Translate this page into:
Nerve Epidermal Growth Factor-Like 1 Protein (NELL-1) Expression in Mercury-Related Membranous Nephropathy: Is It a True Association or a Chance Occurrence?
Corresponding author: Norton Stephen, Department of Pathology, All India Institute of Medical Sciences (AIIMS), Madurai, India. E-mail: norton.divya@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Srinivas BH, Stephen N, Priyamvada PS, Nachiappa Ganesh R, Parameswaran S, Gochhait D. Nerve Epidermal Growth Factor-Like 1 Protein (NELL-1) Expression in Mercury-Related Membranous Nephropathy: Is It a True Association or a Chance Occurrence? Indian J Nephrol. 2024;34:482-6. doi: 10.25259/IJN_109_2024
Abstract
Background:
Neural epidermal-like growth factor-like 1 (NELL-1) is a protein kinase C binding protein expressed in osteoblasts and renal tubules. It is expressed in 5%–25% glomerular cells at the mRNA level. Membranous Nephropathy (MN) is characterized by the presence of antibodies against certain types of antigens on the glomerular basement membrane. The most common one implicated in primary MN is an antibody against PLA2R. Many newer antigens have been discovered in the recent past, which are proven to cause secondary MN, one of which is NELL-1. NELL-1 has been associated with malignancy-associated MN and also recently associated with traditional indigenous medications containing mercury. In this study, we study the expression of NELL-1 in mercury-associated MN.
Materials and Methods:
Records of ten cases of Mercury -associated MN were retrieved from the Institute medical archives and NELL-1 Immunohistochemistry was performed in all ten cases.
Results:
NELL-1 was found to be positive in 50% of the cases of Mercury associated MN. In addition, mass spectrometric studies was performed, which revealed the common Mercuric compound associated to be ‘Swaskalpa’, ‘Sudarshana Melugu’ and ‘Rasagandhi Mezhugu’.
Conclusion:
This study highlights why it is important to diagnose mercury-associated MN by a pathologist by picking up the finer histopathological clues and by using NELL-1 immunohistochemistry, especially in PLA2R-negative patients. The former is true as most of the time a history of mercuric compound intake is missed out.
Keywords
Membranous nephropathy
Mercury
NELL-1
PLA2R
Introduction
Neural epidermal-like growth factor-like 1 (NELL-1) is a 90-kDa protein kinase C binding protein containing a secretory peptide predominantly expressed in osteoblasts and renal tubules. It is hardly expressed in the glomerulus, but 5%–25% of glomerular cells express NELL-1 at the mRNA level.1–3 Membranous nephropathy (MN) is characterized by the presence of antibodies against certain types of antigens on the glomerular basement membrane. The most common antigen implicated is the M type of Phospholipase A2 receptor antigen, which is responsible for about 70% of MN. The second identified antigen to be discovered was thrombospondin type-1 domain-containing 7A (THSD7A) which was detected in 1–3%. The rest of the associated antigen implicated in the pathogenesis of MN has been the topic of highlight for the past few years.4,5
By convention, MN was divided into primary and secondary types. While primary cases of MN were considered idiopathic, all the cases of secondary MN were associated with autoimmune disease, infection, malignancy, hematopoietic stem cell transplant (HSCT), sarcoidosis, and more. It was found that all cases of primary MN were PLA2R and THSD7A positive and all the cases of secondary MN were associated with the newer antigens.
With the advent of laser microdissection and tandem mass spectrometry, several new antigens have been discovered, which include EXT1/2 (Exostatin), NELL-1 (neural epidermal growth factor-like 1 protein), Semaphorin (SEMA 3B), procadherin 7, protocadherin FAT1, and neuron-derived neurotrophic factor (NDNF).6-8
Recent observations have suggested NELL-1-related MN to have an association with traditional indigenous medications (TIM) with mercuric compounds. In this study, we study the utility of NELL-1 in mercury-related MN.
Materials and Methods
A total of ten cases of MN related to mercury compound intake were obtained from the archives of the Department of Pathology at our institute. All the clinical details of cases of mercury-related MN were taken from the archives. The PLA2R status was available for all cases. The Institutional Ethics board of JIPMER, Puducherry has given ethical approval on November 2022 and has waived the consent as there were no direct human subjects involved.
