Translate this page into:
Outcomes of Primary Arteriovenous Fistula for Hemodialysis in Elderly Patients (>65 Years) with End Stage Renal Disease: A Study on Indian Population
Address for correspondence: Dr. U. P. Singh, Department of Urology and Renal Transplant, SGPGIMS, Lucknow - 226 014, Uttar Pradesh, India. E-mail: dr_upsingh@yahoo.co.in
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
The outcome of arteriovenous fistula (AVF) for hemodialysis (HD) in elderly population remains an issue. The aim of our study was to evaluate the outcomes of arteriovenous fistulas created at our institute in patients older than 65 years.
Methods:
All chronic HD patients with age >65 years who had an AVF created between January 1, 2010 and January 1, 2017 were included retrospectively. Baseline demographic information including age, gender, etiology of renal failure and comorbidities were recorded. Access characteristics including access type and anatomic location were recorded. The end point of study was primary and secondary patency. Minimum follow up period of study was 1 year.
Results:
A total of 422 AVF were created within the study period. The mean age was 69.3 years. The anatomical site of AVF creation was radiocephalic (RCF) in 74.8% (n = 316), brachiocephalic (BCF) in 18.9% (n = 80) and brachiobasilic (BBF) in 6.1% (n = 26). At one year after creation, cumulative survival of the AVF was 64.7%. At 36 months the primary and secondary patency of RCF, BCF and BBF was 43.6%, 58.6%, 42.6% and 47.3%, 62.5%, 56.9% respectively. The overall median survival did not differ between RCF and BBF fistulas. However, when both were compared with BCF (median survival 1034 days), BBF (median survival 741 days) and RCF (median survival 592 days) had significantly poorer survival (P = 0.004). The most common reason for access failure was thrombosis (28.4%) followed by failure to mature (9%) and aneurysm related complications (9%).
Conclusions:
Age should not be a limiting factor when choosing AVF as the preferred HD access. Brachiocephalic AVF has better primary and secondary patency with higher overall median survival. However RCF also provides reasonably good survival rates with acceptable complications in elderly population. Thrombosis and fistulas that fail to mature present as a primary concern to patients in elderly population, and demand further study.
Keywords
Arteriovenous fistula
elderly
hemodialysis
patency
Introduction
In current era, the hemodialysis has achieved broad acceptance among patients and physicians due to improved technology and innovation to sustain life in patients of end stage renal disease.[1] The introduction of external arteriovenous shunt by Schribner was a milestone in making Chronic HD feasible for patients with end-stage renal disease (ESRD). This was further advanced by development of arteriovenous fistula (AVF) by Brescia et al.[2] The minimum cost of maintenance, least amount of intervention with easy and superior access, better patient survival and minimum rates of complications when compared with all other forms of vascular access has made arteriovenous fistula first choice of vascular access for chronic HD.[34567]
A group of young non diabetic patients were selected for creation of AVF in original description of AVF in 1966 by Cimino and Brescia. However, the number of older patients requiring maintenance HD has increased significantly due to better availability of dialysis along with increased prevalence of end-stage renal disease in the elderly.[8] Since arteriovenous fistulas (AVFs) have a limited life span, the primary approach for planning vascular access has been to use distal vessels first so that proximal vessels can be preserved for an anticipated future need of a new access. A counterview to this is the shortened life expectancy of elderly patients on maintenance hemodialysis as they may not survive to need a second AVF.[910] Moreover the maturation rates of AVF are poorer in older patients because of high incidence of diabetes and hypertension leading to poorer vascular endothelial health accompanied with higher incidence of peripheral vascular disease resulting in impairment of blood inflow to AVF.[11]
These facts have changed the preference of operating surgeons for creation of an elbow fistula (brachiocephalic AVF) rather than wrist fistula (radiocephalic AVF) in older patients.[12345] However the higher rate of vascular steal syndrome with brachiocephalic AVFs remains a counterbalancing argument.[12] There is limited availability of literature describing outcomes of AVF placements in the elderly; more so in Indian population, with conflicting conclusions. Indians are affected by cardiovascular diseases more than a decade earlier as compared to European population.[1314] Although the prevalence of traditional risk factors like hypertension, hypercholesterolemia and smoking is not higher in Indians, but, some risk factors for atherosclerosis such as higher total cholesterol to high-density lipoprotein cholesterol ratio, high triglyceride levels, visceral obesity and type 2 diabetes mellitus are particularly present in Indians.[151617] The aim of our study was to evaluate the outcomes of arteriovenous fistulas in Indian elderly population.
