Translate this page into:
Pathologic Spectrum of Kidney Diseases Associated with Snake Bites
Corresponding author: Anila Abraham Kurien, Department of Pathology, Renopath Center for Renal and Urological Pathology, Chennai, Tamil Nadu, India. E-mail: anila_abraham08@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Malathi CV, Prema K.S J, Kurien AA. Pathologic Spectrum of Kidney Diseases Associated with Snake Bites. Indian J Nephrol. doi: 10.25259/IJN_28_2025
Dear Editor,
Snake bites rarely cause acute kidney injury (AKI), and have poorly understood underlying pathology. We present 216 Indian patients who developed AKI following snake bites to demonstrate the spectrum of histopathologic findings.
The kidney pathology archives were scanned for patients with a history of snake bites who underwent kidney biopsies between 2013 and 2024. The snakebite diagnoses were based on clinical history and characteristic fang marks. Demographics and laboratory values were obtained from clinical data provided during the biopsy.
A total of 216 patients were identified. Biopsies were received from 52 centers. There were 123 males (56.9%) and 93 females (43.1%). The mean patient age was 44.7 ± 14.3 years. All patients except one presented with AKI and a 6.9 ± 3.2 mg/dL mean serum creatinine.
Of them, 211 biopsies were adequate for diagnosis. Biopsy diagnoses included acute tubular injury (ATI, n=64), acute interstitial nephritis (AIN, n=58), ATI combined with AIN (ATI/AIN, n=28), renal cortical necrosis alone (n=11), thrombotic microangiopathy (TMA, n=48), mesangio-proliferative glomerulonephritis (n=1), and IgA nephropathy with AIN (n=1) [Figure 1]. Pigmented casts were present in 32 ATI cases (50% of those with ATI), nine ATI/AIN cases (32%), and three TMA cases (6%). Immunohistochemical staining confirmed hemoglobin and myoglobin pigments in 18 and 11 cases, respectively. Two patients with ATI had both hemoglobin and myoglobin casts. Concurrent cortical necrosis was present in 23 patients with TMA (48%). Nearly all biopsies showed the absence of chronic changes. The mean global glomerulosclerosis was 7.0%. Most patients lacked interstitial fibrosis and tubular atrophy (IF/TA, 92.8%). Mild and moderate IF/TA was present in 6.2% and 1% of patients, respectively. Arteriosclerosis was seen in 18.1% of biopsies.
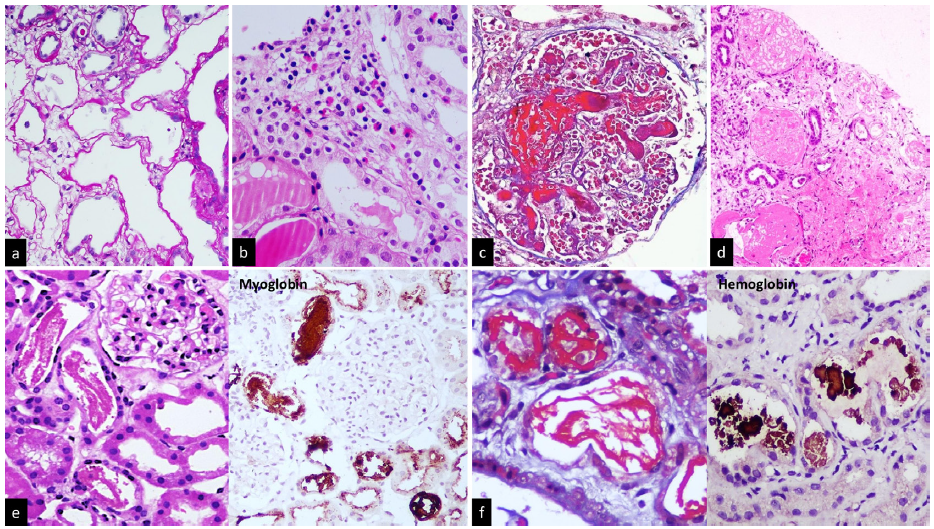
- (a) Renal tubules show features of acute tubular injury with dilated lumen, epithelial simplification and loss of apical brush border (PAS stain), (b) Acute interstitial nephritis with interstitial inflammatory infiltration comprising predominantly eosinophils and few lymphocytes (H&E stain), (c) Fibrin thrombi occluding the glomerular capillaries (Masson Trichrome Stain), (d) Coagulative necrosis of the renal cortex (H&E Stain), (e) Venom induced rhabdomyolysis with rope-like pigmented casts (PAS Stain). Myoglobin immunostain is positive in the casts, confirming the diagnosis of rhabdomyolysis associated tubular injury (Immunohistochemistry, myoglobin), (f) Intravascular hemolysis causes tubular epithelial injury with globular, beaded fuchsinophilic pigmented casts (Masson Trichrome stain). Hemoglobin immunohistochemical stain shows positivity in the tubular luminal casts (Immunohistochemistry, hemoglobin).