Further, IHC with NELL-1 was performed on all ten cases of. Anti-NELL-1 Rabbit polyclonal Antibody (DAKO) was used in a dilution of 1:50 for the study. The control used for the study was no-mucinous colorectal adenocarcinoma glands, which served as the external control.8
Five micron-thick sections were taken on the surface of APES- (3-aminopropyltriethoxysilane) coated slides. Proper deparaffinization of the section was done by xylene, followed by rehydration with varying concentrations of alcohol. Antigen retrieval is done in TRIS wash buffer and endogenous peroxidase blocking is done by hydrogen peroxide on the given sections. Incubation with the primary antibody NELL-1 and secondary antibodies followed by staining. Application of DAB chromogen and Hematoxylin and Eosin stain were followed by dehydration, clearing, and mounting. The IHC stained sections were examined by two independent pathologists.
Mass spectrometry was done to find out the composition of the compounds in the TIM. The common ones that were found were Swaspakalpa, Sudarshana Melugu, and Rasagandhi Mezhugu. The mercury levels were detected in these compounds via Mass spectrometry and the levels were correlated with the NELL-1 expression.
Results
The median age of presentation of cases associated with TIM was 42.5, with 80% of the cases belonging to the female gender. In 60% of the cases, the indication for taking this indigenous medication is because of respiratory disorders; 20% of the cases were associated with back aches.
One was a known case of psoriasis and the other was for menorrhagia. Among the cases, the most common mercury compound in these indigenous medications was Swaskalpa (40%), Sudarshana Melugu (20%), and Rasagandhi Mezhugu (20%). Among the remaining cases, the compound could not be made out.
The median serum mercury levels were found to be 38.4 and the urinary mercury levels were found to be 39.2 [Table 1].
| Clinical Parameters | Membranous Nephropathy with TIM |
|---|---|
| Age | Median 42.5 years |
| Gender | 8:2 |
| Indication for drug |
Upper respiratory tract infection (URTI)(60%) Back ache (20%) Psoriasis (10%) Menorrhagia (10%) |
| Drug (Compound) |
Swaskalpa (40%) Sudarshana Melugu (20%) Rasagandhi Melugu (20%) Unknown (20%) |
| Presenting complaints | Nephrotic syndrome (100%) |
| Serum Creatinine | 0.9 (Mean) |
| eGFR | 85.7 (Mean) |
| Serum Albumin | 2.1 (Mean) |
| Urine PCR | 9.1 |
| Renal biopsy |
Membranous nephropathy (100%) Mesangial hypercellularity (30%) Tubulo-interstitial Nephritis (70%) |
| IF findings |
IgG, C3, Kappa, Lambda (100%) IgA, IgM, C1q (20%) |
| Serum Mercury | 38.4 |
| 24 Hr urinary Mercury | 39.2 |
| Treatment |
70% conservative treatment 30% steroids No chelating agents |
| Outcome |
Complete remission (90%) Lost to follow-up (10%) |
| Time of remission | 3.8 months |
| NELL-1 antibody |
Positive (50%) (GBM positivity) Negative (50%) |
| PLA2R antibody | Negative |
| HbsAg | Negative |
| HCV | Negative |
| HIV 1/2 | Negative |
TIM: Traditional Indigenous Medication, eGFR: estimated Glomerular filtration rate, PCR: Polymerase chain reaction, IF: Immunofluorscence, IgG: Immunoglobulin G, C3: Complement factor 3, IgA: Immunoglobulin A, IgM: Immunoglobulin M, NELL-1: Neural epidermal growth factor-1 like protein, HCV: Hepatitis C virus, HIV: Human Immunodeficiency virus, GBM: Glomerular basement membrane, MN: Membranous nephropathy, PLA2R: Phospholipase A2 receptor, HbsAg: Hepatitis B surface antigen.
Immunohistochemistry with NELL-1 was performed in these cases. It was found that NELL-1 was positive in 50% of the cases with localization to the glomerulus. In the rest of the cases, it was negative [Figures 1–4].

- H&E sections show glomerulus with uniform thickening of glomerular basement membrane with mild mesangial proliferation (40x), H&E: Hematoxylin & Eosin.
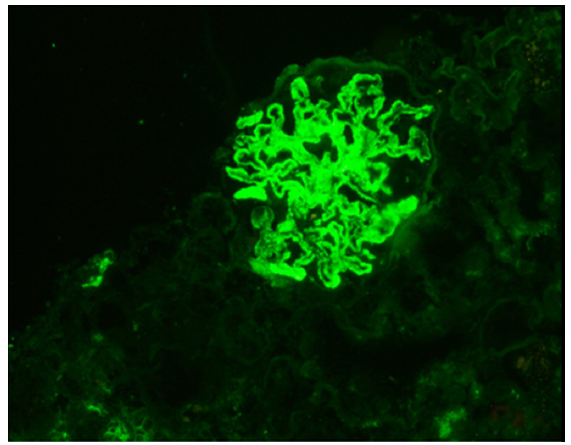
- IgG immunofluorescence positive in the glomeruli (intensity-3+), IgG: Immunoglobulin G.
