Translate this page into:
Neutrophil Gelatinase–Associated Lipocalin as a Marker for Contrast-Induced Nephropathy in Patients Undergoing Percutaneous Coronary Intervention: A Prospective Observational Analysis
Address for correspondence: Dr. Ankit Kumar Sahu, Department of Cardiology, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, Uttar Pradesh - 226 014, India. E-mail: ankitsahu.md@gmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Incidence of contrast-induced nephropathy (CIN) post percutaneous coronary intervention (PCI) varies between 5% and 20%. Neutrophil gelatinase–associated lipocalin (NGAL) is a sensitive marker for acute kidney injury. Data regarding the predictive accuracy of NGAL in Indian patients undergoing PCI is sparse.
Methods:
A total of 212 consecutive “all-comer” patients, undergoing PCI from March 2015 to April 2016 were recruited in this single-center observational study. Plasma NGAL levels were measured at 4 hours post PCI using commercially available enzyme-linked immunosorbent assay (Triage® Alere™, San Diego, CA, USA).
Results:
Twenty-five (11.8%) patients developed CIN. The 4-hour post-PCI plasma NGAL levels were significantly higher in patients with CIN than without (400.6 ± 269.3 ng/mL vs. 109.8 ± 68.0 ng/mL, P < 0.0001). Patients developing CIN had higher age, low estimated glomerular filtration rate (eGFR), and higher contrast volume usage during PCI. After adjusting for confounding factors, diabetes mellitus (adjusted odds ratio [AOR] 3.04; P = 0.039; 95% confidence interval [CI]: 1.06–8.73), hypotension at presentation (AOR 24.84; P < 0.0001; 95% CI: 4.65–132.83), and multi-staged PCI (AOR 13.45; P < 0.0001; 95% CI: 4.54–39.79) were found to independently predict the development of CIN. NGAL levels significantly correlated with age (r = 0.149, P = 0.031), eGFR (r = −0.385, P < 0.0001), hemoglobin (r = −0.214, P = 0.002), contrast volume (r = 0.185, P = 0.007), and 48-hour post-PCI serum creatinine levels (r = 0.334, P < 0.0001). At a cutoff of 256.5 ng/mL, plasma NGAL had a sensitivity of 68% and a specificity of 95.2% (area under the curve = 0.878; P < 0.0001; 95% CI: 0.801–0.955) to predict the occurrence of CIN.
Conclusions:
Plasma NGAL is an early and highly predictive biomarker of CIN in patients undergoing PCI. Patients having diabetes, hypotension at presentation and those undergoing second-stage procedures are at a high risk of developing CIN after PCI.
Keywords
Acute kidney injury
contrast-induced nephropathy
neutrophil gelatinase–associated lipocalin
percutaneous coronary intervention
Introduction
Contrast-induced nephropathy (CIN) after renal hypoperfusion and drug-induced nephrotoxicity, is the third most common cause of hospital-acquired acute kidney injury (AKI) accounting for 11% of AKI.[1] The incidence of CIN following percutaneous coronary intervention (PCI) depends on the definition of CIN used, the study population, and the risk factors predisposing to CIN. Although in patients undergoing PCI, CIN is not uncommon (incidence of 5%–20%) yet CIN leading to dialysis is rare (0.5%–2.0%). However, patients requiring dialysis have high mortality (35.7%) with a 2-year survival rate of only 19%.[2]
Conventionally, creatinine, which is a marker of renal function rather than renal injury and is presently the gold standard for defining CIN, has been an insensitive biomarker and more often late to detect acute changes in kidney function. Emerging technologies such as functional genomics and proteomics have uncovered novel candidates in the form of biomarkers that can facilitate timely effective renal protection strategies and ultimately have a positive impact on long-term outcomes for patients with CIN.[34] Among the top candidate biomarkers for contrast-induced AKI at present are neutrophil gelatinase–associated lipocalin (NGAL),[5] interleukin 18 (IL-18),[6] kidney injury molecule-1 (KIM-1),[7] urinary liver-type fatty acid–binding protein (L-FABP),[8] cystatin C,[9] N-acetyl-(D) glucosaminidase (NAG).[10]
We, therefore, aimed to assess the incidence of CIN in our patient subset undergoing PCI, identify the factors predictive of CIN in this group of patients, and additionally assess the predictive cutoff value of early plasma NGAL levels in detecting the occurrence of CIN downstream during the hospitalization.
Materials and Methods
Study population
A total of 212 consecutive “all-comer” patients undergoing PCI at our institute between March 2015 and April 2016 were included in this single-center, prospective, observational study. The decision to perform PCI was made at the discretion of the operating cardiologist on the basis of the patient's clinical profile, lesion characteristics, and patient preference. Written informed consent was obtained prior to the procedure in all patients as per institution protocol. All data related to the procedure including the patient's clinical presentation and follow-up were retrieved from computerized database software where all such records were maintained with yearly follow-up information. Incomplete records were refurbished using telephonic contact with the patients. The approval of the institutional ethics committee was obtained as a protocol. Patients who had undergone coronary artery bypass surgery (CABG) within the past 1 month and those having an active infection, malignancy, and chronic inflammatory states were excluded from the study.
Procedure protocol
All patients were pretreated with aspirin and loaded with clopidogrel 600 mg or ticagrelor 180 mg or prasugrel 60 mg depending on the patient's clinical profile and contraindications, if any. Unfractionated heparin was given at the time of procedure and titrated to maintain activated clotting time (ACT) >250 seconds. Intravenous antiplatelet agents (glycoprotein IIb/IIIa inhibitors) were given at the discretion of the operator depending on the complexity of the lesion, length of the stent contemplated, the use of multiple stents, and the patient's clinical status. Post-procedure, all patients were prescribed dual antiplatelet drugs for at least 1 year. Other cardioactive medications were prescribed in accordance with the patient's clinical need and guidelines recommendation. Complete revascularization was aimed in all patients except in those who presented with acute ST elevation MI (STEMI) in whom only the culprit lesion was done at first go and significant non-culprit lesions were usually revascularized later in a staged procedure mostly in the same hospital admission.