Snake envenoming is a serious global health issue, especially in tropical countries. Snake bites are common in rural areas owing to agricultural activities and low socioeconomic status. The clinical manifestations range from local reactions to life threatening systemic complications.
The venomous species of medical importance have varying potential to cause hemo-, myo-, or neurotoxic effects. Snake venom is a complex conglomerate of enzymes and proteins. Phospholipase A2, hyaluronidase, and metalloproteinases are some crucial constituents involved in toxicity.1 The chemical composition of the venom and timely medical intervention determine the severity and extent of the disease.2 Native medicine in India causes a disregard for the crucial antivenom administration timeframe.3
Snake bite-induced AKI shows high morbidity and mortality. The high vascularity of kidneys makes them more susceptible to snake venom. Hemodynamic alterations affecting renal perfusion, release of inflammatory cytokines, direct toxicity by venom enzymes, immunologic response, endothelial injury, or allergic reactions to anti-venom are the mechanisms involved in nephropathy [Figure 1].
Most patients developing AKI from snake bites do not get biopsied. Our study illustrates the spectrum of histopathological findings in renal biopsies following snake envenomation. AKI was the predominant nephropathy presentation, as in other studies. The mean creatinine at presentation was comparable to other studies.4
Renal pathology in snake bites can involve glomerular, tubulointerstitial or vascular compartments [Figure 2]. We predominantly encountered tubulointerstitial pathology. ATN is the common tissue diagnosis in many snake bite studies, inducing AKI, as in our study.4 The biopsies showed varying degrees of tubular epithelial cell sloughing, epithelial simplification, and luminal brush border loss. AIN was found concomitantly in a subset of cases. In biopsies, AIN featured neutrophilic, eosinophilic, and lymphocytic infiltrates. Tissue diagnosis helps in specific AIN management.
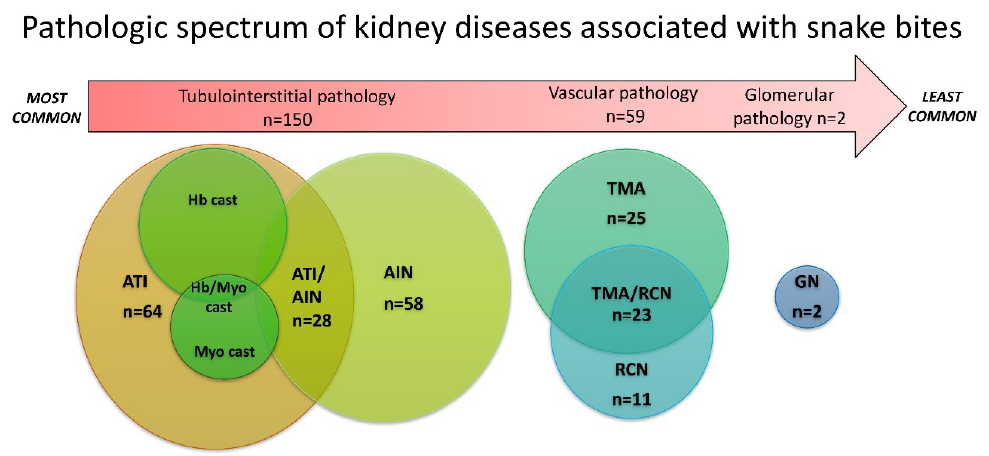
- The pathologic spectrum observed in snake bite induced kidney injury (n=211). ATI: Acute tubular injury, Hb: Hemoglobin, Myo: Myoglobin, AIN: Acute interstitial nephritis, TMA: Thrombotic microangiopathy, RCN: Renal cortical necrosis, GN: Glomerulonephritis.