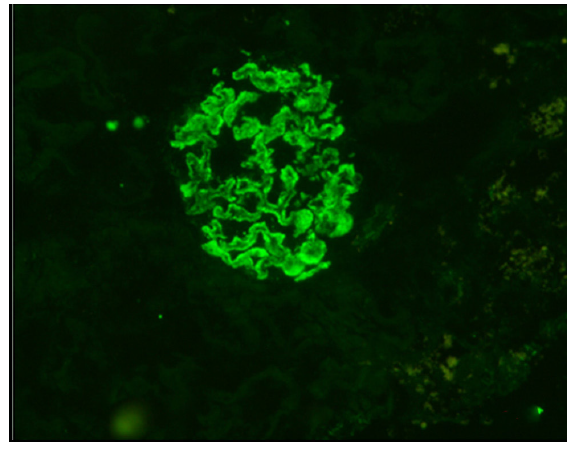
- C1q immunofluorescence positive in the glomeruli (intensity-2+).
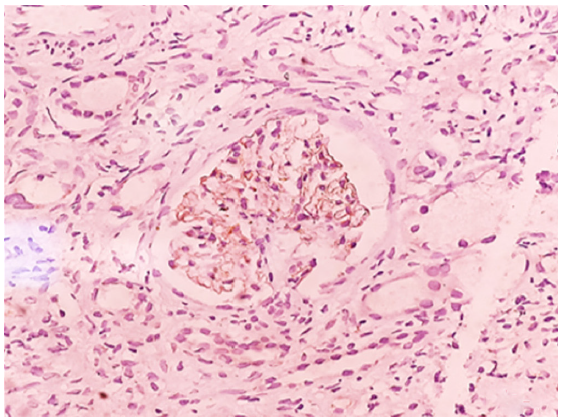
- NELL-1 immunohistochemistry positive in the glomeruli (intensity-3+), NELL-1: Nerve epidermal growth factor like protein.
All cases of MN associated with TIM showed complete remission. The average time of remission was found to be 3.8 months. Seventy percent of the cases were managed conservatively and steroids were given for 30% of the cases. The patients with severe disease, with lower GFR, low serum albumin, high proteinuria, and mercury levels, were given steroids and they responded well with similar median remission time. No chelating agents were used in our study.
Discussion
MN, which is considered to be the most common cause of adult nephrotic syndrome, has been classified as primary and secondary MN. While primary MN is considered to be idiopathic and associated with PLA2R antibodies, secondary MN is associated with secondary causes like connective tissue disorders, malignancies, and certain infections like Hepatitis B, Hepatitis C, and more.1
Several newer antigens have been associated with MN with the advent of laser microdissection and tandem mass spectrometry. Each of the newly discovered antigens is associated with an exclusive group of secondary causes of MN.
Among the newer antigens, NELL-1 is associated with malignancy, EXT1/2 has been associated with autoimmune disorders, Semaphorin 3B with pediatric MN, and so on. Some recent observations also found that a percentage of NELL-1 was not associated with any secondary causes and was deemed primary MN.9,10
Recent observations have found NELL-1 to be positive in MN associated with TIM. Among the TIM, the most common are mercury-containing compounds. In India, mercury therapy is followed in the Ayurveda, Unani, and Siddha systems of Indigenous medications. In Ayurveda, mercury is called “Rasa” because it slows the aging process.11
Eighty percent of the cases were females in our study, which was similar to the study on NELL-1 positive MN by Sethi et al.12 Among the ten cases associated with mercury intake, 50% of the cases were positive for NELL-1.
The compound associated with the five cases include Swaskalpa in 40% of cases, Rasagandhi Mezhugu in 40%, and Sudarshana Mezhugu in 20%. So, it can be said that NELL-1 is associated with mercury-associated MN.
The Siddha medicine “Rasagandhi Mezhugu” contains 1.04% of elemental mercury and mercuric chloride, which comes in 500 mg capsules. The average serum and urinary levels of mercury in our patients were found to be 38.4 ug/L and 39.2 ug/L, respectively.
