Translate this page into:
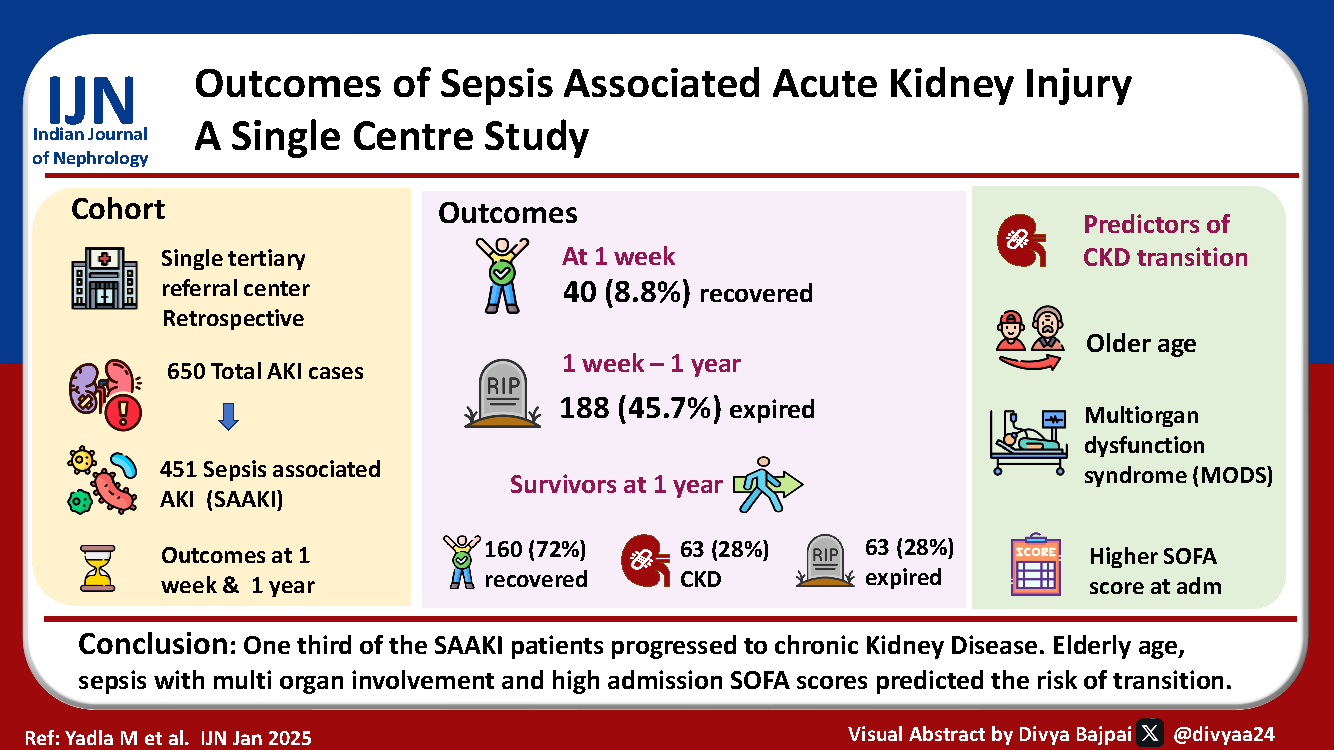
Outcomes of Sepsis–Associated Acute Kidney Injury
Corresponding author: Manjusha Yadla, Department of Nephrology, Gandhi Medical College, Hyderabad, Telangana, India. E-mail: manjuyadla@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Yadla M, Babu NM. Outcomes of Sepsis–Associated Acute Kidney Injury. Indian J Nephrol. doi: 10.25259/IJN_313_2024
Abstract
Background
Acute kidney injury (AKI) is common in tropical countries. Most common cause of AKI in India is sepsis. AKI is known to progress to acute kidney disease (AKD). Long-term follow-up of sepsis associated AKI is pivotal for identifying factors influencing progression.
Materials and Methods
We conducted a case record review of patients admitted between January 2022 and January 2023 to assess the outcomes of sepsis-AKI and the factors associated with the transition to chronic kidney disease (CKD).
