Translate this page into:
No detection of Helicobacter pylori in atherosclerotic plaques in end stage renal disease patients undergoing kidney transplantation
Address for correspondence: Dr. Ehsan Mansourian, No. 220, South Bozorg Mehr Street, Malek Abad Blv, Postal Code: 9186953141, Mashhad, Iran. E-mail: ehsan@live.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Chronic infection known to be a predisposing factor for the development of atherosclerosis. Several studies have found a possible role of Helicobacter pylori in the pathogenesis of atherosclerosis. The aim of this study was to investigate the presence of H. pylori in atherosclerotic plaques in iliac arteries in 25 end stage renal disease (ESRD) patients undergoing kidney transplantation. Esophagogastroduodenoscopy was performed in all patients before transplantation. Biopsy specimens obtained from gastric antrum were sent for pathologic evaluation. Gastric H. pylori infection was confirmed by microscopic assessment and rapid urease test. Arterial specimens were obtained from iliac arteries during kidney transplantation. Presence of H. pylori DNA in atherosclerotic plaques and healthy vessel samples was evaluated by the polymerase chain reaction (PCR). The mean age of patients was 44.1 ± 22.6 years. Risk factors in patients with atherosclerosis were hypertension (68%), diabetes mellitus (20%), hyperlipidemia (20%), positive family history (16%). Atherosclerotic plaques were found in 21 (84%) patients. PCR analysis did not detect H. pylori in any case. There was a significant relationship of atherosclerosis with hypertension (P = 0.006) but not with diabetes mellitus and hyperlipidemia (P = 0.5). There was no significant relationship between atherosclerosis and gastric H. pylori infection (P = 0.6). This study revealed no association between the presence of H. pylori as a pathogen of vessel walls and atherosclerosis in ESRD.
Keywords
Atherosclerosis
end stage renal disease
helicobacter pylori
kidney transplantation
Introduction
Atherosclerosis is a frequent cause of renovascular lesions especially in the elderly.[12] More than half of the end stage renal disease (ESRD) patients on dialysis are over 60 years old, the age in which atherosclerosis is more common.[3] The accelerated atherosclerotic process in chronic kidney disease and particularly those with ESRD cause a higher prevalence of coronary artery disease than the general population. High mortality rate in ESRD patients is related to cardiovascular disease, including accelerated atherosclerosis and its complications.[4]
Although diabetes mellitus, hypertension, smoking, and hyperlipidemia are the major known risk factors for the development ofatherosclerosis,[256] atherosclerosis may occur in the absence of these risk factors. Novel risk factors contributing to initiation and progression of atherosclerosis include inflammation and infections.[789] Some studies have found the association of elevated levels of C-reactive protein and future risk of coronary heart disease and stroke, supporting the hypothesis that inflammation plays a role in the pathogenesis of atherosclerosis.[1011] Although the clinical association between non-traditional risk factors and atherosclerosis is not yet proved, several studies suggest the possible role of different bacterial and viral pathogens as initiators of the inflammatory processes. Numerous infections have been concerned in human atherosclerosis such as Helicobacter pylori, Chlamydia pneumoniae, Herpes simplex virus, and Cytomegalovirus (CMV).[121314151617] Considering cardiovascular or cerebrovascular diseases, H. pylori infections may be associated with stroke and coronary heart disease as a result of the atherosclerotic changes in blood vessels that is due to a chronic inflammatory response.[18] Low socioeconomic condition may predispose the individuals to H. pylori infection and cardiovascular disease.[19]
The role of chronic inflammation as a suggested cause of high morbidity and mortality in these patients by acceleration of atherosclerosis has received considerable attention in recent years. The aim of this study was to search for the presence of H. pylori genomic deoxyribonucleic acid (DNA) in atherosclerotic plaques using polymerase chain reaction (PCR) in ESRD patients undergoing kidney transplantation.
Materials and Methods
Study population
This study was approved by the Research Ethics Committee of Mashhad University of Medical Sciences, Iran. The study population consisted of 25 patients, who were admitted to the kidney transplantation Department of the Ghaem hospital, for renal transplantation between November 2010 and March 2011. All subjects provided informed consent.
