Translate this page into:
Nephrology Services in Uttar Pradesh
Corresponding author: Narayan Prasad, Department of Nephrology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, Uttar Pradesh, India. E-mail: narayan.nephro@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Prasad N, Meyyappan J, Veeranki V. Nephrology Services in Uttar Pradesh. doi: 10.25259/IJN_170_2024
Abstract
Uttar Pradesh comprises 16.5% of India’s population and is the most populated state of the country. Compared to the central government budget of 2.1% of GDP on health care, the state has promised an expenditure of 7.2% on health care. The hot, humid summer and dry winter predispose people to many vector-borne diseases, which increase the surge of acute kidney injury. The trained medical and non-paramedical personnel are insufficient to cater for the estimated population of 48,000 end-stage kidney disease patients in the UP. Each district has a dialysis unit; however, the number of dialysis machines is insufficient, and the kidney transplant facilities are limited mainly to the capital of the state. Peritoneal dialysis penetration is very low.
Keywords
Kidney disease care
Uttar Pradesh
Dialysis
Kidney transplantation
Medical and paramedical personnel
Introduction
Uttar Pradesh (UP), covering a total area of 240,928 square kilometers, with a population of 240 million and a population density of 1001 people/km2, is the most populous state in India. It is the habitat of 16.5% of the total population of India.1 It comprises 18 divisions and 75 districts, organized into four zones: Eastern, Western, Awadh (Central), and Bundelkhand, based on distinct geographic locations with differing socioeconomic conditions and health infrastructure [Figure 1]. The health infrastructure, which also covers kidney disease care, is better in Western and Central UP, with a higher number of tertiary care institutions and hospitals compared to the Eastern part and Bundelkhand.
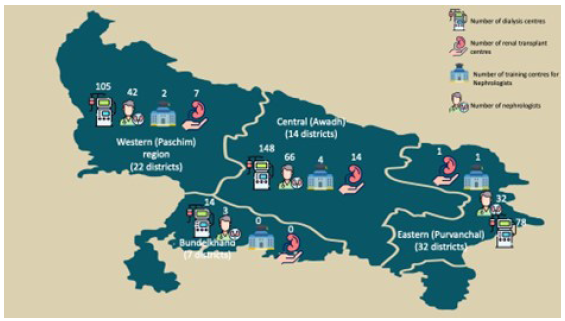
- Distribution of hemodialysis centers, approved renal transplant centers, nephrologists and training institutes across the four regions of UP. Map not drawn to scale. Only for schematic representation and numbers depicts the total number available in the region.
Weather Conditions and Kidney Diseases
The state experiences subtropical hot-humid summers, fairly good rainy weather and dry winters, predisposing them to many vector-borne diseases like dengue, malaria, filariasis, leishmaniasis, etc., that may involve kidneys. With the outbreak of dengue and malaria, the incidence of acute kidney injury (AKI) also increases. The Ganges, Yamuna, Sarayu, and Ghaghara rivers traverse their landscape, sustaining agriculture and livelihoods for the majority. Primarily agrarian, its people engage in farming, with sectors like handloom weaving and tourism contributing significantly to the economy. Waterborne diseases and parasitic infestation are not uncommon, which lead to diarrheal illness, causing dehydration, AKI, hospitalization, and rarely death. Farmers working barefoot in the waterlogged field also experience leptospirosis, causing AKI and multi-organ dysfunction, which was initially thought to be the disease of the coastal part of India.
Community-acquired AKI is common. Sepsis and tropical infections were identified as the primary cause, with approximately 8.2% of patients progressing to chronic kidney disease (CKD).2 Non-institutional and unattended deliveries contribute to pregnancy-associated AKI.3 The widespread misuse of over-the-counter availability of nephrotoxic painkillers, antibiotics, traditional remedies, poisoning, snake bites and exposure to toxins such as fish gallbladder contribute significantly to it. Despite hot-humid conditions, the use of pesticides, and farmers working in the fields, the state has no obvious hotspots of CKD of unknown etiology at present.
Socioeconomic Condition and Healthcare Expenditure
As per the National Family Health Survey (NFHS)-5, 22.93% of the UP population is poor,3 and overall literacy rate is also low (74%), with male and female literacy of 82% and 66.1%, respectively.4 The economy of the state is the fifth largest among states in India with gross state domestic product (GSDP) of Rs. 24.99 trillion (US$313 billion) in 2022–23.5
The Central and State Governments’ budgeted expenditure on the health sector reached 2.1% of GDP in financial year (FY) 2023, 2.2% in 2022, against 1.6% in FY2021; however, the current budgeted expenditure stood at around 1.98%, insufficient to achieve the goal of National Health Policy, 2017 envisioning health expenditure to reach 2.5% of the GDP by 2025. The current expenditure falls below the world average.