Results
Of a total of 2600 renal intensive care admissions, 451 were diagnosed with sepsis-AKI. About 8.8% (40 cases) completely recovered within the first week (AKI recovered), and the remaining 91.1% cases (AKD) were followed up for 1 week to 1 year. The mortality rate between this period was about 45.7% (188 patients). On the assessment of survivors (223 patients), complete renal recovery was noted in 160 patients, and 28.3% (63 patients) transitioned to CKD. Elderly age, high SOFA score, and multiorgan failure were associated with higher progression to CKD (P < 0.05).
Conclusion
AKI patients need a follow-up period of at least 1 year, as delayed recovery is common. Sepsis-associated AKI progresses to CKD in about 28% of patients with risk factors being old age, presence of comorbidities, severe sepsis with multiorgan involvement, and high SOFA score.
Keywords
Sepsis
AKI
Long-term outcomes
CKD
Introduction
Acute kidney injury (AKI) is an independent cause of poor outcomes in critically ill patients. AKI in low-and middle-income countries (LMICs) is predominantly community-acquired. AKI is a risk factor for chronic kidney disease (CKD). The risk of CKD increases with the number of AKI episodes, with an 8-9 fold increase after an episode of AKI and a three-fold increased risk of end-stage renal disease (ESRD) during the follow-up years. In LMICs, as AKI follow-up is lacking, the risk of progression to CKD is likely underestimated.
AKI occurs in about 19% patients with moderate sepsis, 23% in severe sepsis and 51% in patients with septic shock.1 Sepsis-associated AKI (SA-AKI) is an independent predictor of increased mortality and morbidity. Adult patients with SA-AKI have a mortality rate of 60%,2 while in children, this varies from 57–60%.3 AKI is known to be associated with increased duration of hospitalization and a high healthcare cost burden. In a recent study, it was reported that the estimated annual cost of management of AKI is 1.7 billion USD.4
Sepsis-AKI is common in tropical countries like India, with a reported prevalence of 37%.5 It was estimated that 8% of AKI may transition to CKD.4 Vairakkani et al. showed SA-AKI to be the most common cause of AKI (51%).6 Understanding the progression of SA-AKI is pivotal in the prevention and reduction of CKD burden. In addition, AKI patients are at risk of cardiac and vascular complications. The study describes the clinical profile and outcomes of SA-AKI.
Materials and Methods
This was an observational study of case records of all patients with SA-AKI admitted to the critical care unit from June 2021 to September 2022 at Gandhi Medical College/Hospital, Hyderabad a public sector hospital. All patients with SA-AKI admitted to the nephrology critical care unit from June 2021 to September 2022 were included. Ethical approval was obtained.
We excluded patients whose case records were not retrievable, those with incomplete data, who left against medical advice, pregnancy-related AKI, and pediatric cases (<12 years).
Standard case definitions were considered for case identification of AKI (KDIGO 2012), AKD (ADQI 2015), SAAKI (ADQI 2022), and CKD (KDIGO 2024).7-10
As per ADQI consensus 2022, AKI diagnosed within 48 hours of diagnosis of sepsis is defined as early SA-AKI, and those diagnosed between 48 hours and 7 days of sepsis diagnosis are classified as Late SA-AKI.9
Case records of 451 patients were collected. Baseline data included age, gender, and comorbidities. Symptoms and indications of admission were recorded. Laboratory parameters on the first day of ICU admission were included. Organ dysfunction was assessed using the SOFA score. The use of invasive and noninvasive ventilation, inotropes, and renal replacement therapy were recorded.
Patients were grouped as AKI/AKD based on the duration of renal dysfunction (as per standard case definition, KDIGO 2012 and ADQI 2015).7,8 All 451 cases were diagnosed as late SA-AKI.
Details of follow-up visits at 1 year were collected from outpatient records, and their blood pressure, RFT, and eGFR (as per CKD EPI) were noted, and the risk factors for progression to CKD were assessed. As the study was designed a year later, regular records of 3-month and 6-month follow-ups are unavailable in all patients.
Statistical analysis was performed using the Statistical Package for Social Sciences software, version 21.0 (SPSS). Descriptive statistics were expressed in terms of mean and standard deviation. Association between two discrete attributes was determined by the Chi-square test. The means of the various parameters were compared using the Student’s t-test (for two groups). Multivariate logistic regression was used to identify the risk factors associated with progression to CKD. P < 0.05 was considered statistically significant.