These levels were found to be much higher than the permissible level of mercury in the body. The normal serum and urinary levels of mercury were < 11 ug/L and < 10 ug/L, respectively.13
It is rare to detect exposure to mercury in the general population, which can be hazardous only on a long-term exposure. The form of the mercuric compound is also vital to determine the toxicity profile whether it is elemental, mercurial salts, or it is inorganic mercury.13 Among the various forms of mercuric compounds, the inorganic form is found to be toxic to the kidney and the gut. The other two forms of the compound are found to cross the blood–brain barrier and cause neurotoxicity. Though all forms of mercury compounds lead to renal failure, it is the inorganic mercuric compounds that have drastic effects on the kidney.14
Acute exposure leads to acute tubular injury, whereas cases with chronic smaller dose exposure lead to chronic tubulointerstitial nephritis. The proximal tubules are the first to be exposed to mercuric compounds, which is the reason for tubulointerstitial nephritis.
Among the cases with TIM history, seven out of the ten cases (70%) showed a tubulointerstitial pattern of injury. All our cases belonged to cases with chronic exposure to Mercuric compounds.15,16
In addition to tubule-interstitial nephritis, chronic exposure to small doses can lead to glomerular damage presenting with nephrotic syndrome. The most common documented causes for nephrotic syndrome were MN and minimal change disease.17
In our study, all ten cases were mercury-induced MN; we were able to detect the source of mercury compounds in eight cases. In the remaining two cases, we were unable to detect a specific cause for the elevated mercury levels.
According to the literature, mercury-associated minimal change disease occurs by direct injury of the podocytes, whereas mercury-associated MN occurs due to a dysregulation in the immune function. There is an exuberant Th2 response which leads to T cell-mediated activation of B cells with IgG1 activation. This IgG1 may bind to the NELL-1 antigens expressed in the glomerular cells and transfer to the subepithelial side and activate the complement pathway and more IgG1 antibodies, thereby leading to immune complexes of MN.14
Additionally, the Hg-induced MN showed mesangial proliferation and are PLA2R and THSD7A negative distinguishing them from idiopathic MN. In our study, all the cases were negative for PLA2R and THSD7A, but only 30% of the cases showed additional mesangial proliferation.14,18,19
With regards to the direct immunofluorescence technique, IgG1 was positive in all the cases, whereas C1q was only positive in 20% of the cases. Other antibodies detected were IgA (20%) and IgM (20%). The possible reason for C1q negativity could not be explained.
NELL-1 is expressed in low levels in adult tissues, but is active during development where it is essential for intramembranous and endochondral ossification.20 NELL-1-associated MN is a specific subtype of MN which accounts for 16% of PLA2R-negative MN. NELL-1 was positive in 3.8% of the primary MN. Initially, NELL-1 was found to be associated with malignancy-associated MN which was found to be 33% in a study, whereas other studies have shown an association of 15% and 20%, respectively.21
In our study, there was one case that had a history of malignancy and also had a history of intake of mercury-containing TIM (10%). The next common association of NELL-1 was with TIM-containing mercury compounds. It was found that 87.9% of the mercury-related MN cases were associated with TIM, many of which contained mercury-related compounds. The exact percentage of cases directly associated with mercury-related MN was not mentioned in the study.22
In our study, 50% of the cases were positive for NELL-1, and one of the cases had an associated history of malignancy (10%). The exact reason for only a 50% positivity may be related to the chronicity and the serum levels of mercury which were found to be higher among the five positive cases. We can theoretically hypothesize that NELL-1 may serve as a susceptibility factor (second hit) for the development of MN in only a specific subset of patients taking TIM.22 This can explain the fact that only 50% of the cases were positive for NELL-1. In a recent review by Sethi et al., the association of NELL-1 with various secondary causes was discussed, and concluded that NELL-1 positivity may not point to a specific etiology and may be associated with a heterogeneous group of secondary causes.21
With regards to treatment, mercury-related nephropathy causes a state of inflammation and has autoimmune pathogenesis; steroids will help in a state of immunosuppression thereby halting the disease progression. More studies are needed to validate the use of steroids in mercury-associated nephropathies.23–24
The pros of this study are its novelty and the thorough workup available for all ten cases. Even in the comprehensive study by Kurien et al. on TIM-associated MN, only nine cases of mercury-associated MN had full comprehensive data for the cases.22
The main drawback of the study is the validation, as more studies may be needed and has to be done in various cohorts to disprove the association between NELL-1 and MN is not merely by chance. Serological correlation with NELL-1 was not done in our study.
