Translate this page into:
Outcomes and characteristics of intermittent hemodialysis for acute kidney injury in an intensive care unit
Address for correspondence: Mr. Suresh Sankarasubbaiyan, AB 48, Annanagar, Chennai - 600 040, India. E-mail: suresh150902@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Renal replacement therapy in intensive care units (ICUs) varies globally and is dependent on medical and non-medical factors. We performed a retrospective analysis of patients initiated on dialysis in an ICU. Patient and clinical characteristics, cause of kidney injury, laboratory parameters, hemodialysis characteristics, and survival were reviewed. Acute physiological and chronic health (APACHE II) score was use to study the sickness profile. A total of 92 patients underwent 525 hemodialysis sessions. There were 60 male and 32 female patients. The mean age of the patients was 56.5 ± 16 years. The cause of acute kidney injury included sepsis 64, cardiac 7, malaria 7, postoperative 4, trauma 3, poisoning 2, and others 4. Vasopressors were used in 75% and mechanical ventilation was used in 74 (82%) of the cases. APACHE II score was 22.3 + 7.4. The mean creatinine level was 3.6 + 3.7 mg/dl. The duration of dialysis was less than 4 h in 324 (61.2%) sessions and greater than 6 h in 118 (22.5%) sessions. The percentage of 30-day survival was 30%. Intermittent hemodialysis customized to renal support needs of ICU patients is an appropriate option in resource-limited settings.
Keywords
Acute kidney injury
India
intensive care unit
renal replacement therapy
Introduction
Acute kidney injury (AKI) is occurs in 5.7 - 24% of intensive care unit (ICU) patients.[12] It is commonly associated with multiorgan failure, pre-existing renal disease, sepsis, and renal hypoperfusion.[1–4] Renal replacement therapy (RRT) is reportedly used in 51-82% of patients with AKI in ICU.[34] Mortality of patients with AKI in ICU ranges from 46.8% to 60% and use of vasopressors, mechanical ventilation, shock (septic and cardiogenic) were independent predictors of mortality.[12] Treatment of AKI includes addressing the etiology, hemodynamic support, maintaining fluid and electrolyte balance, avoiding nephrotoxic drugs, appropriate drug dosing for level of glomerular filtration rate, and RRT. The preferred choice for RRT among peritoneal dialysis (PD), intermittent hemodialysis (IHD), or continuous renal replacement therapy (CRRT) remains unresolved despite several randomized controlled trials.[5–8]
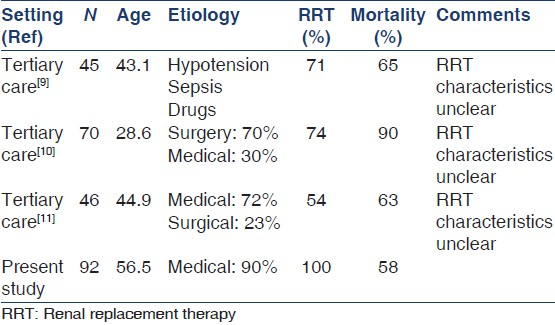
In the Indian context, three studies have previously reported the profile and outcome of AKI in ICUs.[9–11] But the treatment characteristics of RRT, therapy modification, sickness profile were not described. Hence, our study aimed to study the patient characteristics, renal replacement practice of modified IHD, and the outcome of patients with AKI in an ICU in a secondary care institution in urban south India.
Materials and Methods
A retrospective study of all consecutive patients over the age of 18 who underwent hemodialysis in the medical ICU between January 2004 and January 2007 was performed. Patient demographics, clinical characteristics, reasons for renal replacement, vasopressor use, mechanical ventilation, and enteral nutrition support were recorded. Biochemical and hematological parameters at the onset of hemodialysis were noted. Acute physiological and chronic health (APACHE II) score was assessed to describe the sickness profile.