Results
AKI was the admission diagnosis in 2.5% of the 2600 ICU admissions during the study period. Of the AKI (598) cases, 461 were associated with sepsis (77.2%). Four patients left against medical advice, and seven case records were incomplete, leaving 451 patients for analysis [Figure 1].
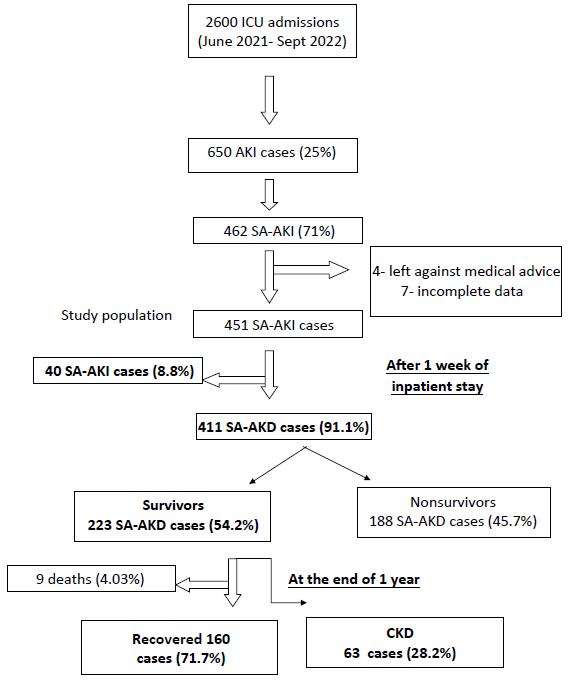
- Flowchart. AKI: Acute kidney injury, SA-AKI: Sepsis associated-acute kidney injury, SA-AKD: Sepsis associated-acute kidney disease, CKD: Chronic kidney disease.
The mean age was 48 ± 14 years with the range of 25–70 years. Men constituted 61% (275) of the study population. The major comorbidities included hypertension 259 (57.4%) and diabetes 202 (44.8%). Other comorbidities were cardiac diseases 34 (7.5%), cerebrovascular diseases 25 (5.5%), and seizure disorders 18 (3.9%) [Table 1]. The most common clinical presenting features were shortness of breath (7.4%), cough (8.8%), loose stools (8.4%) with dehydration and hypotension, fever (9.7%), seizures (2.6%), and altered sensorium (3.3%).
| Baseline characteristics | n(%)(451) |
|---|---|
| Age (Years) | 48 ± 14 |
| Gender | |
| Male | 275 (61%) |
| Female | 176 (39%) |
| Hypertension | 259 (57.4%) |
| DM | 202 (44.8%) |
| Cardiac disease | 34 (7.5%) |
| Cerebrovascular disease | 25 (5.5%) |
| Seizure disorder | 18 (3.9%) |
| Symptoms | |
| Shortness of breath | |
| Fluid overloaded state | 32 (7.4%) |
| Cough with expectoration | 40 (8.8%) |
| Fever | 44 (9.7%) |
| Loose stools | 38 (8.4%) |
| Seizures | 12 (2.6%) |
| Altered sensorium | 15 (3.3%) |
| Mean duration of hospital stay (days) | 8.4 ± 6.4 |
| Mean SOFA score at admission | 7.8 ± 2.2 |
| Etiology | |
| Sepsis with multi organ dysfunction | 146 (32.3%) |
| Pneumonia | 41 (9.09%) |
| UTI | 64 (14.1%) |
| Acute Febrile illness | 55 (12.1%) |
| Cellulitis | 23 (5.09%) |
DM: Diabetes mellitus, SOFA: Sequential organ failure assessment, UTI: Urinary tract infection
On assessment of the possible causes of AKI, sepsis with multiorgan involvement was found to be the most common (32.3%). Other primary etiologies of sepsis were urinary tract infection: 64 (14.1%) and tropical infections: 55 (12.1%), followed by pneumonia: 41 (9.09%) and cellulitis: 23 (5.09%.) [Table 2].