Baseline evaluation
Baseline evaluation included the collection of demographic information, medical history, risk factors for atherosclerosis, medication use, psychosocial evaluation, physical examination, and routine biochemical and hematological studies such as sampling of blood in the fasting state for sugar, lipid; blood grouping, white blood cell cross-match, viral studies (hepatitis B, hepatitis C, CMVand human immunodeficiency virus), electrocardiogram, and chest radiography.
Specimen collection and H. pylori assessment
All patients underwent esophagogastroduodenoscopy using a forward-viewing endoscope (Olympus CLV-160, Tokyo, Japan). The endoscopic appearance of esophagus, stomach, and duodenum were recorded. During endoscopy, biopsy specimens of gastric antrum were sent for pathologic evaluation. For detection of H. pylori infection, H and E staining on biopsy specimens and rapid urease test were used.
Arterial specimens containing atherosclerotic plaqueswere obtained from iliac arteries (internal or common iliac artery) during kidney transplantation under aseptic conditions. Tissue samples were fixed in formalin and stored at–80°C for histologic studies. Presence of H. pylori DNA in atherosclerotic plaques and in healthy vessel samples was evaluated by the PCR using the Sbsbio tissue Kit (Beijing, China). Presence of atherosclerosis was confirmed by microscopic assay.
Statistical analysis
Statistical analysis was performed using the Fisher's exact test or Mann–Whitney's U test. Logistic regression analysis was carried out to evaluate the independent influence of each variable (sex, age, atherosclerotic factors like smoking, diabetes mellitus, hypertension, hyperlipidemia, obesity, family history and H. pylori infection). P values less than 0.05 were considered statistically significant.
Results
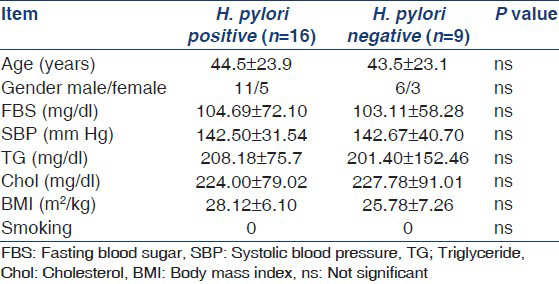
There were 25 patients, 9 women and 17 men. The mean age was 44.1 ± 22.6 (range 26-67) years. Upper gastrointestinal (GI) endoscopy revealed that gastric erosion and duodenal mucosal erythema were the most frequent types of mucosal lesions (16%), followed by esophagitis (8%), gastric ulcer (4%), and esophageal varices (4%). Normal upper GI endoscopy was found in 10 cases (40%). Of the 25 patients enrolled in the study, 16 (64%) were positive and 9 (36%) patients were negative for gastric H. pylori infection [Table 1].
Risk factors present in patients with atherosclerosis were hypertension (68%), diabetes mellitus (20%), hyperlipidemia (20%), and positive family history (16%). None of the patients were smokers or morbidly obese. Atherosclerotic plaques were found in 21 (84%) patients. There was a significant relationship between atherosclerosis and hypertension (P value = 0.006) but neither was any relationship between atherosclerosis and diabetes mellitus and hyperlipidemia (P = 0.5). There was no significant relationship between atherosclerosis and gastric H. pylori infection (P = 0.6). PCR analysis did not detect H. pylori in any of cases.
Discussion
Atherosclerosis is a multi-factorial disease. The importance of conventional risk factors in pathogenesis of atherosclerosis is well known. To refine newer risk factors in an individual, many studies have been done. Many studies have found a possible association between different microbial infections and atherogenesis. Although a positive association between H. pylori infection and atherosclerosis in carotid and coronary atherosclerotic diseases has been found,[9151617202122] some studies could not confirm this association.[23242526]
This study was not designated to investigate the causative effect of H. pylori on atherosclerosis nor to prove atherosclerosis as a certain etiology of ESRD. Our study showed no significant relationship between atherosclerosis and H. pylori infection. In this study, we could not detect H. pylori in atherosclerotic plaques of iliac artery (internal or common) in ESRD patients undergoing kidney transplantation whereas H. pylori was detected in 64% of patients in their gastric specimens.