Evaluation tools
During the hospital stay, all clinical details of the patient were captured on a pro forma and included various patient- and procedure-related risk factors for CIN, namely, diabetic status, age, estimated glomerular filtration rate (eGFR; Cockcroft–Gault formula), hypertension, preexisting renal dysfunction, congestive heart failure, post–renal transplant, primary PCI, anemia, preprocedural hemodynamic instability, volume, osmolality and ionicity of contrast used, use of intra-aortic balloon pump, and multiple administration of contrast within 72 hours. An echocardiogram was done to evaluate the baseline left ventricular (LV) function. Venous blood samples were collected on admission in the coronary care unit or emergency department before PCI, which were used for the evaluation of basal biochemical and hematological parameters. Venous blood measuring 2 mL was collected in EDTA (ethylenediaminetetraacetic acid) vials for the measurement of plasma NGAL and serum creatinine levels at 4 hours and 48 hours after PCI, respectively.
Jaffe's colorimetric assay was employed by an automated clinical chemistry analyzer (RX imola, Randox laboratories limited, UK) to estimate serum creatinine levels. However, the standardization of creatinine calibration was not traceable to isotope dilution mass spectrometry. NGAL was evaluated using commercially available enzyme-linked immunosorbent assay (Triage® Alere™ NGAL test, San Diego, CA, USA).
Definitions
Contrast-induced nephropathy
Impairment in renal function denoted by an increase in serum creatinine by >0.5 mg/dL or >25%, assessed at 48 hours after the procedure after intravascular administration of contrast medium, without an alternative etiology in accordance with the European Society of Urogenital Radiology diagnostic criteria for CIN.[11]
Statistical analysis
Continuous variables were expressed as mean ± standard deviation, and categorical variables were expressed as percentages. P values ≤0.05 were considered significant. Descriptive analysis was used to assess the distribution of data. A multiple logistic regression model was created to isolate the statistically significant risk predictors associated with CIN. A Chi-square test was used to compare the risk factor profile between the group of patients having high plasma NGAL levels or not. A cutoff was derived using the receiver operating characteristic curve distribution of NGAL values in different patients with or without CIN, and the Youden index was calculated.[12] Youden index is defined as (sensitivity + specificity) -1. The best cutoff was taken as the highest Youden index. Statistical analysis was done using the IBM SPSS Statistical Software (IBM SPSS Statistics Version 20.0, IBM SPSS, USA).
Results
The baseline demographic and clinical profile of the entire study group stratified into those developing CIN or not is shown in Table 1. A total of 212 patients were included in the study, out of which 25 (11.8%) patients developed CIN post-PCI. Patients developing CIN were elder to those who did not develop CIN (65.2 ± 11.5 vs. 57.4 ± 9.5 years; P < 0.001). Three fourths of the patients belonged to the 50–75 years age bracket. One fourth of the patients had diabetes (n = 59, 27.8%), and hypertension was present in half (n = 106, 50%). Only eight (3.78%) patients had preexisting renal dysfunction. Two patients were on renal replacement therapy, whereas none had a prior renal transplant. In-hospital mortality for post-PCI patients was 2.4% (n = 5).
| Variable | Total cohort (n=212) | CIN | P | |
|---|---|---|---|---|
| Yes (n=25) | No (n=187) | |||
| Age in years, mean (SD) | 58.3±10.1 | 65.2±11.5 | 57.4±9.5 | <0.001* |
| ≤50, n (%) | 41 (19.3) | 6 (24.0) | 35 (18.7) | |
| 51-74, n (%) | 157 (74.1) | 16 (64.0) | 141 (75.4) | 0.38 |
| ≥75, n (%) | 14 (6.6) | 3 (12.0) | 11 (5.9) | |
| Sex, n (%) | ||||
| Male | 182 (85.8) | 22 (88.0) | 160 (85.5) | 0.74 |
| Female | 30 (14.2) | 3 (12.0) | 27 (14.5) | |
| Diabetes, n (%) | 59 (27.8) | 15 (60.0) | 44 (23.5) | <0.001* |
| Hypertension, n (%) | 106 (50.0) | 11 (44.0) | 95 (50.8) | 0.52 |
| LVEF, mean±SD | 46.4±7.7 | 46.7±6.0 | 46.4±7.9 | 0.86 |
| CHF, n (%) | 3 (1.4) | 2 (8.0) | 1 (0.5) | 0.003* |
| LV dysfunction, n (%) | 89 (42.0) | 12 (48.0) | 77 (41.2) | 0.51 |
| Mild | 41 (19.3) | 8 (32.0) | 33 (17.6) | |