Materials and Methods
This study is a retrospective analysis of collected data (for clinical care) on a cohort of patients with consecutively created AVF. All chronic HD patients with age more than 65 years who had an AVF created within this program between January 1, 2010 and July 1, 2016 were included in the study. Prior to AVF creation, the surgeon assessed all patients. Preoperative USG with color Doppler for upper limb vessels using a pre-designed pro forma was routinely performed. All AVF were created using end to side anastomoses and were followed up by surgeon after creation and first venipuncture was done after assessment by nephrologist. The AVF were created by 4 surgeons with experience of 3 years or more using the same technique. Initially RCF was created provided the vessels had adequate caliber (2mm or more) and flow (25 ml/second or more). Otherwise the elbow was explored and BCF created. BBF was created when no suitable cephalic vein was found. A policy of minimum 6 to 8 weeks maturation period was strictly followed before first venipuncture.
Since January 1, 2010, baseline demographic information has been collected, including patient characteristics: age, gender, comorbidities, and etiology of renal failure. Access characteristics including access type and anatomic location were recorded.
Definitions of outcomes
Primary patency was the “interval from the time of access creation until any intervention designed to maintain or to re-establish patency, access thrombosis, or the time of measurement of patency”. Secondary patency “was the interval from the time of access placement until access abandonment, thrombosis, or the time of patency measurement including intervening manipulations (surgical or endovascular interventions) designed to re-establish functionality in thrombosed accesses.”[18] In our study, all patients who had failure of AVF, underwent evaluation by intervention radiologists. Angiography followed by balloon dilatation was done in these patients.
Secondary patency measures the period for which AVF was in use hence it was considered the most important end point. Minimum follow up period was 1 year. The patients who switched to peritoneal dialysis, died with a functioning AVF, underwent renal transplantation or transferred to another dialysis center were excluded from the study.
Data analysis was done using student t-test for continuous data and Chi-square test was used for dichotomous data. One way ANOVA was used to analyse continuous data when more than 2 groups were involved. Kaplan-Meier plots were used for estimation of time-to-event distributions. All tests of significance were two-sided with a P value <0.05. The statistical software SPSS 20.0 was used.
Results
A total of 422 AVF were created within the study period. The patient and access characteristics are presented in Table 1. Seventy-five (75.8) percent of all study patients were male, and 24.2% were females. The mean age of group was 69.3 years. The etiology of renal failure was diabetes in 35.1% (n=148), hypertension in 11.1% (n=47) and glomerulonephritis in 38.3% (n=162). Diabetes as a comorbidity was present in 33% (n=139), hypertension in 83.1% and CAD in 19.4% (n=82) patients.
| Number of patients | 422 |
| Age (years), mean±SD | 69.3±2.5 |
| Sex, n (%) | |
| Male | 320 (75.8) |
| Female | 102 (24.2) |
| Etiology, n (%) | |
| Diabetes | 148 (35.1) |
| Hypertension | 47 (11.1) |
| Glomerulonephritis | 162 (38.3) |
| Interstitial nephritis | 16 (3.7) |
| Other | 49 (11.6) |
| Comorbidities, n (%) | |
| DM | 139 (33) |
| HTN | 351 (83.1) |
| CAD | 82 (19.4) |
| CHF | 51 (12) |
| PVD | 21 (5) |
| COPD | 17 (4) |
| Anatomical site, n (%) | |
| RC | 316 (74.8) |
| BC | 80 (18.9) |
| BB | 26 (6.1) |
SD: Standard deviation, COPD: Chronic obstructive pulmonary disease, PVD: Peripheral vascular disease, CHF: Congestive heart failure, CAD: Coronary artery disease, HTN: Hypertension, DM: Diabetes mellitus, RC: Radiocephalic, BC: Brachiocephalic, BB: Brachiobasilic
The anatomical site of AVF creation was radio-cephalic in 74.8% (n=316), brachiocephalic in 18.9% (n=80) and brachio-basilic in 6.1% (n=26). The primary patency rates (at 6 months, 1, 2 and 3 years) of RCF, BCF and BBF is summarized in Table 2. Primary patency of BCF was found to be significantly better than RCF at 1 year (70.5% vs 58.3%) and 3 years (58.6% vs 43.6%). However when compared to BBF, primary patency of BCF was marginally better at 1 year (70.5% vs 68.3%) but significantly higher at 3 years (58.6% vs 42.6%) as shown in Figure 1. At one year after creation, the cumulative survival of AVF was 64.7%. The overall median survival did not differ between radiocephalic and brachiobasilic fistulas. However, when both were compared with brachicephalic AVF (median survival 1034 days), brachiobasilic and radiocephalic AVF (median survival 496 and 541 days respectively) had significantly poorer survival (P = 0.004). The primary patency rates of RCF, BCF and BBF were not significantly different among age groups (65-70, 71-75 and >75 years) as given in Table 3.