We found H. pylori infection in 64% our patients. Sixty percent of evaluated patients had endoscopic abnormalities which are similar to other reports, occurring in 25-64% ESRD patients.[27] These findings can support the possibility of occurrence of post-transplantation peptic ulceralthough future prospective studies with larger study population are needed to confirm this hypothesis.
PCR is a sensitive, accurate diagnostic tool for H. pylori infection. In comparison to other methods for diagnosing H. pylori, PCR yields high sensitivity and specificity for H. pylori. PCR methods would increase the probability of H. pylori detection.[2829] Careful attention must be paid to ensure no cross-contamination, while gathering thebiopsies and laboratory phases.[2830] The false-positive result may possibly be due to the presence of cross-reacting DNAs such as yet-uncultured human micro-organisms. Another possible explanation for false positive is that there were no viable bacteria in the plaques biopsy samples but only dead organisms or chromosomal DNA remained in the cells after H. pylori infection.[31] One important disadvantage of conventional PCR in detection of H. pylori is inhibition of PCR amplification by a specific inhibitor, causing false negative by preventing positive finding.[282930]
Studies investigating the presence of H. pylori in iliac atherosclerotic plaque are few in the literature and this may be due to the difference in epidemiology of atherosclerosisin coronary, carotid, and iliac arteries andaccording to our knowledge there is no previous study in ESRD patients undergoing kidney transplantation to investigate the relationship between H. pylori and atherosclerosis.
The exact way by which inflammation associates with atherosclerosis is not known. The possible mechanisms contributing to the pathogenesis of atherosclerosis are induction of vascular inflammation, endothelial dysfunction and proinflammatory cytokines that may cause instability and rupture of pre-existing atherosclerotic plaques.[152632]
There are conflicting data about relationship of H. pylori in atherosclerosis. Although some studies found H. pylori in atherosclerotic plaques,[16172021] some other researchers found no evidence of H. pylori in the endarterectomy plaques of patients who were seropositive for H. pylori.[33343536373839] Thus, the issue of an association between H. pylori and atherosclerosis remains controversial.[40]
Blasi et al., studied 51 patients who underwent abdominal aortic aneurysm surgery for presence of H. pylori. In all cases PCR showed no evidence of H. pylori presence in atherosclerotic plaque specimensalthough 92.1% of patients were seropositive for H. pylori.[3334] Kaklikkaya et al., reported 21 patients undergoing surgery for aortoiliac occlusive disease, searching for H. pylori in aorta-iliac atherectomy specimens by PCR. They did not find H. pylori in any of specimens.[35] Dore et al., found no association between H. pylori and atherosclerosis in any of the 32 patients with cardiovascular disease.[36]
H. pylori infection can cause vascular disease directly, as a pathogen of vessel walls or indirectly through the inflammatory process. Activation of inflammatory pathways by infiltration of inflammatory cells that secrete the inflammatory cytokines induces adipocyte dysfunction, the main pathway to atherosclerosis; destabilize the fibrous cap tissue, endothelial desquamation, and plaques rupture which occur in atherosclerosis due to action of various inflammatory markers.[57818] In addition, H. pylori may have a role in promoting atherosclerosis by modifying lipid metabolism by elevating lowdensitylipoproteinand decreasing high density lipoprotein (HDL).[1927414243] H. pylori positive subjects have severe endothelial dysfunction which predisposes them to atherosclerosis.[1926]
The present study has several limitations. Atherosclerosis is a multi-factorial disease, and different risk factors should be considered. Since this was a descriptive study, we could not elucidate upon the mechanism by which H. pylori infection causes atherosclerosis. To discover this relationship, prospective cohort model studies should be performed. The relatively small population studied is a limiting factor and to elucidate the role of H. pylori in atherosclerosis, other studies should be carried out with larger number of patients.
Conclusion
This study revealed no association between the presence of H. pylori, asa pathogen of vessel walls, and atherosclerosis in ESRD. Although H. pylori may have a role in atherosclerosis by secretion of different types of cytokines which can promote a proinflammatory, procoagulant, and proatherogenic environment which does not necessarily need to be the result of the presence of H. pylori antigens on the walls of vessels in ESRD. Thus, these results suggest that the H. pylori infection is unlikely to be a direct cause of atherosclerosis but do not preclude an indirect role in the process.