| Moderate | 34 (16.0) | 4 (14.0) | 30 (16.0) | 0.23 |
| Severe | 13 (6.1) | 0 (0) | 13 (7.6) | |
| Mode of presentation, n (%) | 84 (39.6) | 9 (36.0) | 75 (35.4) | |
| STEMI | 25 (11.8) | 5 (20.0) | 20 (9.4) | 0.42 |
| NSTEMI | 17 (8.0) | 3 (12.0) | 14 (7.5) | |
| Unstable angina | 86 (40.6) | 8 (32.0) | 78 (41.7) | |
| Primary PCI, n (%) | 23 (10.9) | 1 (4.0) | 22 (11.8) | 0.24 |
| Anemia, n (%) | 57 (23.6) | 7 (28.0) | 50 (26.7) | 0.89 |
| Hypotension, n (%) | 10 (4.7) | 7 (28.0) | 3 (1.6) | <0.001* |
| Prior renal dysfunction, n (%) | 8 (3.8) | 3 (12.0) | 5 (2.7) | 0.02* |
| Iso-osmolar contrast use, n (%) | 93 (43.9) | 13 (52.0) | 80 (42.8) | 0.38 |
| Low-osmolar contrast use, n (%) | 119 (56.1) | 12 (48.0) | 107 (57.2) | |
| Iomeprol | 47 (22.1) | 3 (12.0) | 44 (23.5) | 0.41 |
| Iopromide | 72 (34.0) | 9 (36.0) | 63 (33.7) | |
| Baseline creatinine, mg/dl | 1.20±0.42 | 1.13±0.71 | 1.20±0.37 | 0.39 |
| Hemoglobin, g/dl | 12.8±1.90 | 12.3±2.06 | 12.9±1.88 | 0.15 |
| Staged PCI procedure, n (%) | 31 (14.6) | 15 (60.0) | 16 (8.5) | <0.001* |
| eGFR in mL/min/m2, n (%) | ||||
| ≤30 | 5 (2.4) | 2 (8.0) | 3 (1.6) | |
| 31-59 | 55 (25.9) | 19 (76.0) | 36 (19.3) | <0.001* |
| 60-89 | 105 (49.5) | 4 (16.0) | 101 (54.0) | |
| ≥90 | 47 (22.2) | 0 (0) | 47 (25.1) | |
| eGFR in mL/min/m2 (mean±SD) | 71.0±21.4 | 49.3±13.9 | 74.6±19.7 | <0.001* |
| Volume of contrast used in mL, n (%) | ||||
| ≤200 | 86 (40.6) | 15 (60.0) | 71 (38.1) | 0.05 |
| 201-399 | 116 (54.7) | 8 (32.0) | 108 (57.6) | |
| ≥400 | 10 (4.7) | 2 (8.0) | 8 (4.3) | |
| Volume of contrast in mL (mean±SD) | 263.7±83.2 | 326.4±132.9 | 255.4±70.6 | <0.001* |
| In-hospital mortality, n (%) | 5 (2.4) | 2 (8.0) | 3 (1.6) | 0.048* |
| Need for in-hospital RRT, n (%) | 2 (0.9) | 1 (4.0) | 1 (0.5) | 0.092 |
SD=standard deviation; CIN=contrast-induced nephropathy; LVEF=left ventricular ejection fraction; CHF=congestive heart failure; LV=left ventricular; STEMI=ST elevation myocardial infarction; NSTEMI=non-ST elevation myocardial infarction; CAD=coronary artery disease; eGFR=estimated glomerular filtration rate (by Cockcroft-Gault method); PCI=percutaneous coronary intervention; RRT=renal replacement therapy. *Significant P values
Baseline characteristics
About 60% of the patients in the CIN group had diabetes compared with 23.5% in the non-CIN group (P < 0.001). Significantly, more patients in the CIN group presented with clinical heart failure (8% vs. 0.53%; P = 0.003) and had hypotension at presentation (28% vs. 1.6%; P < 0.001) when compared with the non-CIN group. LV dysfunction and anemia were present in 42% and 23.6% of patients, respectively, at baseline, which was not different in the two groups. Primary PCI was done in 10.85% (n = 23) of patients, out of which only one patient developed CIN. Pre-existing renal dysfunction was present in eight (3.77%) patients, out of which three had worsening of renal function post-procedure, which was significantly more as compared with the non-CIN group (P = 0.02). The mean baseline eGFR was 71.0 ± 21.4 mL/min/m2 with patients in the CIN group having significantly lower eGFR compared with the non-CIN group (49.28 ± 13.94 vs. 74.59 ± 19.67 mL/min/m2; P < 0.001). Iso-osmolar and low-osmolar contrast was used in 43.9% (n = 93) and 56.1% (n = 119), respectively. The mean contrast volume used per patient in the study was 263.7 ± 83.2 mL, with patients in the CIN group having significantly higher contrast volume compared with those in the non-CIN group (326.4 ± 132.9 vs. 255.4 ± 70.6 mL; P < 0.001). About 60% (n = 15) of the patients in CIN group underwent staged procedure as compared to 8.5% (n = 16) in the non-CIN group (P < 0.001). The time interval between the staged procedures was not assessed separately.
Outcomes in diabetic patients
Baseline creatinine (1.31 ± 0.62 vs. 1.15 ± 0.30 mg%; P = 0.01), volume of contrast used per patient (286.8 ± 93.7 vs. 254.9 ± 77.3 mL; P = 0.01) and 48-hour post-PCI creatinine (1.29 ± 0.69 vs. 1.07 ± 0.31 mg%; P = 0.002) were significantly higher in diabetics. The basal hemoglobin (11.96 ± 2.11 vs, 13.11 ± 1.72 g%; P < 0.001) and eGFR (64.62 ± 24.31 vs. 73.49 ± 19.74 mL/min/m2; P = 0.007) were significantly lower in diabetic patients compared with nondiabetics. Despite being nonsignificant, the 4-hour post-PCI NGAL levels were higher in diabetics when compared with nondiabetics [Table 2].