| Fistula | 6 months | 12 months | 24 months | 36 months | Median days |
|---|---|---|---|---|---|
| RC | 84.6% | 58.3% | 49.1% | 43.6% | 541 |
| BC | 89.5% | 70.5% | 63.2% | 58.6% | 1034 |
| BB | 79.9% | 68.3% | 56.8% | 42.6% | 496 |
| Overall | 83.3% | 64.7% | 58.8% | 51.7% | 692 |
RC: Radiocephalic, BC: Brachiocephalic, BB: Brachiobasilic
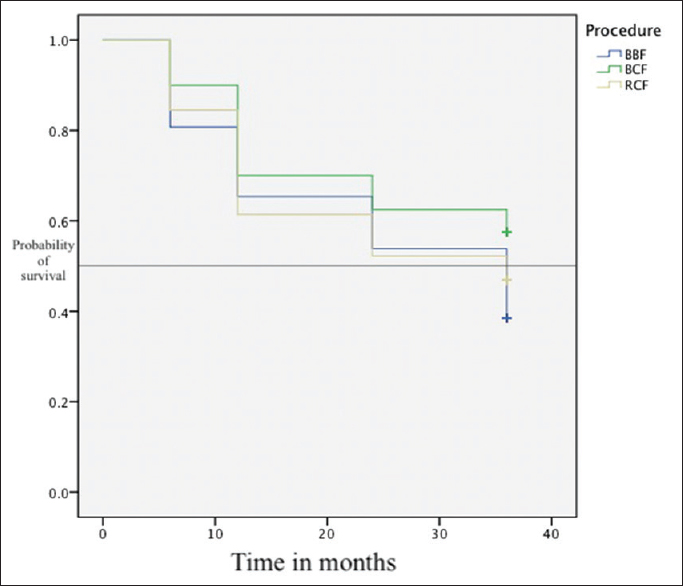
- Primary patency of brachiobasilic fistula, brachiocephalic fistula and radiocephalic fistula
| 1 year patency | RCF (n=316) | BCF (n=80) | BBF (n=26) | P |
|---|---|---|---|---|
| 65-70 (n=229) | 60.26% (n=172) | 71.9% (n=43) | 69.7% (n=14) | 0.149 |
| 71-75 (n=113) | 57.6% (n=85) | 69.2% (n=21) | 66.7% (n=7) | 0.312 |
| 76 and above (n=80) | 57.5% (n=59) | 67.3% (n=16) | 65.9% (n=5) | 0.419 |
RCF: Radiocephalic fistula, BCF: Brachiocephalic fistula, BBF: Brachiobasilic fistula
The secondary patency rates are summarized in Table 4. The overall secondary patency at 1 year was 72.5% and was reduce to 58.3% at 3 years as shown in Figure 2. The secondary patency of BCF was significantly better than that of BBF and RCF at 1 year (75.2% vs 72.7% vs 68.1%) and at 3 years (62.5% vs 56.9% vs) as shown in Figure 3. The median survival of BC fistula was significantly higher than RC and BB fistula (1321 vs 741 vs 592 days respectively).
| Fistula | 6 months | 12 months | 24 months | 36 months | Median days |
|---|---|---|---|---|---|
| RC | 87.1% | 68.6% | 56.4% | 47.3% | 741 |
| BC | 92.1% | 75.2% | 68.1% | 62.5% | 1321 |
| BB | 81.1% | 72.7% | 64.1% | 56.9% | 592 |
| Overall | 87.7% | 72.5% | 62.2% | 58.3% | 891 |
RC: Radiocephalic, BC: Brachiocephalic, BB: Brachiobasilic

- Overall primary and secondary patency of arteriovenous fistula

- Secondary patency for brachiobasilic fistula, brachiocephalic fistula and radiocephalic fistula
The primary reason for AVF loss was thrombosis in 28.4% (n=120 patients). Thirty-eight (9%) of AVF were lost each due to maturation failure and due to aneurysm related complications [Table 5]. In 2 patients, ligation of AVF done due to severe steal syndrome.