| Characteristics | SA-AKD (n=411) |
|---|---|
| Age (years) | 49.8 ± 13.6 |
| Gender | |
| Male | 266 (64.7%) |
| Female | 145 (35.2%) |
| Comorbid status | |
| Hypertension | 239 (58.1%) |
| DM | 189 (45.9%) |
| Cardiac disease | 31 (7.5%) |
| Cerebrovascular disease | 23 (5.5%) |
| Seizure disorder | 14 (3.4%) |
| Mean duration of hospital stay (days) | 17.5 ± 9.9 |
| Etiology of admission | |
| Mods | 134 (32.6%) |
| Pneumonia | 37 (9.0%) |
| UTI | 56 (13.6%) |
| Tropical infection | 49 (11.9%) |
| Cellulitis | 20 (4.8%) |
| Gastroenteritis | 34 (8.2%) |
| Laboratory profile | |
| Hemoglobin (g/dL) | 9.8 ± 1.3 |
| WBC count | 22230 ± 8361.4 |
| Platelets | 1.28 ± 0.23 |
| Serum creatinine (mg/dL) | 7.92 ± 2.44 |
| pH | 7.2 ± 0.1 |
| PO2 (mmHg) | 94.1 ± 15.7 |
| Serum albumin (g/dL) | 2.9 ± 0.5 |
| Mean SOFA score | 8.3 ± 3.8 |
| Inotropes support | 157 (38.1%) |
| Mechanical ventilator | 122(29.6%) |
| Blood culture positivity |
18% Gram negative bacilli (E.Coli, Klebsiella) |
| Mode of RRT | |
| Hemodialysis | 226 (54.9%) |
| Peritoneal dialysis | 101 (24.5%) |
| HD + PD | 82 (19.9%) |
| CRRT | 41 (9.9%) |
| Outcome status | |
| Survivors | 223 (54.3%) |
| Nonsurvivors | 188 (45.7%) |
DM: Diabetes mellitus, SOFA: Sequential organ failure assessment, UTI: Urinary tract infection, SA-AKD: Sepsis associated -acute kidney disease, SD: Standard deviation, RRT: Renal replacement therapy, HD: Hemodialysis, PD: Peritoneal dialysis, WBC: White blood cell count, MODS: Multi organ dysfunction syndrome
Of the 451 patients, only 40 (8.8%) had AKI, as per the definition, with complete renal recovery in less than a week. Over 90% of the study population comprised sepsis-associated acute kidney disease (SA-AKD) (411–91.1%)[Table 2].
SA-AKD group had a mean age of 49.8 ± 13.6 years, with male predominance. Hypertension and diabetes were the major comorbidities, constituting 58 and 45% of the population, respectively. MODS (32.6%), UTI (13.6%), and tropical infection (11.9%) were the major etiologies for SA-AKD [Table 2].
We observed a high SOFA score at admission (8.3 ± 3.8) due to multiorgan involvement, suggesting the severity of sepsis. Of the patients, 29.6% (122) required mechanical ventilation, and 38.1% (157) required inotropes.
A total of 226 (54.9%) patients underwent hemodialysis (HD), followed by peritoneal dialysis (PD) in 101 (24.5%) patients and a hybrid mode of HD + PD in 82 (19.9%) patients, and CRRT in 41 (9.9%) patients.
A total of 188 patients (41.6%) died during the hospital stay. Hypoalbuminemia (P = 0.03), higher mean SOFA scores (P = 0.001), and higher requirement of inotropes and mechanical ventilators [Table 3] were associated with high mortality. The presence of comorbidities such as diabetes and hypertension did not show statistically significant association with mortality (P = 0.7). Preexisting cardiac disease was not found to be associated with higher mortality (P = 0.7).
