CHCC) Lucknow, 8. Command Hospital Eastern Command (CHEC) Kolkata, 9. Indian Naval Hospital Ship (INHS) Asvini Mumbai, 10. Command Hospital Southern Command (CHSC) Pune, 11. Command Hospital Air Force (CHAF) Bengaluru, and 12. INHS Kalyani, Visakhapatnam.
The Ex-Servicemen Contributory Health Scheme (ECHS) was set up on 01 Apr 2003 as a health insurance scheme to provide comprehensive cashless medical facilities to all veterans and their dependants for a one-time premium of Rs 30,000– Rs 120,000. Today, there are 28 regional ECHS centers and 426 ECHS polyclinics spread across the country. Regional ECHS centers empanel local private/corporate hospitals/ laboratories for services unavailable with them or the service hospital nearby.2 Most veterans in their dependents receive dialysis in empanelled hospitals.
History of nephrology and landmark events in Armed Forces
In the 1960s, Major General Inder Singh (senior-most physician of armed forces), an astute clinician and a visionary, understanding the importance of super specialities, sent physicians for training in Cardiology, Neurology, Endocrinology and Nephrology. Colonel NN Sharma was sent for short-term training in Nephrology and on his return, he started the nephrology practice at Army Hospital, Delhi Cantt.
Hemodialysis (HD) services started in the Armed Forces at Command Hospital, Pune in the 1960s using Drake Willock/Travenol machines. According to Gen HS Uberoi, one of the senior-most nephrologist of the Armed Forces, a patient was given HD for acute kidney failure in 1965 at Command Hospital, Pune, while he was an MD student in Armed Force Medical College.
Colonel RS Hoon (later Lt Gen) as Professor (Medicine) at AFMC Pune gave Capt. (later Col) Akhil Mishra ‘Role of Peritoneal Dialysis in AKI’ as his dissertation topic in 1969. For the first time in the AFMS, 20 patients of AKI received acute peritoneal dialysis from 1969 to 1971.
Prof. KS Chugh, fondly called ‘Father of Indian Nephrology’ in India, started formal training in nephrology (DM Nephrology) in 1969 at PGIMER Chandigarh and the first batch of students consisting of Col K Bhattacharya (later Maj Gen) and Dr. MS Amaresan passed out in 1971.3 Col Bhattacharya was the first trained nephrologist of India and was the pioneer in starting a formal nephrology program in the Armed Forces in 1971. In next decade, Brig Yashpal, Maj Gen HS Uberoi, and Col Akhil Mishra, all trained by Prof. KS Chugh, became the torchbearers of nephrology services in the AF.
The first kidney transplant in the AFMS was performed in February 1991 at INHS Asvini, Mumbai by Surg. Cdr. R Malik, the nephrologist and Surg. Cdr. (later Vice Admiral) VK Saxena, the urologist. In May 1991, Army Hospital started its renal transplant program with Col Akhil Mishra as nephrologist and Col HS Bhatyal as the surgeon. After that, renal transplantation started in the Command Hospitals at Pune (1993), Kolkata (1998), Bangalore (1998), and Lucknow (2002). Col Yashpal and Col PP Varma (later Lt Gen) started the transplant program at Pune with Col. (later AVM) Madhusoodanan as transplant surgeon. Surg. Cdr. R Malik and Col PP Varma started transplant program at Kolkata with Col Tapan Sinha and Col Deepak Batura as surgeons. Wing Cdr. Gokul Nath started transplant in Bangalore and Col AS Narula (later Lt Gen) and Col AK Hooda (later Lt Gen) along with Col DK Jain as surgeon started transplant program in Lucknow. The first cadaveric transplant was performed at the Army Hospital Research and Referral (AHRR) in 1998.
Col. PP Varma started the Dr. NB Nephrology training program at the AHRR in 2005, where 25 students have been trained. In 2006, AORTA (Armed Forces Organ Retrieval and Transplant Authority) was raised at AHRR, which has given a huge boost to deceased donor transplant program in the AF.
Present nephrology establishment in AFMS
Today, the AFMS has 12 nephrology centers with 25 nephrologists (including 3 women nephrologists) [Figure 1]. Each of these centers has facilities for HD, PD and critical care nephrology, with 6 centers engaged in kidney transplantation.
Hemodialysis
The hemodialysis (HD) facility which started in Delhi and Pune in the 1960s–1970s has extended to 12 centers now catering to serving soldiers and their dependents. Table 1 depicts the hemodialysis statistics. Half of these centers provide hemodiafiltration. All centers have a facility for continuous renal replacement therapy (CRRT). More than 80% of patients are provided thrice in week hemodialysis.4
| Facility | Mean +SD |
|---|---|
| Hemodialysis sessions/month | 533.3 ± 225.9 |
| Maintenance hemodialysis patients/month | 55.0 ± 20.6 |
| Hemodialysis machines in each center | 12.6 ± 5.0 |
| Peritoneal dialysis patients per center | 56.7 ± 31.2 |
| Total transplants done by AFMS (till 2023) | 2718 |
| Total deceased donor kidney transplants done | 250 |
| Average kidney transplants per year | 96.2 ± 44.3 |
AFMS: armed forces medical services, AF: armed forces
Peritoneal dialysis
Peritoneal dialysis (PD) is provided by all 12 centers and a total of 680 patients are on PD as on December 2023, with about 57 patients at each center.4 It is interesting to note that in AF, number of patients on PD exceeds the number of patients on HD and AF is able to provide RRT to those in remote locations. All centers also offer automated PD to their patients. Acute PD is also done, it has been able to save lives in those with AKI due to snake bite, malaria, rhabdomyolysis or heat stroke in far flung areas.