The central health budget of current financial year rose by 12% over the previous year, which is merely a cover for inflation. In contrast, the health and family welfare budget of UP of FY 2022–23 has been increased by 20%, from about USD 471 million to USD 568 million as of March 2023. The state budgeted to spend 7.2% of the state GDP on health.6 The state leads the nation with 4.15 crore beneficiaries under the Ayushman Bharat Yojana, translating to approximately one in every six individuals.7
Kidney Disease Burden
The exact burden of CKD in state is unknown. With an estimated CKD population of 800 per million population and end-stage kidney disease (ESKD) of 200 per million population in India, UP likely has 192,000 people with CKD and 48000 patients with ESKD. Diabetic nephropathy is the leading cause of ESKD followed by chronic interstitial nephritis and chronic glomerulonephritis. Majority patients belong to the lower-middle socioeconomic conditions and are poorly educated. People develop CKD at an early age or the median age, 40–50 years, the most productive years for the patient. Approximately, 55% of patients are referred late to nephrologists, with consequent high risk of the emergency start of dialysis with temporary vascular access and had a higher risk of mortality.8
ESKD Care and Renal Replacement Therapy Provision
All modalities of renal replacement therapy (RRT), maintenance hemodialysis (MHD), peritoneal dialysis (PD) and renal transplantation (RT) are available within the state; however, the capacity to cater all ESKD patients is challenging, and limited to major cities. With just 145 trained nephrologists, there aren’t enough to meet the high demand for CKD care. Internists primarily take care of the CKD patients at early stages, during the period when intervention can retard the progression of CKD. Despite the easy availability and low cost of generic preparations the use of renin–angiotensin system (RAAS) blockers and SGLT-2 inhibitors is relatively low. Less than 50% use RAAS blockers in early CKD in India, including this state.9 Only 8 out of 67 medical colleges (35 government and 32 private) in the state had nephrologists, the majority of nephrologists (n = 45) workingin the state are centered in the state capital. Early CKD patients are unable to access specialist nephrology care. The comparison of nephrology services metrics between UP and India are shown in Table 1.
| Parameter | Uttar Pradesh* | India* |
|---|---|---|
| Chronic kidney disease (%) | 8.5 | 8.5 |
| End stage renal disease | 152 | 152 |
| Chronic dialysis | 38 | 49.2 |
| Nephrologists | 0.60 | 1.9 |
| Hospitals equipped with hemodialysis | 1.29 | NA |
| Annual PD incidence | 0.79 | 1.42 |
| Patients on hemodialysis | 129 | 129 |
| Renal transplant incidence | 1.97 | 3.98 |
| Renal transplant centers | 0.09 | 0.11 |
| Cadaveric transplant incidence | 0.06 | 0.37 |
| Hemodialysis machines | 6.75 | NA |
| Hemodialysis centers | 1.43 | 0.36 |
| Peritoneal dialysis centers | 0.08 | 0.14 |
Dialysis Coverage
Universal coverage for RRT is not provisioned in the state. Most of the patients who develop ESKD opt for MHD. Patients below the poverty line had free access to MHD, covering all costs under NHM, but they have to travel to the district headquarters where free dialysis facilities have been set up. A large majority of lower middle-class people had to pay out of pocket, and are unable to sustain the cost of dialysis, ultimately resulting in inadequate dialysis and high drop out, similar to what is observed in other states.10
Hemodialysis Facilities
The distribution of hemodialysis facilities across the state in various districts is shown in Figure 1. There are 345 dialysis units, distributed across various districts. Among these, 22 units are under public management, 79 are under public–private partnership, and 244 are private.11 All the 75 district hospitals have hemodialysis units with 5–10 hemodialysis machines in each center. Three service providers under the public–private partnership are Heritage Hospitals in 40 centers with 540 machines, DCDC Kidney Care in 21 centers with 210 machines, and Eskag Sanjeevani Group in 18 centers with 180 machines. The largest dialysis unit is the Sanjay Gandhi Postgraduate Institute of Medical Sciences (SGPGIMS) with 125 stations.