Acknowledgment
The authors wish to thank Dr. Mohammad Khajedaluee for the statistical analysis and Dr. Mohammad Javad Mojahedi, Nephrologist for his help and assisstance. This article could not have been completed without the whole-hearted assistance of Dr. Negar Mokhtari Amirmajdi in editing the article.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Atherosclerotic ischemic nephropathy. Epidemiology and clinical considerations. Urol Clin North Am. 1994;21:195-200.
- [Google Scholar]
- Prospective study of atherosclerotic disease progression in the renal artery. Circulation. 1998;98:2866-72.
- [Google Scholar]
- Kidney transplantation in older adults: Does age affect graft survival? Urol J. 2005;2:93-6.
- [Google Scholar]
- Chronic Inflammation and Coronary Atherosclerosis in Patients with End-Stage Renal Disease. Cardiorenal Med. 2012;2:117-124.
- [Google Scholar]
- Nontraditional risk factors and biomarkers for cardiovascular disease: Mechanistic, research, and clinical considerations for youth: A scientific statement from the American Heart Association. Circulation. 2011;123:2749-69.
- [Google Scholar]
- Mechanisms of tissue injury in renal artery stenosis: Ischemia and beyond. Prog Cardiovasc Dis. 2009;52:196-203.
- [Google Scholar]
- C-Reactive protein, a sensitive marker of inflammation, predicts future risk of coronary heart disease in initially healthy middle-aged men: Results from the MONICA (Monitoring Trends and Determinants in Cardiovascular Disease) Augsburg Cohort Study, 1984-1992. Circulation. 1999;99:237-42.
- [Google Scholar]
- Chemokine receptor 7 knockout attenuates atherosclerotic plaque development. Circulation. 2010;122:1621-8.
- [Google Scholar]
- Impact of infectious burden on extent and long-term prognosis of atherosclerosis. Circulation. 2002;105:15-21.
- [Google Scholar]
- Inflammation, aspirin, and the risk of cardiovascular disease in apparently healthy men. N Engl J Med. 1997;336:973-9.
- [Google Scholar]
- Roles of infectious agents in atherosclerosis and restenosis: An assessment of the evidence and need for future research. Circulation. 1997;96:4095-103.
- [Google Scholar]
- Interactive role of infection, inflammation and traditional risk factors in atherosclerosis and coronary artery disease. J Am Coll Cardiol. 1998;31:1217-25.
- [Google Scholar]
- Search for genomic sequences of microbial agents in atherosclerotic plaques. Int J Immunopathol Pharmacol. 2011;24:243-6.
- [Google Scholar]
- Serum amyloid A as a predictor of coronary artery disease and cardiovascular outcome in women: The National Heart, Lung, and Blood Institute-Sponsored Women's Ischemia Syndrome Evaluation (WISE) Circulation. 2004;109:726-32.
- [Google Scholar]
- Detection of Chlamydia pneumoniae and Helicobacter pylori DNA in human atherosclerotic plaques by PCR. J Clin Microbiol. 2000;38:4408-11.
- [Google Scholar]
- Detection of Helicobacter pylori DNA in aortic and left internal mammary artery biopsies. Tex Heart Inst J. 2008;35:130-5.
- [Google Scholar]
- Association between Helicobacter pylori Seropositivity and the Coronary Artery Calcium Score in a Screening Population. Gut Liver. 2011;5:321-7.
- [Google Scholar]
- Endothelial dysfunction is reversible in Helicobacter pylori-positive subjects. Am J Med. 2011;124:1171-4.
- [Google Scholar]
- Detection of Chlamydia pneumoniae and Helicobacter pylori in atherosclerotic plaques of carotid artery by polymerase chain reaction. Int J Infect Dis. 2006;10:116-23.
- [Google Scholar]
- CagA-positive cytotoxic H. pylori strains as a link between plaque instability and atherosclerotic stroke. Eur Heart J. 2004;25:64-8.