| Variable | Diabetic (n=59) | Nondiabetic (n=153) | P |
|---|---|---|---|
| Age, years | 60.32±10.13 | 57.58±9.97 | 0.08 |
| Baseline creatinine, mg/dl | 1.31±0.62 | 1.15±0.30 | 0.01* |
| eGFR, mL/min/m2 | 64.62±24.31 | 73.49±19.74 | 0.007* |
| LVEF, % | 46.86±5.94 | 46.25±8.29 | 0.61 |
| Hemoglobin, G/dl | 11.96±2.11 | 13.11±1.72 | <0.001* |
| Volume of contrast, mL | 286.78±93.74 | 254.85±77.32 | 0.01* |
| 48-hour post-PCI creatinine, mg/dl | 1.29±0.69 | 1.07±0.31 | 0.002* |
| 4-hour post-PCI plasma NGAL, ng/mL | 167.81±180.45 | 134.95±129.08 | 0.14 |
| CIN, n (%) | 15 (25.4) | 10 (6.5) | <0.001* |
NGAL=neutrophil gelatinase-associated lipocalin; CIN=contrast-induced nephropathy; LVEF=left ventricular ejection fraction; eGFR=estimated glomerular filtration rate (by Cockcroft-Gault method); PCI=percutaneous coronary intervention. *Significant P values
Post-procedural markers of CIN
Figure 1 shows the pre-PCI and post-PCI trends of the two markers of CIN, namely, serum creatinine and plasma NGAL. The overall mean 48-hour postprocedural serum creatinine level was 1.13 ± 0.46 mg/dl, being significantly high among patients with CIN as compared with those in the non-CIN group (1.48 ± 0.91 vs. 1.08 ± 0.34 mg/dl; P < 0.001). Also, the mean (geometric) plasma NGAL level measured 4-hour post-PCI was 144.1 ± 145.5 ng/mL (range 18–936 ng/mL) with significantly higher levels in the CIN group as compared with the non-CIN group (400.6 ± 269.3 vs. 109.8 ± 68.0 ng/mL; P < 0.001). The plasma NGAL levels followed a skewed non-Gaussian type of distribution pattern.
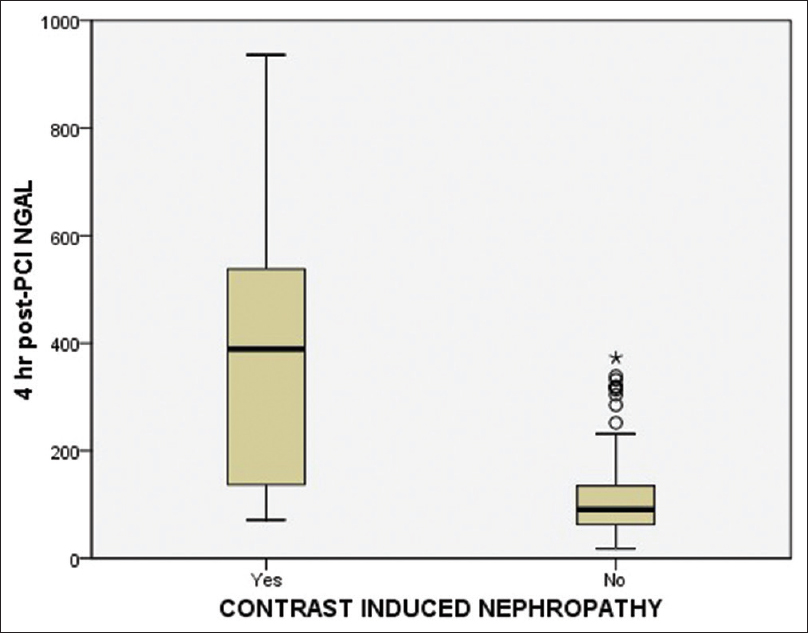
- Box plot showing distribution of 4-hour post-PCI NGAL levels in patients with and without CIN
Predictors of CIN
After adjustment for confounding risk factors by multivariate linear regression analysis, diabetes mellitus (adjusted odds ratio [AOR] 3.04; P = 0.039; 95% confidence interval [CI]: 1.06–8.73), hypotension at presentation (AOR 24.84; P < 0.0001; 95% CI: 4.65–132.83), and second-stage PCI (AOR 13.45; P < 0.0001; 95% CI: 4.54–39.79) were found to independently predict the development of CIN [Table 3]. No significant difference in plasma NGAL was observed between patients administered iso-osmolar and low-osmolar contrast media (P = 0.556).
| Variable | HR (95% CI) | P |
|---|---|---|
| Diabetes | 3.04 (1.06-8.73) | 0.039* |
| Hypotension at presentation | 24.84 (4.65-132.83) | <0.0001* |
| Staged PCI procedure | 13.45 (4.54-39.79) | <0.0001* |
| Prior renal dysfunction | 3.58 (0.48-26.92) | 0.216 |
| CHF at presentation | 6.55 (0.12-346.34) | 0.353 |
| Contrast volume | 1.02 (0.99-1.04) | 0.205 |
| Age | 1.86 (0.74-4.64) | 0.185 |
| eGFR | 0.83 (0.63-1.08) | 0.165 |
CIN=contrast-induced nephropathy; PCI=percutaneous coronary intervention; CHF=congestive heart failure; HR=hazard ratio; CI=confidence interval, eGFR=estimated glomerular filtration rate. *Significant P values
Predictive accuracy of NGAL for CIN
At a cutoff of 256.5 ng/mL for 4-hour post-PCI plasma NGAL levels, the sensitivity was 68% and the specificity was 95.2% (area under the curve [AUC] = 0.878; P < 0.0001, 95% CI: 0.801–0.955) as shown in Figure 2.