| Survival | p-value | ||
|---|---|---|---|
| Yes (n=223) | No (n=188) | ||
| Gender [n (%)] | |||
| Male | 151 (60.8%) | 115 (61.4%) | |
| Female | 72 (39.1%) | 73 (38.8%) | 0.553 |
| Age (years) | 44.39 ± 12.8 | 46.36 ± 14.99 | 0.283 |
| Comorbidities | |||
| Hypertension | 105 (47.5%) | 134 (71.2%) | 0.539 |
| Diabetes | 71 (31.9%) | 118 (62.7%) | 0.781 |
| Cardiac disease | 11 (5.3%) | 20 (10.6%) | 0.724 |
| Cerebrovascular disease | 9 (4.1%) | 14 (7.4%) | 0.497 |
| Biochemical profile | |||
| Serum creatinine (mg/dL) | 7.0 ± 4.0 | 7.1 ± 2.9 | 0.330 |
| Hemoglobin (g/dL) | 9.0 ± 1.3 | 9.2 ± 1.8 | 0.571 |
| WBC counts | 8090.79 ± 5173.76 | 11266.23 ± 17235.82 | 0.562 |
| Platelets | 1.55 ± 0.92 | 1.76 ± 0.91 | 0.853 |
| Serum albumin (g/dL) | 2.98 ± 0.45 | 2.19 ± 0.51 | 0.031* |
| Uric acid (mg/dL) | 6.03 ± 0.71 | 5.96 ± 0.69 | 0.519 |
| Mean SOFA score | 7.0 ± 2.1 | 8.4 ± 3.9 | 0.001* |
| Mechanical ventilation | 27 (12.5%) | 95 (50.5%) | 0.003* |
| Inotropes | 49 (22.4%) | 108 (57.4%) | 0.004* |
| Mode of dialysis | |||
| Hemodialysis | 143 (64.2%) | 83 (44.1%) | 0.35 |
| Peritoneal dialysis | 51 (22.8%) | 50 (26.5%) | |
| HD+PD | 43 (19.3%) | 39 (20.7%) | |
| CRRT | 13 (6.0%) | 28 (14.8%) | |
| Diagnosis | |||
| Sepsis with | |||
| MODS | 64 (28.8%) | 70 (37.2%) | 0.230 |
| Pneumonia | 18 (8.36%) | 19 (10.1%) | |
| UTI | 41 (18.6%) | 15 (7.9%) | |
| Acute Febrile illness | 33 (15.2%) | 16 (7.9%) | |
| Cellulitis | 14 (6.4%) | 6 (3.1%) | |
WBC: White blood cells, SOFA: Sequential organ failure assessment, HD: Hemodialysis, PD: Peritoneal dialysis, CRRT: Continuous renal replacement therapy, UTI: Urinary tract infection, MODS: Multiorgan dysfunction syndrome, *: P<0.05
During the follow-up period of 1 year, among 223 survivors, 9 expired, 63 (28%) progressed to CKD. The remaining 160 (71.7%) recovered, with normal GFR, serum creatinine, and urine examination. A delayed complete renal recovery was observed in 71% of the survivor group.
Among the CKD group of 63 patients, 22 (34.9%) were in Stage 4 and 8 had ESRD (12.7%). Older age, presence of diabetes, hypertension, and cardiac disease, presence of multiorgan involvement, and hypotension and ventilation requirement at admission were were associated with progression to CKD.
Discussion
Sepsis-AKI is linked to greater death rates and longer hospital stays.11 Sepsis is thought to be both a cause and a consequence of AKI. Sepsis following AKI is reported to be associated with higher mortality and length of stay.12 Our study is the first one documenting long term outcomes in SA-AKI in India. We noted complete recovery in only 40 out of 491 patients. In the majority, AKI had progressed to AKD (90%). Among the etiology of SA-AKI, sepsis with MODS followed by UTI and pneumonia were found to be common. Sepsis with MODS had a high SOFA score at admission and further was associated with high mortality. Sepsis was identified to be cause of AKI in 47.3% admissions in a study by Kolhe et al.13 Oliguric AKI was associated with greater mortality compared to nonoliguric AKI.13 High mortality with progression to AKD was also reported in a study by Flannery et al.14
Higher mortality rates were observed in high SOFA scores, severe AKI, and sepsis with MODS, a finding noted also by Gurjar et al.15 Factors associated with mortality were severe hypoalbuminemia, multiorgan involvement, and high SOFA scores.