Conclusion
NELL-1 which is a novel target antigen in MN especially in secondary causes of MN where it has to be demonstrated through Immunohistochemistry/Immunofluorescence technique as it helps the clinician to probe into the history of TIM intake or associated Malignancies. Thus, the clinician needs to take a thorough history of TIM intake as it is a reversible cause. It is also vital for the pathologist to pick up the subtle clues on histomorphology, Immunofluorescence (IgG1 dominant deposits), and Immunohistochemistry (NELL-1 positivity) for a definitive diagnosis of TIM-associated MN especially in cases where the history is not provided/ missed.
Conflicts of interest
There are no conflicts of interest.
References
- New ‘Antigens’ in membranous nephropathy. J Am Soc Nephrol. 2021;32:268-78.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Biochemical characterization and expression analysis of neural thrombospondin-1-like proteins NELL1 and NELL2. Biochem Biophys Res Commun. 1999;265:79-86.
- [CrossRef] [PubMed] [Google Scholar]
- Efficient production and characterization of recombinant human NELL1 protein in human embryonic kidney 293-F cells. Mol Biotechnol. 2012;51:58-66.
- [CrossRef] [PubMed] [Google Scholar]
- M-type phospholipase A2 receptor as target antigen in idiopathic membranous nephropathy. N Engl J Med. 2009;361:11-21.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Thrombospondin type-1 domain-containing 7A in idiopathic membranous nephropathy. N Engl J Med. 2014;371:2277-87.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Exostosin 1/exostosin 2-associated membranous nephropathy. J Am Soc Nephrol. 2019;30:1123-36.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Neural epidermal growth factor-like 1 protein (NELL-1) associated membranous nephropathy. Kidney Int. 2020;97:163-74.
- [CrossRef] [PubMed] [Google Scholar]
- NELL1 is a target antigen in malignancy-associated membranous nephropathy [published online ahead of print August 20, 2020] Kidney Int 10.1016/j.kint.2020.07.039
- [Google Scholar]
- Neural epidermal growth factor-like 1 protein (NELL-1) associated membranous nephropathy. Kidney Int. 2020;97:163-74.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of neural epidermal growth factor-like 1- and exostosin 1/exostosin 2- associated membranous nephropathy: a single-center retrospective study in Japan. Sci Rep. 2022;12:2967.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Mercury and mercury-containing preparations: History of use, clinical applications, pharmacology, toxicology, and pharmacokinetics in traditional chinese medicine. Front Pharmacol. 2022;13:807807.
- [CrossRef] [PubMed] [Google Scholar]
- Neural epidermal growth factor-like 1 protein (NELL-1) associated membranous nephropathy. Kidney Int. 2020;97:163-74.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic kidney disease and exposure to nephrotoxic metals. Int J Mol Sci. 2017;18:1039.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- What can mercury teach us about membranous nephropathy and minimal change disease? Kidney Int Rep. 2022;7:1157-60.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Unveiling the features of mercury-associated minimal change disease: Comparison with primary minimal change disease. Kidney Dis (Basel). 2021;7:156-65.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Toxic nephropathy secondary to chronic mercury poisoning: clinical characteristics and outcomes. Kidney Int Rep. 2022;7:1189-97.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Mercury-associated glomerulonephritis:A retrospective study of 35 cases in a single Chinese center. BMC Nephrol. 2019;20:228.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Mercury induced membranous nephropathy: clinical and pathological features. Clin J Am Soc Nephrol. 2010;5:439-44.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Lipoic acid supplementation associated with neural epidermal growth factor-like 1 (NELL1)-associated membranous nephropathy. Kidney Int. 2021;100:1208-13.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The role of NELL-1, a growth factor associated with craniosynostosis, in promoting bone regeneration. J Dent Res. 2010;89:865-78.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The many faces of NELL1 MN. Clin Kidney J. 2022;16:442-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Traditional indigenous medicines are an etiologic consideration for NELL1-positive membranous nephropathy. Kidney Int. 2022;102:1424-6.
- [CrossRef] [PubMed] [Google Scholar]
- Neural epidermal growth factor-like 1 protein-positive membranous nephropathy in Chinese patients. Clinical Journal of the American Society of Nephrology (CJASN). 2021;16:727.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Mercury-induced membranous nephropathy: Clinical and pathological features. Clin J Am Soc Nephrol. 2010;5:439-44.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]