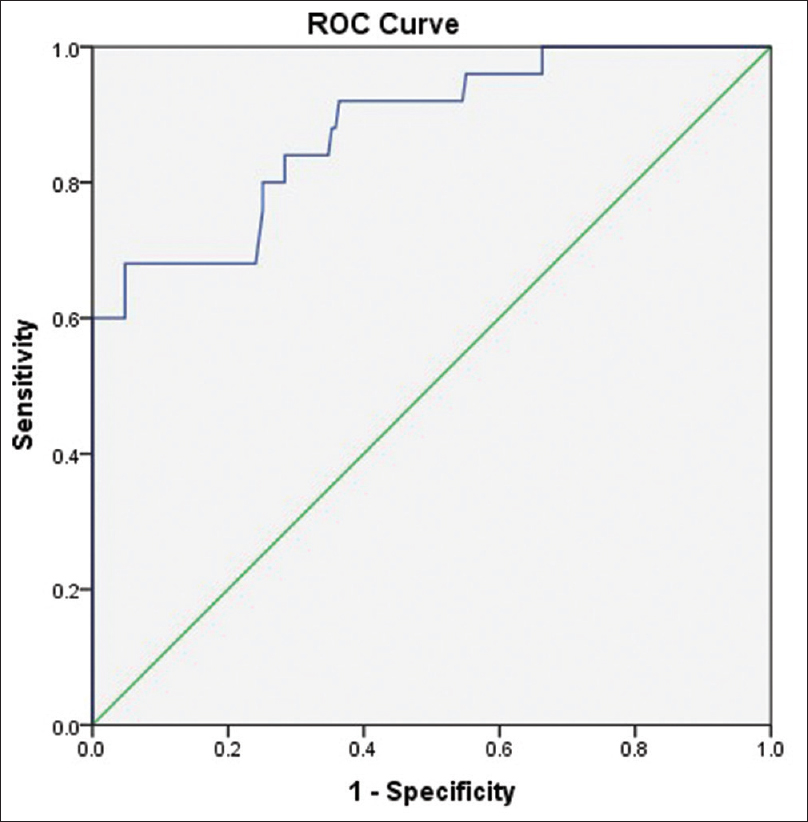
- Receiver-operated characteristics curve depicting sensitivity and specificity of 4-hour post-PCI NGAL levels for predicting CIN
Correlation of NGAL with other risk factors for CIN
The NGAL levels significantly correlated with age (r = 0.149, P = 0.031), eGFR (r = −0.385, P < 0.0001), hemoglobin (r = −0.214, P = 0.002), volume of contrast used (r = 0.185, P = 0.007), and 48-hour post-PCI serum creatinine levels (r = 0.334, P < 0.0001) as shown in Figure 3.
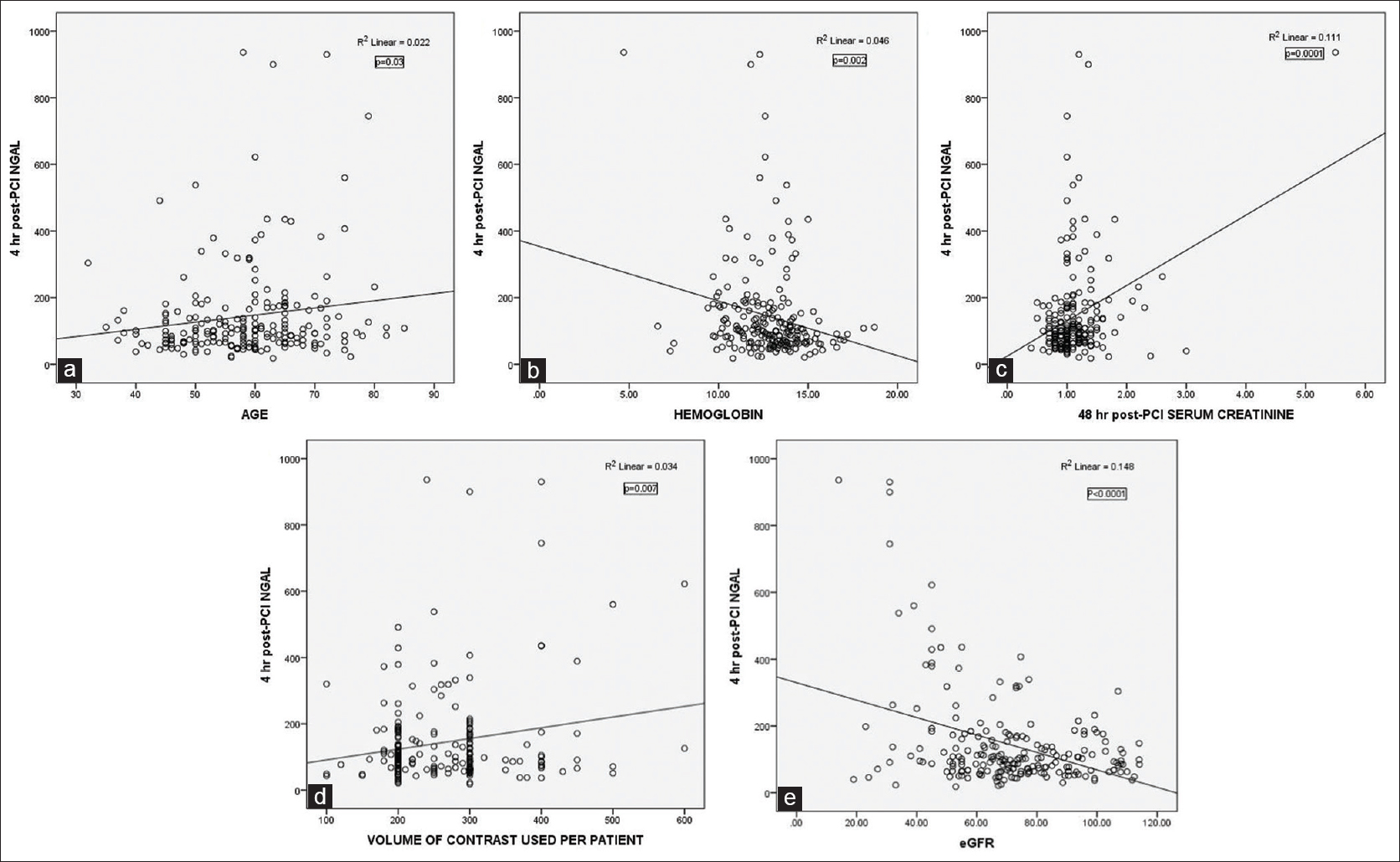
- Plot showing correlation of 4-hour plasma NGAL level with age (Panel a), hemoglobin (Panel b), serum creatinine (Panel c), volume of contrast used (Panel d), and eGFR values (Panel e)
Discussion
Our study provides a single-center experience of employing a novel biomarker for early recognition and prediction of contrast-induced AKI in patients undergoing PCI. The incidence of CIN in our study was 11.8%, whereas in various other studies, it is reported to vary between 5% and 20%.[2] Here, it is imperative to clarify that although multiple definitions using varying serum creatinine thresholds exist for defining contrast-induced nephropathy (e.g. ESUR (European Society of Urogenital Radiology) criteria,[11] KDIGO (Kidney Disease: Improving Global Outcomes) working group criteria,[13] AKIN (Acute Kidney Injury Network) criteria,[14] RIFLE (Risk, Injury, Failure, Loss of Function, End-Stage) classification,[15] ACR (American College of Radiology) criteria,[16] yet ultimately all definitions of contrast-induced AKI are arbitrary, not specific to contrast-induced injury and based only on laboratory testing. Employing the criterion of a smaller rise in serum creatinine may lower the threshold for diagnosing CIN, thereby increasing the incidence of contrast nephropathy especially after coronary interventions. Nevertheless, to standardize the definition of CIN, recently in 2020 ACR in association with NKF (National Kidney Foundation) has proposed to use AKIN criteria for diagnostic purposes.[17]
Renal medullary ischemia[181920] arising from an imbalance of local vasoconstrictive and vasodilatory influences[212223] and direct cytotoxicity[2425] coupled with increased demand for oxygen-driven sodium transport[2627] may be the key to CIN pathogenesis. Another important observation of our study was the identification of risk factors that independently predict the development of CIN, namely, diabetes, hemodynamic instability at presentation, and multi-staged procedures. In fact, our study projected the incidence of CIN in 25.4% of diabetic and 6.5% of nondiabetic patients in contrast to previously reported incidence of 20% and 13% in diabetics and nondiabetics, respectively.[2829]
NGAL is an emerging biomarker of renal injury applicable in a whole gamut of conditions such as immunoglobulin A (IgA) nephropathy,[30] posttransplant graft dysfunction,[31] childhood-onset systemic lupus erythematosus (SLE),[32] post–cardiovascular surgery[33] and following contrast exposure during angiography.[123435] It is also upregulated in other pathological conditions such as inflammatory bowel disease, neoplasms, preeclampsia, pancreatitis, arthritis, heart failure, and autoimmune myocarditis.[36373839404142] Inflammation via C-reactive protein and neutrophil leukocyte esterase infiltrating the atherosclerotic plaque plays a role in the pathogenesis of atherosclerosis and plaque instability thereby explaining the increased expression of NGAL in the setting of acute coronary syndrome (ACS).[4344] Similarly, post-PCI disruption and mechanical alteration of atherosclerotic plaque provide for the basis of raised NGAL in this setting.[4546]