The cost of hemodialysis varies, ranging from INR 1300 to INR 2000 per session in the public sector and public–private partnership hospitals, totaling INR 130,000 - 200,000 annually for dialysis treatments alone. In contrast, private-sector dialysis costranges from INR 3500 - 4000 per session, attracting mainly the upper socio-economic class and those eligible for such reimbursement. Most individuals below the poverty line opt for free dialysis under the Pradhan Mantri National Dialysis Programme (PMNDP) and Ayushman Bharat Insurance Scheme. Many patients are covered under government-sponsored schemes like the Central Government Health Scheme and a self-insurance scheme for financial support.
The survey of the 345 units revealed that only 198 units (57.3%) are supervised by nephrologists, and the rest by internists or technicians. These unsupervised centers have higher drop-out rates and higher hepatitis C virus infection and CRBSI. Regular monitoring of dialysis adequacy and dosage assessment are practiced in 205 units (59.4%), which is probably an overestimate. Dialysis is usually started with temporary catheters, with less than 10% of patients having functioning arterio-venous fistulas (AVF). Yet, within 12 months, over 60% of patients transitioned to AVF, and less than 1% utilizing arteriovenous grafts.
CRBSI rates range from 2 to 5 per 1000 catheter days, affecting approximately one-fourth of dialysis patients. Most centers (90%) are reusing dialyzers. A thrice-weekly dialysis regimen is predominantly accessible to affluent patients in corporate hospitals. Instead, twice-weekly sessions is the norm, especially in publicly funded facilities. With the availability of dialysis units in district hospitals, the distance to travel to dialysis centers was reduced to about 50 kilometers from approximately 100 kilometers. However, there is a need for improved surveillance to ensure the quality of care across the state.
Peritoneal Dialysis
The exact PD penetration rate is estimated to be less than 10%. At present, there are 325 patients on PD in UP; of them, 55 are on automated PD. An important reason for poor PD penetration is a lack of PD training. Only 3 centers within state are giving training for PD. The cost of MHD and PD appears the same and PD may be cost-effective if hidden costs of HD are added on during cost analysis.12,13 Another possible reason is physician disincentive due to a different reimbursement model. The PD peritonitis rate declined over the years from 0.63 episodes to 0.47 episodes per patient year.14 The cost of PD is not covered under PMNDP program in the state, however, CGHS and Government employees are getting reimbursement for PD.
Kidney Transplantation (KT)
According to the State Organization for Tissue and Organ Transplantation (SOTTO), a total of 23 centers, comprising 6 in public and 17 private sectors, are approved for KT in the state. Among these, 12 are located within the state capital.15 Only 2 public sectors hospitals, SGPGIMS and RMLIMS, are actively doing transplantation. Only SGPGIMS has all the facilities of transplant immunology work-up, and capability of performing high-risk transplantation including ABO incompatible KT. Of a total of 300–350 KT performed in the state annually, half are performed at one center, SGPGIMS. Given that KT facilities are concentrated in urban pockets like Lucknow, Noida and Ghaziabad, there is a huge unmet need for the rest of the state. In addition, there is a huge organ shortage across the state. ABO incompatible KT and paired kidney exchange in SGPGI address the gap only partly. Deceased donor transplantation is in its early stages, with only two public and one private sector hospital performing fewer than a dozen KT per year in the state.
Conservative Kidney Management
The concept of conservative kidney management is primitive and only two public sector institutions conceptually advocate for conservative kidney management. With the aging of the general population in the state, there is a dire need to evolve the CKD for the elderly requiring RRT.
Interventional Nephrology
Most nephrologists in the state are trained in vascular access creation and non-tunneled and tunneled venous catheter placement during their training period. SGPGIMS has a post-doctoral fellowship program in Intervention Nephrology approved by the International Society of Nephrology, and trains fellows from around the world and country. The department has dedicated two operation theatres for vascular procedures. Two centers train students for percutaneous Tenckhoff catheter insertion techniques for initiating PD.
Kidney Biopsy and Histopathology Reporting
All nephrologists are trained in kidney biopsy, however only 25% of nephrologists do kidney biopsy routinely. The major reason for the reluctance in doing kidney biopsy are the lack of facilities to tackle complications like bleeding and the shortage of trained nephropathologists. Only three public sectors had immunofluorescence facilities, and only one center, SGPGIMS, has in-house electron microscopy facilities for kidney pathology reporting.