| Reason for AVF loss | RC:BC:BB (n) |
|---|---|
| Thrombosis/stenosis | 96:17:7 |
| Failure to mature | 32:4:2 |
| Aneurysm related complications | 26:9:3 |
| Ligation due to severe steal syndrome/high cardiac output | 0:2:0 |
| Total | 154:32:12 |
AVF: Arteriovenous fistula, RC: Radiocephalic, BC: Brachiocephalic, BB: Brachiobasilic
Discussion
This study, focused on functional outcome of AVF at different sites indicates that AVF is a viable option in elderly patients on hemodialysis. Our findings are supported by published recommendations promoting AVF as vascular access of first choice for HD among all age groups. Literature is full of studies that have analysed age as a covariate of access survival and various other outcomes, however the conclusions and results have largely been inconclusive. There are few studies which have specifically evaluated how older age is associated with AVF outcomes.[119202122] Lin et al.[23] studied 176 AVF, and showed that age alone did not contribute to poor outcomes, they also found that combination of age with diabetes increases the risk of AVF failure. Staramos et al.[24] studied patients older than 70 years. Their experience showed similar “primary cumulative patency” rates for both grafts and AVF. Their results contradict with another large retrospective study including 494 permanent accesses in elderly patients who had previous failed access.[25] The authors found that elbow AVF have best results.
The cumulative patency rate [Tables 1 and 2] observed in our study is comparable to the literature.[262728] For example, Golledge et al.[29] found cumulative patency rates (after thrombolysis, surgical intervention or angioplasty) of 70% after first year and 63% two years later. In our study, the average one- and two-year cumulative patency for radiocephalic fistulas were 68.6% and 56.4%, respectively, and were consistent with average radiocepahlic AVF patencies of 67.3% and 56.6%, obtained from a number of studies that excluded AVF that failed to mature.[30] Our study is also consistent with a study by Konner et al.[31] comprising of 748 AVF and found excellent access survival in elderly patients. Although the most of AVF in their study were created at elbow, we can extend their results and denote that comparable survival rates can also be obtained in smaller, wrist vessels as more than one-third of AVF in our study were radiocephalic.
Based on our data we support K-DOQI recommendations for using wrist vessels first, whenever possible, before contemplating upper arm AVF creation. However, this study also demonstrated that median survival (in term of days) was almost twice as high for elbow AVF compared with wrist AVF. Dixon et al.[32] also support our data, they showed higher cumulative patency rates of 71%, 57%, and 57% at one, three, and five-year for elbow AVF as compared to 54%, 46%, and 36% for wrist AVF. Our experience with BVT is still early, and a prospective study is underway.
In our study primary patency (no intervention required) at one year was 64.7%. Similar results were published by Staramos et al. in a study of 68 elderly patients where he found one year primary patency of 67%,[24] and by Golledge et al. in their study of 107 radiocephalic fistula showing one year primary patency of 69%.[29] Therefore, these data demonstrate that, it is possible to achieve longer over-all survival and high cumulative patencies in the elderly population.
Our practice is to ensure confirmation of adequate vessel diameter and flow rates in the wrist vessels by Doppler study prior to creation of AVF in elderly patients, which may have had an impact on the outcome of AVF in this cohort. To ensure long term patency, the initial puncture should be done after at least 8 weeks of maturation and proper assessment by a nephrologist. All further punctures should be done by a well trained technician under observation of a experienced nephrologist.
In present study, failure to mature (FTM) and thrombosis are the primary reasons for loss of AVF. Pathophysiology of both is different yet somehow related to each other. Adequate flow in and out of fistula is required for its maturation, which in-turn is dependent on vessel wall integrity non-development of collaterals and absence of neo-intimal hyperplasia. One of the dreaded complications of BCF is steal syndrome, the incident of which can be reduced by making an optimal arrteriotomy. Another option is to use the proximal radial artery instead of the brachial but in our centre, a patient who is undergoing BCF is likely to have a failed distal RCF, which precludes the use of radial artery.[12]
Hereby we recognize the limitations of our study that it is a single-center experience and retrospective in nature, keeping this in view external validity of this study may be limited.
Conclusion
Age should not be a limiting factor when choosing AVF as the preferred HD access. Brachiocephalic AVF has better primary and secondary patency with higher overall median survival. However, RCF also provides reasonably good survival rates with acceptable complications in elderly population. Thrombosis and fistulas that fail to mature present as a primary concern to patients in elderly population, and demand further study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Arteriovenous fistula outcomes in the era of the elderly dialysis population. Kidney Int. 2005;67:2462-9.