In several prospective cohort studies, urine and plasma NGAL levels have been shown to rise within 1 to 2 hours after the onset of AKI, whereas the rise in serum creatinine is not detected until 1 to 2 days later. It has been shown by Tuldhar et al. that plasma and urinary NGAL measured as early as 2 hours after cardiopulmonary bypass can predict the increased risk of developing AKI in pediatric and adult cardiac surgery patients.[47] An earlier rise in serum levels may be due to the fact that NGAL is released into the circulation probably secondary to inflammation activation of neutrophils initiated by the contrast agent. Studies done in patients having stable angina, unstable angina,[46] and chronic kidney disease,[48] and undergoing PCI[49] or coronary angiography[50] demonstrate good predictability of CIN by estimation of serum or urinary NGAL levels. In our study, using the Youden index, the best cutoff value for plasma NGAL to predict AKI was estimated to be 256.5 ng/mL, with 68% sensitivity and 95.2% specificity. Padhy et al. also demonstrated that a plasma NGAL cutoff level of 155.2 ng/mL predicted an early development of CIN in patients undergoing PCI.[49] Similar findings in other small observational studies supplement our data to establish NGAL as an excellent predictor of CIN.[51] Bachorzewska-Gajewska et al. found plasma NGAL to predict CIN after PCI with a sensitivity of 90% and a specificity of 76% in patients with stable angina.[464952] In a prospective study involving the pediatric population undergoing elective cardiac catheterization, both urinary and plasma NGAL predicted CIN.[53] Using a cutoff value of 100 ng/mL, the prediction of CIN was excellent for 2-hour plasma NGAL (AUC 0.91, sensitivity 90%, specificity 74%) and 4-hour urinary NGAL (AUC 0.92, sensitivity 76%, specificity 80%).[52]
Variability in the predictive values of NGAL for CIN in different studies may be attributed to the difference in selection criteria, the age of patients (pediatric or adult population), the type of coronary artery disease (CAD) presentation (ACS, stable CAD), the mode of coronary intervention (diagnostic angiography, PCI, or CABG), the method of NGAL estimation (plasma or urine), the time frame for obtaining samples (early <4 hours or delayed >4 hours from intervention), and the mechanism of myocardial injury (ischemic or nonischemic heart failure). In various studies, the NGAL levels were shown to correlate with serum creatinine levels, duration of the procedure, hemoglobin A1c (HbA1c) levels, hematocrit, hemoglobin, hypertension, age, and presence of diabetes. In our study, the NGAL levels correlated positively with age, the volume of contrast agent, and postprocedural creatinine, whereas it negatively correlated with eGFR and hemoglobin. As our patient population had a diverse composition in terms of clinical presentation due to an “all-comer” design, our data inferences can be applied to a wider range of the patient population. Diabetic patients were especially found to be at increased risk for CIN as they were elderly, had increased baseline creatinine and volume of contrast used, and had low hemoglobin and eGFR as compared with nondiabetic patients. Recent data have demonstrated that in patients with LV dysfunction, NGAL is a strong predictor of 30-day rehospitalization due to heart failure and all-cause mortality.[54] Contrary to the above view, LV dysfunction and hypertension in our study were not predictors of CIN, probably because of the uniform distribution of patients with varying LV function and hypertensive status in both groups.