Hemodialysis (HD) was performed using the Fresenius 4008 B machine. Standard water treatment was used. Dialysate concentrates were commercially purchased. F5 polysulfone dialyzers were used (surface area of the dialyzer was 0.9 m2). All the patients were anticoagulated with unfractionated heparin-based on clinical risk assessment. The intensive care team and nephrologist decided on ultrafiltration based on clinical risk assessment and hemodynamics. HD characteristics that included blood flow rate (BFR), dialysate flow rate (DFR), anticoagulation, and ultrafiltration (UF) were reviewed. Major complications were documented. All the patients in the ICU received only HD as renal replacement therapy and none received PD or continuous renal replacement therapy.
Patient survival was recorded at 30 days after initiation of renal support. Renal survival was defined as dialysis-free survival 30 days after initiation. Data were shown as mean ± SD. Microsoft Excel and Epi info software were used for data analysis. Mean of various parameters were compared among the survivors and non-survivors using appropriate statistical tests and P < 0.05 was considered significant. Continuous variables were categorized using median as the cut point. Univariate analysis for risk factors for non-survivors was done and unadjusted odds ratios were computed. Multivariate analysis was done using logistic regression methods and adjusted odds ratios were computed.
Results
A total of 92 patients underwent 525 HD treatments during the study period. Baseline characteristics are described in Table 1. There were 60 male and 32 female patients. The mean age was 56.5 ± 16 years. The etiology of renal failure were sepsis in 64 patients, cardiac in seven patients, malaria for seven patients, post-surgical for four, trauma for two patients, poisoning for two patients, and other causes for four patients.

Table 1 also illustrates treatment characteristics: 75% (68 patients) of the patients were on vasopressors, 82% (74 patients) were on mechanical ventilation and 77% (70 patients) received enteral nutrition support. APACHE II score mean was 22.3 ± 7.4, mean BUN was 63.6 ± 37.7 mg%, mean serum creatinine was 3.6 ± 3.7 mg%, and mean pH was 7.2 ± 0.2. The mean serum sodium was 133.3 ± 11.2 mEq/L and mean serum potassium was 5.0 ± 4.5 mEq/L. Mean hemoglobin was 9.4 + 2.4 g% and mean total white cell count was 16.2 ± 16.9 cells/mm3, and lastly, mean platelets were 1.5 ± 1.2 m.cells/mm3.
Table 2 shows the dialysis prescription pattern. The mean time difference between admission to ICU and start of HD was 6.8 days. Dialysis duration distribution: 324 sessions (61.2%) of dialysis for <4 h, 83 sessions (15.9%) were for 4-6 h and 118 sessions (22.5%) persisted for >6 h. Mean BFR was 191.8 ± 35.2 ml/min, and mean DFR: 474.9 ± 109.8 ml/min. Mean heparin used was 281 ± 339 u/h and mean UF 242.1 ± 279.3 ml/h. 67 treatments (12.7%) had hypotension.
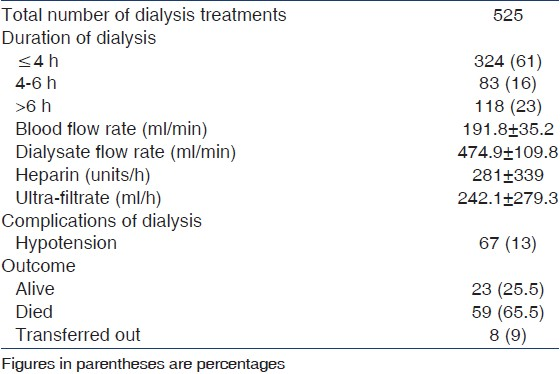
Outcome was analyzed at 30 days from the start of HD [Table 2]. Of the 92 patients; 23 (25.%) were alive, 59 (64.1%) died, and 10 (10.8%) patients were either transferred or discharged at request.