The major risk factors associated with progression to CKD were older age, comorbid burden of hypertension, diabetes, coronary artery disease, prolonged duration of hospitalization, and initial presentation of sepsis with multiorgan involvement, with dependency on organ supports, all of which harmed renal function. Similar findings were noted by Kim et al.,16 suggesting that the elderly population, diabetes, and higher creatinine at discharge are risk factors for CKD. In the systematic review by Liu et al.,17 factors such as diabetes and hypertension, sepsis with shock predominantly abdominal infections, medications, use of vasopressors, and invasive treatments were associated with poor outcomes. Flannery et al.,14 reported that a large proportion of survivors of SA-AKI failed to return to baseline kidney function and progressed to CKD compared to sepsis without AKI.
Lopes et al.18 found that compared to patients without prior AKI, patients with sepsis-associated AKI were at greater risk for 2-year mortality. In a similar study by Gurjar et al.,15 it was observed that age and severe sepsis with high APACHE II scores were associated with high mortality.
We reiterate our observation in the above study that SA-AKI is associated with high mortality and is an independent risk factor for CKD. There is a huge need for larger group studies, longer follow-up studies, and RCTs as part of sepsis-AKI research to understand and predict the outcomes of SA-AKI.
The limitations are that we could not follow up with all the patients due to various logistical constraints. Pre-morbid serum creatinine is not available in our study group.
In conclusion, SAAKI accounts for 17% of ICU admissions and is a major cause of AKI. SA-AKI is associated with high mortality and high mean, SOFA score, and hypoalbuminemia are associated with mortality. About 28% of SA-AKI developed CKD at the end of 1-year follow-up, the major risk factors associated with progression to CKD are older age, comorbid burden of hypertension, diabetes, coronary artery disease, prolonged duration of hospitalization, and initial presentation of sepsis with multiorgan involvement.
Conflicts of interest
There are no conflicts of interest.
References
- The natural history of systemic inflammatory response syndrome. A prospective study. JAMA. 1995;273:117-123.
- [Google Scholar]
- Update on sepsis associated acute kidney injury:emerging targeted therapies. Biologic. 2016;10:149-156.
- [Google Scholar]
- The economic impact of acute kidney injury in England. Nephrol Dial Transplant. 2014;29:1362-1368.
- [CrossRef] [PubMed] [Google Scholar]
- Acute kidney injury in a tertiary care center of south India. Indian J Nephrol. 2022;32:206-215. doi: 10.4103/ijn.IJN_481_20
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Community-acquired acute kidney injury in India: data from ISN-acute kidney injury registry. Lancet Reg Health Southeast Asia. 2024;21:100359. doi: 10.1016/j.lansea.2024.100359. PMID: 38317681; PMCID: PMC10839681
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Kidney Disease: Improving Global Outcomes (KDIGO) 2021. Acute kidney injury guideline, with definition. (4)
- Acute Disease Quality Initiative (ADQI) 2015. Acute kidney disease consensus definition.
- Acute Disease Quality Initiative (ADQI) workgroup 2022- Sepsis associated acute kidney injury : consensus report of 28th workgoup.
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD work group. KDIGO 2024 clinical practice guideline for the evaluation and management of chronic kidney disease.
- Septic acute kidney injury in critically ill patients: Clinical characteristics and outcomes. Clin J AM Soc Nephrol. 2007;32:431-439.
- [Google Scholar]
- Program to improve care in acute renal disease (PICARD) study group. Sepsis as a cause and consequence of acute kidney injury: Program to improve care in acute renal Disease. Intensive Care Med. 2011;37:241-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Case mix, outcome and activity for patients with severe acute kidney injury during first 24 hours after admission to an adult, general critical care unit: Application of prediction models from secondary analysis of ICNARC case mix programme database. Crit Care. 2008;12:S2.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Sepsis-Associated acute kidney disease and long-term kidney outcomes. Kidney Med. 2021;3:507-514.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Septic acute kidney injury in critically ill Indian patients. Indian J CritCare Med. 2013;17:49-52.
- [CrossRef] [Google Scholar]
- One–year progression and risk factors for the development of chronic kidney disease in septic shock patients with acute kidney injury: a single-centre retrospective cohort study. J Clin Med. 2018;7:554.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Risk factors of sepsis associated acute kidney injury in patients with sepsis: A meta-analysis. Intensive Care Res. 2023;3:163-170.
- [CrossRef] [Google Scholar]
- Long-term risk of mortality after acute kidney injury in patients with sepsis: a contemporary analysis. BMC Nephrol. 2010;11:9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]







