Translate this page into:
Oral Anticoagulant-Related Nephropathy: A New Cause for an Old Entity
Corrresponding author: Patrícia Valério, Nephrology Department, Vila Franca de Xira Hospital, Vila Franca de Xira, Lisbon, Portugal. E-mail: p.valerios89@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Valério P, Soares E, Abrantes C, Góis M, Sousa H, Farinha A, et al. Oral Anticoagulant-Related Nephropathy: A New Cause for an Old Entity. Indian J Nephrol. 2025;35:113-4. doi: 10.25259/IJN_528_20
Dear Editor,
We present a case of a 70-year-old male admitted in the nephrology department due to fatigue, anorexia, vomiting, decreased urinary output and macroscopic hematuria. He had normal kidney function in the previous month.
His past medical history comprised of hypertension, bilateral hip prosthesis, pulmonary embolism during the postoperative period of the second surgery, and a recurrence of pulmonary embolism four months after oral anticoagulation suspension. He was medicated with rivaroxaban 20 mg id and perindopril 4 mg daily for 3 years.
The patient had been in his usual heath until 1.5 months ago, when he was admitted because of erysipelas and skin lesions suggestive of vasculitis in the inferior limbs. Skin biopsy that showed leukocytoclastic vasculitis. He was successfully treated with piperacillin-tazobactam 4500 mg every eight hours and prednisolone 20 mg daily for two weeks.
Five weeks later, he started vomiting, with oliguria and gross hematuria. On admission, he presented an arterial blood pressure of 140/80 mmHg, and a normal physical examination, with no vasculitis signs. Table 1 presents admission laboratory results. Kidney ultrasound showed enlarged kidneys (140 mm), with preserved corticomedullary differentiation, without hydronephrosis.
The patient was transferred to the nephrology department to proceed with the investigation [Table 1]. He was started on urgent hemodialysis because of oliguric kidney failure with uremic syndrome. A kidney biopsy was performed: the sample had 12 glomeruli, 9 with global sclerosis, 2 with cellular crescents with intraglomerular hemorrhage and segmental endocapillary hypercellularity; the sample presented 80% of interstitial fibrosis and tubular atrophy, associated with interstitial hemorrhage and dysmorphic red blood cell casts; the arteries showed no changes. Immunofluorescence examination showed a C3 parietal granular deposition and electronic microscopy revealed subepithelial humps. These histologic changes suggest anticoagulation-related nephropathy (ARN) and infection-related glomerulonephritis (IRGN) [Figure 1].
| Laboratory analysis | Result |
|---|---|
| Admission | |
| Hemoglobin | 11.0 g/dL |
| White blood cell and platelet count | Normal |
| Serum creatinine | 21.6 mg/dL |
| Serum urea | 343 mg/dL |
| Serum potassium | 8.6 mmol/L |
| INR and activated partial thromboplastin time (aPTT) | Normal (0.9 and 24.4 seconds, respectively) |
| C-reactive protein | Negative |
| Random urine analysis | Proteinuria (+); sediment with pyuria and red blood cells (++), with dysmorphic red blood cells |
| Arterial blood gas | Metabolic acidemia - pH 7.09, pCO2 17.9 mmHg, pO2 108 mm Hg, HCO3- 8.5 mmol/L, lactate 0.9 mmol/L |
| Investigation | |
|
Random urine analysis (second sample) |
Minor proteinuria (50 mg/dL); sediment with dysmorphic red blood cells (65 cells/ low power field) |
| Blood and urine cultures | Negatives |
| Antistreptolysin-O test | Negative |
| Peripheral blood smear | Normal |
| C3 complement level | Decreased (82 mg/dL) |
| Remain immunological study1 | Negative |
| Serum immunofixation | No monoclonal component |
| Immunoglobulins and light chains dosing; free light-chain ratio | Normal |
| Human immunodeficiency virus (HIV), hepatitis B virus (HBV) and hepatitis C virus (HCV) serologic tests | Negative |
INR: International Normalized Ratio, 1 - C4 complement level was normal; antinuclear antibody (ANA), extractable nuclear antigen antibodies (ENA), anti-neutrophil cytoplasmic antibody (ANCA), anti-glomerular basement membrane antibody, anticardiolipin antibodies, beta 2 glycoprotein antibodies and cryoglobulins.