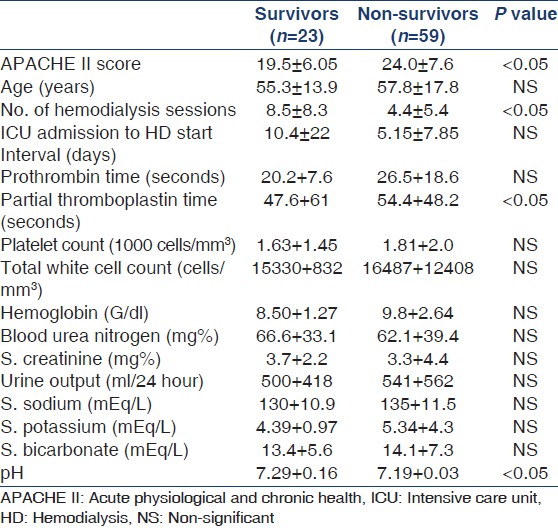
A comparison of survivors and non-survivors was done to identify the predictors for survival. Non-survivors had significantly higher APACHE II scores, lesser number of HD treatments (indicating early mortality), lower pH, and higher PTT. There was no significant difference in serum creatinine, urine output, and hemoglobin between the two groups [Table 3]. Use of ventilatory support, nasogastric feeding, and vasopressors use were not significantly associated with non-survival (data not presented here). APACHE II score above median (>21.5), HD treatments below median (<3), PTT above median (>37.5) and pH below median (<7.2) were significantly associated with non-survival in the univariate analysis [Table 4]. We also did multivariate analysis; however, the same factors were not significant, probably due to the small sample size.

Discussion
Our study illustrated that appropriate modified practice of IHD could be customized to the clinical needs of patients with AKI in ICU. It helped achieve reasonable clinical outcome in environments with resource constraints. Modifications adopted in our practice included increasing frequency of dialysis, varying duration of dialysis, minimizing anticoagulation, reducing dialysate flow, and customizing ultrafiltration based on hemodynamic status. The spectrum of ICU patients developing AKI and the age profile in our patient population was similar to ICU in the developed world.[1] The younger age reported in previous Indian studies was likely due to the socioeconomic class of patients attending tertiary care public hospitals.[9–11] Male patients constituted the majority (66.6%) and sepsis was a major causative factor of AKI. This shifting age pattern was consistent with the shifting demographics in India, health-seeking pattern among patients in private health sector, and increasing chronic diseases in India.
The sickness profile was assessed using APACHE II. Though there are several “sickness scoring systems” uniquely designed for patients with AKI, we used the APACHE II for ease of implementation. The large proportion of sepsis in our series accounted for the high prevalence of multiorgan failure.
Globally, the choice of modality for RRT varies across centers. In recent international surveys on clinical practice patterns, it was found that 80% of the centers administer CRRT, 17% used intermittent RRT (IRRT), and a very few used PD.[2] Continuous therapies were commonly used in Europe, whereas in Australia, more than 90% of the critically ill patients with dialysis-dependent renal failure were treated with CRRT.[2] But CRRT is a labor-intensive and expensive modality of RRT. The above factors were major limitations to utilizing CRRT in nephrology practice in India. Modifications of conventional IHD such as sustained low efficiency dialysis, short daily dialysis, and isolated ultrafiltration were shown to achieve satisfactory patient outcome.[1213] In our study, 83 sessions (15.9%) went on from 4 to 6 h, 118 sessions (22.5%) persisted for >6 h, and about 30% of dialysis treatment were on consecutive days. The retrospective nature of the study limited reviewing other important adverse effects including new onset of infections from access, major bleeding, and transient cardiac arrhythmias. Poor hemodynamic tolerance of IHD was a common problem for patients in the ICU. Hypotension occurred in 12.7% of the IHD sessions in this study. Due to retrospective nature of study, recall bias and improper documentation may influence reliability of our findings. The salient feature was that the patient survival in our study was similar to that published in developed countries. This fact may indirectly indicate that major adverse effects may not have been missed in our data review.