Limitations of the study
We do feel that our study has a few limitations. This was a single-center experience with an observational study design. Although the present study demonstrates an independent prognostic value of NGAL in CAD patients, yet a causal relationship cannot be extrapolated. Therefore, investigation of the sources and specific molecular forms of NGAL is warranted. Furthermore, urinary NGAL levels estimation could have been helpful for making a true assessment of AKI. Our study group was heterogeneous with all types of CAD patients being included. Variability of plasma NGAL measurement in patients with chronic comorbidities represents an important limitation to widespread clinical application.
Conclusion
Of all patients undergoing PCI, one tenth are prone to develop CIN with diabetic patients, those having hypotension at presentation, and those undergoing multi-stage procedures during the index hospitalization being at the highest risk of contrast nephropathy. A 4-hour plasma NGAL of 256.5 ng/mL or above predicts the occurrence of CIN in patients undergoing PCI with a sensitivity of 68% and a specificity of 95.2%.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We acknowledge the contribution of Mr. Mritunjay Mishra, Research Assistant in the department of cardiology, SGPGIMS, for data collection, telephonic follow-ups, and documentation of records and Dr. Prabhakar Mishra, in the department of medical biostatistics, SGPGIMS, for helping with project data analysis.
References
- Proteomics for biomarker discovery in acute kidney injury. Semin Nephrol. 2007;27:637-51.
- [Google Scholar]
- Identification of neutrophil gelatinase-associated lipocalin as a novel early urinary biomarker for ischemic renal injury. J Am Soc Nephrol. 2003;14:2534-43.
- [Google Scholar]
- Urinary IL-18 is an early predictive biomarker of acute kidney injury after cardiac surgery. Kidney Int. 2006;70:199-203.
- [Google Scholar]
- Kidney Injury Molecule-1 (KIM-1): A novel biomarker for human renal proximal tubule injury. Kidney Int. 2002;62:237-44.
- [Google Scholar]
- Valuable markers for contrast-induced nephropathy in patients undergoing cardiac catheterization. Circ J. 2008;72:1499-505.
- [Google Scholar]
- Comparison of serum creatinine and cystatin C for early diagnosis of contrast-induced nephropathy after coronary angiography and interventions. Clin Chem. 2012;58:458-64.
- [Google Scholar]
- Urinary biomarkers in the early diagnosis of acute kidney injury. Kidney Int. 2008;73:863-9.
- [Google Scholar]
- Guidelines for contrast media from the European Society of Urogenital Radiology. AJR Am J Roentgenol. 2003;181:1463-71.
- [Google Scholar]
- Neutrophil gelatinase- associated lipocalin and renal function after percutaneous coronary interventions. Am J Nephrol. 2006;26:287-92.
- [Google Scholar]
- Kidney disease: Improving Global Outcomes. KDIGO clinical practice guideline for acute kidney injury. Kidney Int. 2012;2:1-138.
- [Google Scholar]
- Acute Kidney Injury Network: Report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007;11:R31.
- [Google Scholar]
- Acute renal failure-definition, outcome measures, animal models, fluid therapy and information technology needs: The Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004;8:R204-12.
- [Google Scholar]
- ACR Committee on Drugs, “Manual on Contrast Media, Version 9,”. 2013. Available from: http://www.acr.org/ Quality-Safety/Resources/Contrast-Manual
- [Google Scholar]
- Use of intravenous iodinated contrast media in patients with kidney disease: Consensus statements from the American College of Radiology and the National Kidney Foundation. Radiology. 2020;294:660-8.
- [Google Scholar]
- Rapid DNA fragmentation from hypoxia along the thick ascending limb of rat kidneys. Kidney Int. 1995;47:1806-10.
- [Google Scholar]
- Radiocontrast-induced renal tubular cell apoptosis: Hypertonic versus oxidative stress. Invest Radiol. 2002;37:428-34.
- [Google Scholar]
- Adenosine and extracellular volume in radiocontrast media-induced nephropathy. Kidney Int Suppl. 1998;67:S192-4.
- [Google Scholar]
- The selective adenosine A1 receptor antagonist KW-3902 prevents radiocontrast media-induced nephropathy in rats with chronic nitric oxide deficiency. Eur J Pharmacol. 2001;414:99-104.
- [Google Scholar]
- Effects of contrast media and mannitol on renal medullary blood flow and red cell aggregation in the rat kidney. Kidney Int. 1996;49:1268-75.
- [Google Scholar]
- Effects of contrast media on renal microcirculation and oxygen tension. An experimental study in the rat. Acta Radiol Suppl. 1997;409:1-29.