Kidney Transplantation
6 AFMS centerscentres are regularly performing kidney transplant. The AFMS centers have together performed 2718 total kidney transplants by the year 2023, with AHRR being the leader (n = 1555). Of these 250 have been deceased donor transplants. ABO-incompatible transplants, sensitised patient transplants and swap transplants are routinely performed.5-8 AHRR has a state-of-the-art molecular lab and immunology set up. Out of 6 transplant centers, 4 have immunology labs and all have nephropathologists.
Interventional Nephrology
All centers are performing procedures like temporary dialysis catheter insertion, tunnelled catheter insertion, kidney biopsy and percutaneous PD catheter insertion using interventional facilities like ultrasound and Cath lab/ C Arm. Three centers are also engaged in AV fistula creation and central vein interventions.
Pediatric Nephrology
Six pediatric nephrologists in the AFMS provide comprehensive care to children, encompassing all modalities of dialysis, CRRT and renal transplantation. More than 35 pediatric renal transplants have been performed in the AFMS till date.
Approach to a Patient with ESKD in the Armed Forces?
The overall CKD prevalence in AF is similar to that in the general population.9 Extrapolating from Indian data around 800 new patients develop kidney failure every year.10 Since a dialysis dependent soldier can’t perform combat duties, they remain hospitalised till transplant or relief from service. On an average, 15–20% ESKD patients obtain a donor organ and 10% of these get a cadaveric donor through the AORTA. One-year, 5 year and 10 year estimated graft survival is 95.4% (SE, 0.01), 80.5% (SE, 0.03) and 53.1% (SE, 0.09) respectively and patient survival at one year is 93.2% (SE, 0.01).5 Unlike the general population, 100% of AF personnel who need RRT, receive it. As all hospitals have robust medical stores system, so all drugs remain available to all patients throughout their life.
How kidney care in the AFMS is unique!!
-
1.
The AFMS has over 25 nephrologists for 4 million population (average 6.25 nephrologists per million population), which is far better than the country average.4
-
2.
The AFMS provides free renal replacement therapy and drugs (HD, PD or RRT) to all throughout their life, thus avoiding catastrophic healthcare expenditure.4
-
3.
AFMS is a leader in PD, and contributes >10% of country’s CAPD population.
-
4.
About 15% of all patients with kidney failure receive kidney transplantation, higher than the national figure of 6-8%.
-
5.
Intervention nephrology services are available in all centers in AFMS.
-
6.
Since every soldier is assigned a record office on recruitment, the health records are always available irrespective of their place of service.
Conclusion
The nephrology care in the AFMS is one of the best among government setups. It has remained at forefront in starting nephrology services in India and offers free comprehensive nephrology care to its clientele with the latest cutting-edge facilities.
Acknowledgment
We are grateful to Gen HS Uberoi VSM and Col Akhil Mishra VSM for giving details of nephrology history and facts about earlier times of AFMS.
Conflicts of interest
There are no conflicts of interest.
References
- Ministry of Defence. Archived from the original on 26 February 2012. Retrieved 31 December 2020.
- Ex-servicemen contributory health scheme. Indian J Community Med. 2007;32:241-2. Available from: https://doi.org/10.4103/0970-0218.37685
- [CrossRef] [Google Scholar]
- Five decades of Indian nephrology: a personal journey. Am J Kidney Dis. 2009;54:753-63.
- [CrossRef] [PubMed] [Google Scholar]
- Global dialysis perspective: India. Kidney360. 2020;1:1143-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Renal transplantation - an experience of 500 patients. Med J Armed Forces India. 2007;63:107-11.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Kidney transplantation: The journey across a century. Med J Armed Forces India. 2023;79:631-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Cadaveric renal transplantation: Our experience at a tertiary care center in India. Med J Armed Forces India. 2020;76:58-62.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Use of immunoadsorption columns in ABO-incompatible renal transplantation: A prospective study at a tertiary care center in India. Med J Armed Forces India. 2021;77:15-21.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prevalence of early stages of chronic kidney disease in apparently healthy central government employees in India. Nephrol Dial Transplant. 2010;25:3011-7.
- [CrossRef] [PubMed] [Google Scholar]
- The incidence of end-stage renal disease in India: A population-based study. Kidney Int. 2006;70:2131-3.
- [CrossRef] [PubMed] [Google Scholar]