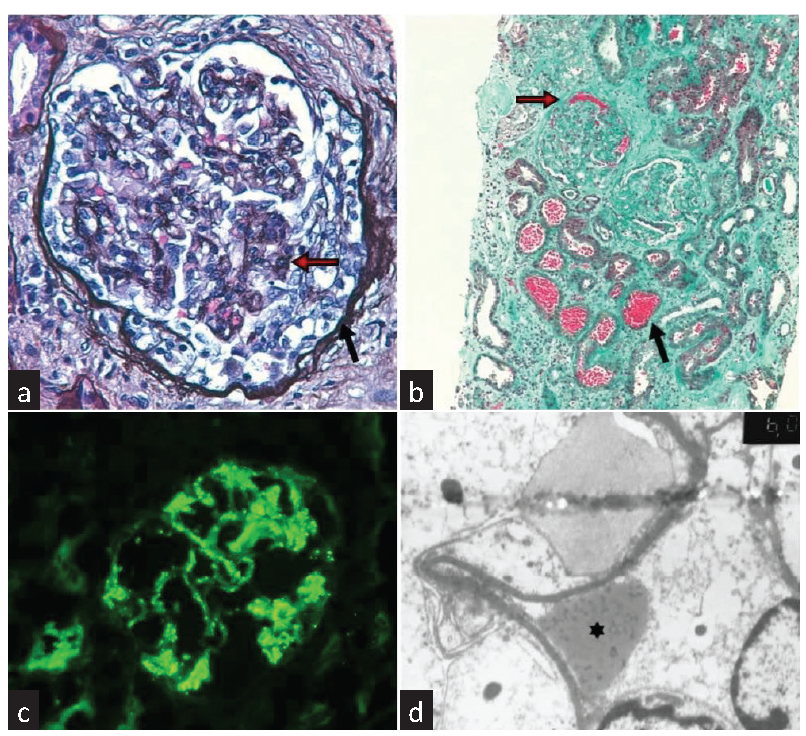
- (a) Silver stain (magnification ×400), on light microscopy (LM): cellular crescent (black arrow) and endocapillary hypercellularity (red arrow); (b) Masson Trichrome stain (magnification ×100), on LM: extensive interstitial fibrosis and tubular atrophy, red blood cells’ casts (black arrow) and glomerular hemorrhage (red arrow); (c) Immunofluorescence: glomerular C3 granular deposition; (d) Electronic microscopy (magnification × 6000): subepithelial hump (*).
ARN was originally described in patients who received supratherapeutic doses of warfarin, defined as an unexplained increase in serum creatinine in the setting of an international normalized ratio of >3.0.1–4
ARN mechanisms rely on glomerular hemorrhage and consequent occlusive red blood cells’ casts, leading to acute glomerular and tubular injuries. However, pathogenesis is not yet well understood.1–3
Several independent risk factors were identified, namely chronic kidney disease (CKD), age, heart failure, hypertension, diabetes mellitus, and medications which interfere with glomerular hemodynamics.2,3 ARN is associated with increased renal morbidity and all-cause mortality. Early recognition is essential to prompt anticoagulation suspension.3,4
There are already some case reports of ARN with direct action anticoagulants (DAAs),5–7 all presenting the same pathological features of warfarin-related nephropathy. While warfarin remains the most common oral anticoagulant, DAAs give us an alternative with some advantages, such as no need for routine monitoring and fewer interactions. However, all DAAs are excreted by kidney in various degrees, but only with a slight dose adjustment to kidney function, which can expose CKD patients to supratherapeutic doses. As little is known about kidney DAA effects, routine monitoring of kidney function is recommended.2,3
Our patient also showed pathological features of an acute IRGN. This probably leads to acute kidney injury (AKI), which explains ARN in a patient on rivaroxaban for a long time.
Over time, the serum creatinine decreased to 2.5 mg/dL. Also, urinary sediment and C3 level returned to normal, reflecting the resolution of the nephritic process.
The patient remained without anticoagulation, with no thrombotic complications during follow up.
In conclusion, ARN is certainly underdiagnosed due to confounding factors, and the risk associated with performing a kidney biopsy. Also, an adequate balance between the risks and benefits of anticoagulation is essential, especially in CKD patients or those with a high risk for AKI.
Conflicts of interest
There are no conflicts of interest.
References
- Acute kidney injury during warfarin therapy associated with obstructive tubular red blood cell casts: A report of 9 cases. Am J Kidney Dis. 2009;54:1121-6.
- [CrossRef] [PubMed] [Google Scholar]
- Oral anticoagulants and risk of nephropathy. Drug Safety. 2015;38:527-33.
- [CrossRef] [PubMed] [Google Scholar]
- Anticoagulation-related nephropathy 2016. J Thromb Haemost. 2016;14:461-7.
- [CrossRef] [PubMed] [Google Scholar]
- The neglected fact: Anticoagulation-related nephropathy. Iran J Kid Dis. 2019;13:343-5.
- [Google Scholar]
- Warfarin-related nephropathy in a patient with mild IgA nephropathy on dabigatran and aspirin. Clin Kidney J. 2013;6:507-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Anticoagulant related nephropathy induced by dabigatran. Case Rep Nephrol. 2018;2018:7381505.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]