Pigmented casts were witnessed in 20.8% of nephropathy cases. The myoglobin and hemoglobin pigment cast formation depicts the myotoxic and hemolytic nature of the venom, respectively. The myotoxic venom causes rhabdomyolysis and release of myoglobin into circulation, which causes direct cytotoxicity, cast formation, or renal ischemia in the kidney. Snake envenomation remained the most common etiology (21.1%- 38%) of myoglobin cast nephropathy in India.5,6 Hemotoxic snake venom can trigger intravascular hemolysis and hemoglobin pigment cast formation. A case series from India identifies snake bites as the second highest cause of hemoglobin cast nephropathy, next to Rifampicin.7 ATI and AIN were associated with hemoglobin casts. Some cases had both hemoglobin and myoglobin casts. The heterogenous biopsy features reflect the simultaneous occurrence of multiple pathologic events and the intricate chemistry of snake venom.
TMA due to snake bites can have systemic involvement but predominantly affects the kidney. TMA was the third most common pathology in renal biopsies. Previous studies have shown a 3.6-18.5% incidence of TMA in snakebite envenoming.8,9 The complex systemic effects of snake venom include disseminated intravascular coagulation, hemorrhage, hemolysis, venom-induced consumption coagulopathy and sepsis. TMA is possibly underreported due to complexity, overlap of clinical syndromes, and bias in the timing of biopsy. TMA frequently requires kidney replacement therapy. Timely management is crucial for the reversal of renal function. C3 deposition in the vessel wall was documented in snake bite-induced TMA, suggesting that snake venom activates the alternate complement pathway.4
Biopsy showed renal cortical necrosis, a lethal complication, occurred either alone or in association with TMA. Coagulative necrosis of the ischemic renal tissue could be patchy (<50% of the cortex) or extensive. Renal cortical necrosis and TMA result in adverse consequences like end-stage kidney disease or mortality. Renal biopsy assessment is valuable in prognostication.
Glomerular lesions were less common. There was one of mesangioproliferative glomerulonephritis case with mesangial C3 deposits, identified by immunofluorescence. Similar findings were documented in other studies.3 Mesangiolysis could be the plausible mechanism. One biopsy showed IgA nephropathy. None of the cases exhibited endocapillary hypercellularity, crescent formation, or fibrinoid necrosis of the capillary tuft.
In conclusion, snake bite-induced renal pathologies are diverse. Pathologic information helps expedite the specific management of snake bite-induced AKI. It also helps predict renal recovery and identify patients requiring long-term follow-up.
Conflicts of interest
There are no conflicts of interest.
References
- Clinicopathological spectrum of snake bite-induced acute kidney injury from india. World J Nephrol. 2017;6:150-61.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Snake-bite-induced acute renal failure in india. Kidney Int. 1989;35:891-907.
- [CrossRef] [PubMed] [Google Scholar]
- The kidney histopathological spectrum of patients with kidney injury following snakebite envenomation in india: Scoping review of five decades. BMC Nephrol. 2024;25:112.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Etiological spectrum and histopathological diagnosis of rhabdomyolysis associated myoglobin cast nephropathy in south india. Indian J Nephrol. 2021;31:22-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Clinical profile and outcome of pigment-induced nephropathy. Clin Kidney J. 2018;11:348-52.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Hemoglobin casts in kidney biopsies: Etiological spectrum. Indian J Nephrol. 2023;33:46-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Snakebite associated thrombotic microangiopathy: A protocol for the systematic review of clinical features, outcomes, and role of interventions. Syst Rev. 2019;8:212.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Thrombotic microangiopathy due to viperidae bite: Two case reports. Indian J Nephrol. 2017;27:161-4.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]