- [Google Scholar]
- Chronic hemodialysis using venipuncture and a surgically created arteriovenous fistula. N Engl J Med. 1966;275:1089-92.
- [Google Scholar]
- Vascular access survival among incident hemodialysis patients in the United States. Am J Kidney Dis. 1997;30:50-7.
- [Google Scholar]
- Cost analysis of ongoing care of patients with end-stage renal disease: The impact of dialysis modality and dialysis access. Am J Kidney Dis. 2002;40:611-22.
- [Google Scholar]
- The association of initial hemodialysis access type with mortality outcomes in elderly medicare ESRD patients. Am J Kidney Dis. 2003;42:1013-9.
- [Google Scholar]
- Type of vascular access and mortality in U.S. Hemodialysis patients. Kidney Int. 2001;60:1443-51.
- [Google Scholar]
- Epidemiology and management of end-stage renal disease in the elderly. Nat Rev Nephrol. 2011;7:591-8.
- [Google Scholar]
- Patient survival following arteriovenous fistula formation. J Vasc Access. 2015;16:195-9.
- [Google Scholar]
- Renal replacement in end-stage renal disease patients over 75 years old. Am J Nephrol. 2003;23:71-7.
- [Google Scholar]
- Predictors of adequacy of arteriovenous fistulas in hemodialysis patients. Kidney Int. 1999;56:275-80.
- [Google Scholar]
- Upper extremity ischemia and hemodialysis vascular access. Eur J Vasc Endovasc Surg. 2004;27:1-5.
- [Google Scholar]
- Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. JAMA. 2007;297:286-94.
- [Google Scholar]
- Treatment and outcomes of acute coronary syndromes in India (CREATE): A prospective analysis of registry data. Lancet. 2008;371:1435-42.
- [Google Scholar]
- Association of food patterns, central obesity measures and metabolic risk factors for coronary heart disease (CHD) in middle aged Bengalee Hindu men, Calcutta, India. Asia Pac J Clin Nutr. 2003;12:166-71.
- [Google Scholar]
- Risk factors for coronary heart disease in Indians: A case-control study from Eastern India. Indian Heart J. 2005;57:738-40.
- [Google Scholar]
- Factor analysis of risk variables associated with metabolic syndrome in Asian Indian adolescents. Am J Hum Biol. 2007;19:34-40.
- [Google Scholar]
- Recommended standards for reports dealing with arteriovenous hemodialysis accesses. J Vasc Surg. 2002;35:603-10.
- [Google Scholar]
- III. NKF-K/DOQI clinical practice guidelines for vascular access: Update 2000. Am J Kidney Dis. 2001;37:S137-81.
- [Google Scholar]
- Vascular access in hemodialysis patients older than 80 years. J Vasc Surg. 2015;61:177-83.
- [Google Scholar]
- First-choice vascular access in patients over 65 years of age starting dialysis. Nephron. 1996;73:342-3.
- [Google Scholar]
- Vascular access for hemodialysis in the elderly: Results and perspectives in a geriatric population. Dial Transplant. 1985;14:560-5.
- [Google Scholar]
- Effects of age and diabetes on blood flow rate and primary outcome of newly created hemodialysis arteriovenous fistulas. Am J Nephrol. 1998;18:96-100.
- [Google Scholar]
- Patency of autologous and prosthetic arteriovenous fistulas in elderly patients. Eur J Surg. 2000;166:777-81.
- [Google Scholar]
- Lessons from 494 permanent accesses in 348 haemodialysis patients older than 65 years of age: 29 years of experience. Nephrol Dial Transplant. 1998;13(Suppl 7):73-7.
- [Google Scholar]
- Vascular access surgery managed by renal physicians: The choice of native arteriovenous fistulas for hemodialysis. Am J Kidney Dis. 2002;40:1264-76.
- [Google Scholar]
- Outcomes of upper arm arteriovenous fistulas for maintenance hemodialysis access. Arch Surg. 2004;139:201-8.
- [Google Scholar]
- Outcome of primary radiocephalic fistula for haemodialysis. Br J Surg. 1999;86:211-6.
- [Google Scholar]
- Overcoming barriers to arteriovenous fistula creation and use. Semin Dial. 2003;16:189-96.
- [Google Scholar]
- Tailoring the initial vascular access for dialysis patients. Kidney Int. 2002;62:329-38.
- [Google Scholar]
- Hemodialysis vascular access survival: Upper-arm native arteriovenous fistula. Am J Kidney Dis. 2002;39:92-101.
- [Google Scholar]