Postgraduate Training
Nephrology services in UP was started in 1977 as a division of Internal Medicine at King George Medical University, Lucknow. The first dedicated nephrology department was established at the SGPGIMS, Lucknow in 1987, which subsequently became the leading center of nephrology training in the country. Other centers providing postgraduate training for nephrology are Ram Manohar Lohia Institute, Lucknow, and Institute of Medical Sciences, Banaras Hindu University, Varanasi. Every year, 12 DM and 6 DNB students start training in nephrology.16
Paramedical manpower
The state also faces a huge deficit of trained dialysis technicians and nurses. Only three centers provide dialysis technician courses. Most dialysis performed at district hospitals under PMNDP is performed by nurses or technicians with limited working knowledge. Inadequately supervised dialysis results in high complication rate and poor dialysis quality.
Future perspectives and challenges
The state government has started medical colleges in most districts, with a proactive approach to strengthen the healthcare infrastructure. However, there is an acute shortage of faculties and trained paramedics who meet the National Medical Council recognition. Extending kidney care services to smaller towns and rural areas is only possible by building infrastructure that is well-matched with urban infrastructure. The lessons of the success stories of public–private partnerships in setting up dialysis units across the state may be used in other areas of medical and nephrology education to enhance the quality of medical education. There is a need for the establishment of ESKD/KRT registries to monitor and improve the quality of the care provided and identify areas with the greatest need for improvement.
Conclusion
Kidney disease care in UP is improving but still has a long way to go to meet the demand of care in the state.
Conflicts of interest
There are no conflicts of interest.
References
- Uttar Pradesh Population 2024. Available from: https://worldpopulationreview.com/world-cities/uttar-pradesh-population [Last accessed on 2024 Mar 26].
- Community-acquired acute kidney injury in India: Data from ISN-acute kidney injury registry. The Lancet Regional Health - Southeast Asia.. 2024;21 Available from: https://www.thelancet.com/journals/lansea/article/PIIS2772-3682(24)00009-X/fulltext [Last accessed on 2024 Mar 26]
- [CrossRef] [Google Scholar]
- Health Performance : NITI Aayog, National Institution for Transforming India, Government of India. Available from: https://social.niti.gov.in/hlt-ranking [Last accessed on 2024 Apr 2].
- Hindustan Times. 2020. UP literacy rate poor than national average: Report. Available from: https://www.hindustantimes.com/education/up-literacy-rate-poor-than-national-average-report/story-04cd30glcG2IchqkB0TLaJ.html [Last accessed on 2024 Apr 2].
- India Brand Equity Foundation. About Uttar Pradesh: Tourism, Agriculture, Industries, Economy & Geography. Available from: https://www.ibef.org/states/uttar-pradesh [Last accessed on 2024 Apr 2].
- Benu P. BusinessLine. 2023. UP and Bihar budgeted more funds for healthcare in FY24. Available from: https://www.thehindubusinessline.com/data-stories/data-focus/up-and-bihar-budgeted-more-funds-for-healthcare-in-fy24/article66888707.ece [Last accessed on 2024 Mar 26].
- Ayushman Bharat Beneficiaries: At 4.15 crore, up has maximum ayushman bharat beneficiaries | Lucknow News - Times of India. Available from: https://timesofindia.indiatimes.com/city/lucknow/at-4-15-crore-up-has-maximum-ayushman-bharat-beneficiaries/articleshow/105276995.cms [Last accessed on 2024 Mar 26].
- Impact of early versus late referral to nephrologists on outcomes of chronic kidney disease patients in Northern India. Int J Nephrol. 2022;2022:e4768540.
- [CrossRef] [Google Scholar]
- Prescription practices in patients with mild to moderate CKD in India. Kidney Int Rep. 2021;6:2455-2462.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Utilization, costs, and outcomes for patients receiving publicly funded hemodialysis in India. Kidney Int. 2018;94:440-5.
- [CrossRef] [PubMed] [Google Scholar]
- HDIS-Haemo Dialysis Information System. Available from: https://hdis.upnrhm.gov.in/ [Last accessed on 2024 Mar 26].
- Peritoneal dialysis-first initiative in India: A cost-effectiveness analysis. Clin Kidney J. 2022;15:128-35.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Monthly cost of three exchanges a day peritoneal dialysis is same as of thrice a week hemodialysis in self-paying Indian patients. Indian J Nephrol. 2012;22:39-41.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Microbiology and outcomes of peritonitis in Northern India. Perit Dial Int. 2014;34:188-94.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- SOTTO-U. P. Available from: https://sottoupdoha.in/ [Last accessed on 2024 Mar 26].
- Available from: https://accr.natboard.edu.in/online_user/frontpage.php?v=4 [Last accessed on 2024 Mar 26].