There is yet no consensus on the timing of initiation of RRT. The mean BUN and creatinine of patients in our study reflect the timing of initiation to be reasonably consistent with contemporary practice. Significantly, it was noted that it was possible that patients initiated early on RRT might have survived even without RRT. There were no randomized trials comparing the outcome of the practice of modified techniques of HD and CRRT in India. A recent randomized trial from India compared intermittent PD and continuous renal replacement therapy in a small group of patients in ICU.[14] The sickness profile of these patients was similar to that our study. In addition, this trial showed that patients in the PD group had comparable outcome to the CRRT group.[14] A recent meta-analysis attempted to address this question noted no better survival with either modality, but there was significant heterogeneity in studies.[15]
Mortality of patients treated with RRT depended heavily on associated organ dysfunction and co-morbidity, but for a general ICU population, the mortality was approximately 50-60%.[121213] which is also reflected in our study (58% at 30 days).
The strength of our study was a large sample size and it is the first study to describe the dialysis prescription details in India [Table 5]. In addition, none of the previous studies have described the treatment characteristics in detail. The limitations were retrospective nature, inadequate details of dosage, and duration of vasopressor use, lack of dialysis dose delivery measurement, and possible under reporting of adverse effects.
We conclude that modification of IHD by varying frequency of treatment, duration of HD, anticoagulation, ultrafiltration, blood flow rate, and dialysis flow rate may be a viable option for RRT in medical intensive care patients in developing countries.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Acute renal failure in critically ill patients: A multinational, multicenter study. JAMA. 2005;294:813-8.
- [Google Scholar]
- A prospective multicenter study of the epidemiology, management, and outcome of severe acute renal failure in a “closed” ICU system. Am J Respir Crit Care Med. 2000;162:191-6.
- [Google Scholar]
- Spectrum of acute renal failure in the intensive care unit: The PICARD experience. Kidney Int. 2004;66:1613-21.
- [Google Scholar]
- Effect of acute renal failure requiring renal replacement therapy on outcome in critically ill patients. Crit Care Med. 2002;30:2051-8.
- [Google Scholar]
- Patient and kidney survival by dialysis modality in critically ill patients with acute kidney injury. Int J Artif Organs. 2007;30:281-92.
- [Google Scholar]
- Continuous renal replacement therapy: A worldwide practice survey. The beginning and ending supportive therapy for the kidney (B.E.S.T. kidney) investigators. Intensive Care Med. 2007;33:1563-70.
- [Google Scholar]
- A randomized clinical trial of continuous versus intermittent dialysis for acute renal failure. Kidney Int. 2001;60:1154-63.
- [Google Scholar]
- A randomized controlled trial comparing intermittent with continuous dialysis in patients with ARF. Am J Kidney Dis. 2004;44:1000-7.
- [Google Scholar]
- Spectrum of acute renal failure and factors predicting its outcome in an intensive care unit in India. Ren Fail. 2006;28:119-24.
- [Google Scholar]
- Acute renal failure in an intensive care unit in India – Prognostic factors and outcome. J Nephrol. 1999;12:390-4.
- [Google Scholar]
- Acute renal failure in the intensive care unit. J Assoc Physicians India. 2006;54:784-8.
- [Google Scholar]
- Daily hemodialysis and the outcome of acute renal failure. N Engl J Med. 2002;346:305-10.
- [Google Scholar]
- Extended daily dialysis: A new approach to renal replacement for acute renal failure in the intensive care unit. Am J Kidney Dis. 2000;36:294-300.
- [Google Scholar]
- Comparing continuous venovenous hemodiafiltration and peritoneal dialysis in critically ill patients with acute kidney injury: A pilot study. Perit Dial Int. 2011;31:422-9.
- [Google Scholar]
- Continuous versus intermittent renal replacement therapy for critically ill patients with acute kidney injury: A meta-analysis. Crit Care Med. 2008;36:610-7.
- [Google Scholar]