- [Google Scholar]
- The role of infection in carotid plaque pathogenesis and stability: The clinical evidence. Curr Vasc Pharmacol. 2010;8:861-72.
- [Google Scholar]
- Absence of association between infectious agents and endothelial function in healthy young men. Circulation. 2003;107:1966-71.
- [Google Scholar]
- Infection with Helicobacter pylori, coronary heart disease, cardiovascular risk factors, and systemic inflammation: The Third National Health and Nutrition Examination Survey. J Natl Med Assoc. 2004;96:1470-6.
- [Google Scholar]
- Seropositivity to Chlamydia pneumoniae or Helicobacter pylori and coronary artery disease. Int J Cardiol. 2006;109:420-1.
- [Google Scholar]
- Predisposition to atherosclerosis by infections: Role of endothelial dysfunction. Circulation. 2002;106:184-90.
- [Google Scholar]
- Gastroduodenal mucosa in uraemia: Endoscopic and histological correlation and prevalence of helicobacter-like organisms. Gut. 1990;31:1093-6.
- [Google Scholar]
- Quantitative study of Helicobacter pylori in gastric mucus by competitive PCR using synthetic DNA fragments. J Clin Microbiol. 1996;34:2421-5.
- [Google Scholar]
- Real-time quantitative PCR for detection of Helicobacter pylori. J Clin Microbiol. 2002;40:3720-8.
- [Google Scholar]
- Unreliability of results of PCR detection of Helicobacter pylori in clinical or environmental samples. J Clin Microbiol. 2009;47:738-42.
- [Google Scholar]
- Detection of Helicobacter pylori gastritis by PCR: Correlation with inflammation scores and immunohistochemical and CLO test findings. Am J Clin Pathol. 2008;129:89-96.
- [Google Scholar]
- Helicobacter pylori infection is associated with decreased serum levels of high density lipoprotein, but not with the severity of coronary atherosclerosis. Lipids Health Dis. 2009;8:59.
- [Google Scholar]
- Detection of Chlamydia pneumoniae but not Helicobacter pylori in atherosclerotic plaques of aortic aneurysms. J Clin Microbiol. 1996;34:2766-9.
- [Google Scholar]
- No evidence for the presence of Helicobacter pylori in atherosclerotic plaques in abdominal aortic aneurysm specimens. Atherosclerosis. 1996;126:339-40.
- [Google Scholar]
- Investigation of Chlamydia pneumoniae DNA, chlamydial lipopolisaccharide antigens, and Helicobacter pylori DNA in atherosclerotic plaques of patients with aortoiliac occlusive disease. Cardiovasc Pathol. 2006;15:105-9.
- [Google Scholar]
- Detection of Chlamydiaepneumoniae but not Helicobacter pylori DNA in atherosclerosis plaques. Dig Dis Sci. 2003;48:945-51.
- [Google Scholar]
- Inflammation, infection and cardiovascular events in chronic hemodialysis patients: A prospective study. J Nephrol. 2003;16:245-51.
- [Google Scholar]
- Serological markers of Chlamydia pneumoniae, cytomegalovirus and Helicobacter pylori infection in diabetic and non-diabetic patients with unstable angina pectoris. Cent Eur J Public Health. 2003;11:102-6.
- [Google Scholar]
- A prospective study of infection and cardiovascular diseases: The Busselton Health Study. Eur J Cardiovasc Prev Rehabil. 2003;10:278-82.
- [Google Scholar]
- Helicobacter pylori infection is associated with elevated low density lipoprotein cholesterol levels in elderly Koreans. J Korean Med Sci. 2011;26:654-8.
- [Google Scholar]
- Current infection with Helicobacter pylori, but not Seropositivity to Chlamydia pneumoniae or Cytomegalovirus, is associated with an Atherogenic, Modified Lipid Profile. Arterioscler Thromb Vasc. 2001;21:427-32.
- [Google Scholar]
- The assessment of carotid intima media thickness and serum paraoxonase-1 activity in Helicobacter pylori positive subjects. Lipids Health Dis. 2010;9:92.
- [Google Scholar]