- [Google Scholar]
- Effects of high- and low-osmolar contrast media on renal plasma flow and glomerular filtration rate in euvolemic and dehydrated rats. A comparison between ioxithalamate, iopamidol, iohexol and ioxaglate. Acta Radiol. 1989;30:383-9.
- [Google Scholar]
- Constriction of the vasa recta, the vessels supplying the area at risk for acute kidney injury, by four different iodinated contrast media, evaluating ionic, nonionic, monomeric and dimeric agents. Invest Radiol. 2010;45:453-7.
- [Google Scholar]
- Hypoperfusion in the renal outer medulla after injection of contrast media in rats. Acta Radiol. 1999;40:521-7.
- [Google Scholar]
- Acute hyperglycemia and contrast-induced nephropathy in primary percutaneous coronary intervention. Am Heart J. 2010;160:1170-7.
- [Google Scholar]
- Urinary neutrophil gelatinase-associated lipocalin (NGAL) is an early biomarker for renal tubulointerstitial injury in IgA nephropathy. Clin Immunol. 2007;123:227-34.
- [Google Scholar]
- Kidney NGAL is a novel early marker of acute injury following transplantation. Pediatr Nephrol. 2006;21:856-63.
- [Google Scholar]
- Urinary neutrophil gelatinase-associated lipocalin as a biomarker of nephritis in childhood-onset systemic lupus erythematosus. Arthritis Rheum. 2006;54:2577-84.
- [Google Scholar]
- Neutrophil gelatinase-associated lipocalin (NGAL) as a biomarker for acute renal injury after cardiac surgery. Lancet. 2005;365:1231-8.
- [Google Scholar]
- NGAL in acute kidney injury: From serendipity to utility. Am J Kidney Dis. 2008;52:395-9.
- [Google Scholar]
- Evaluation of the diagnostic performance of new markers for acute kidney injury associated with contrast administration. J Mahatma Gandhi Inst Med Sci. 2013;18:116-21.
- [Google Scholar]
- Neutrophil gelatinase-associated lipocalin levels in patients with Crohn disease undergoing treatment with infliximab. J Investig Med. 2010;58:569-71.
- [Google Scholar]
- Neutrophil gelatinase associated lipocalin (NGAL) in human neoplasias: A new protein enters the scene. Cancer Lett. 2010;288:10-6.
- [Google Scholar]
- Neutrophil gelatinase-associated lipocalin serum evaluation through normal pregnancy and in pregnancies complicated by preeclampsia. Acta Obstet Gynecol Scand. 2010;89:275-8.
- [Google Scholar]
- Elevated serum neutrophil gelatinase-associated lipocalin is an early predictor of severity and outcome in acute pancreatitis. Am J Gastroenterol. 2010;105:2050-9.
- [Google Scholar]
- Neutrophil gelatinase-associated lipocalin is expressed in osteoarthritis and forms a complex with matrix metalloproteinase 9. Arthritis Rheum. 2007;56:3326-35.
- [Google Scholar]
- Serum neutrophil gelatinase-associated lipocalin (NGAL) in predicting worsening renal function in acute decompensated heart failure. J Card Fail. 2010;16:49-54.
- [Google Scholar]
- Lipocalin-2/neutrophil gelatinase-B associated lipocalin is strongly induced in hearts of rats with autoimmune myocarditis and in human myocarditis. Circ J. 2010;74:523-30.
- [Google Scholar]
- Expression of neutrophil gelatinase-associated lipocalin in atherosclerosis and myocardial infarction. Arterioscler Thromb Vasc Biol. 2006;26:136-42.
- [Google Scholar]
- Estimating the prevalence of elevated plasma neutrophil gelatinase associated lipocalin level in patients with acute coronary syndromes and its association with outcomes. Indian Heart J. 2018;70:220-4.
- [Google Scholar]
- Serum levels of gelatinase associated lipocalin as indicator of the inflammatory status in coronary artery disease. Int J Inflam. 2012;2012:189797.
- [Google Scholar]
- Neutrophil gelatinase-associated lipocalin and L-FABP after percutaneous coronary interventions due to unstable angina in patients with normal serum creatinine. Adv Med Sci. 2009;54:221-4.
- [Google Scholar]
- Rapid detection of acute kidney injury by plasma and urinary neutrophil gelatinase-associated lipocalin after cardiopulmonary bypass. J Cardiovasc Pharmacol. 2009;53:261-6.
- [Google Scholar]
- Serum neutrophil gelatinase-associated lipocalin and cystatin-C are early biomarkers of contrast induced nephropathy after coronary angiography in patients with chronic kidney disease. Angiology. 2014;65:436-42.
- [Google Scholar]
- Serum neutrophil gelatinase associated lipocalin (NGAL) and cystatin C as early predictors of contrast induced acute kidney injury in patients undergoing percutaneous coronary intervention. Clinica Chimica Acta. 2014;435:48-52.
- [Google Scholar]
- Neutrophil gelatinase-associated lipocalin as an early marker of contrast-induced nephropathy after coronary angiography. Angiology. 2014;65:216-23.
- [Google Scholar]
- NGAL for the early detection of CIN after PCI. Scand J Clin Lab Invest. 2014;74:81-8.
- [Google Scholar]
- NGAL is an early predictive biomarker of contrast-induced nephropathy in children. Pediatr Nephrol. 2007;22:2089-95.
- [Google Scholar]
- Neutrophil gelatinase- associated lipocalin and cystatin C: Are they good predictors of contrast nephropathy after percutaneous coronary interventions in patients with stable angina and normal serum creatinine. Int J Cardiol. 2008;127:290-1.
- [Google Scholar]
- Prognostic utility of NGAL in predicting mortality and cardiovascular events in patients with STEMI treated with primary PCI. J Am Coll Cardiol. 2012;60:339-45.
- [Google Scholar]







