Translate this page into:
Penile Calciphylaxis: A Rare Case of Penile Lesion
Address for correspondence: Dr. Kamal Kant Sahu, MD Internal Medicine, Saint Vincent Hospital, Worcester, Massachusetts 123 Summer Street, 01608, United States. E-mail: drkksahu85@gmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Dear Editor,
We read with great interest the recent article titled “Digital Gangrene in a Dialysis Patient Due to Calciphylaxis and Systemic Polyarteritis Nodosa: A Diagnostic Dilemma” by Jain etal. published in your esteemed journal.[1] With our similar experience on “penile calciphylaxis”, a rare site for calcific uremic arteriolopathy (CUA), we aim to increase the awareness amongst our readers about this rare entity.
A 53-year-old male with a medical history significant for end-stage renal disease (ESRD), on regular hemodialysis (HD) for last 2 years, coronary artery disease, diabetes mellitus type 2, and hypertension presented due to penile lesion and pain at local site of 1 month duration [Figure 1a].

- (a) Clinical image showing edematous foreskin and superficial necrosis of the glans. (b and c) CT scan in coronal view showing extensive calcification of descending aorta, renal arteries, common iliac vessels, and its branches
Computed tomography of the abdomen/pelvis revealed marked calcification of the arterial tree throughout including aorta, mesenteric arteries, renal vasculature, iliac vessels and penile vasculature [Figures 1B, C and 2B, C]. Foot X-ray done for ankle pain also showed calcified vessels [Figure 2A]. Blood test suggested hypocalcemia, hypovitaminosis D, hyperphosphatemia, and hyperparathyroidism. Considering clinical features, imaging findings of extensive vascular calcification and lab findings, a diagnosis of penile CUA was made. Currently, he is receiving regular hemodialysis, sodium thiosulphate injection, cinacalcet, and sevelamer.
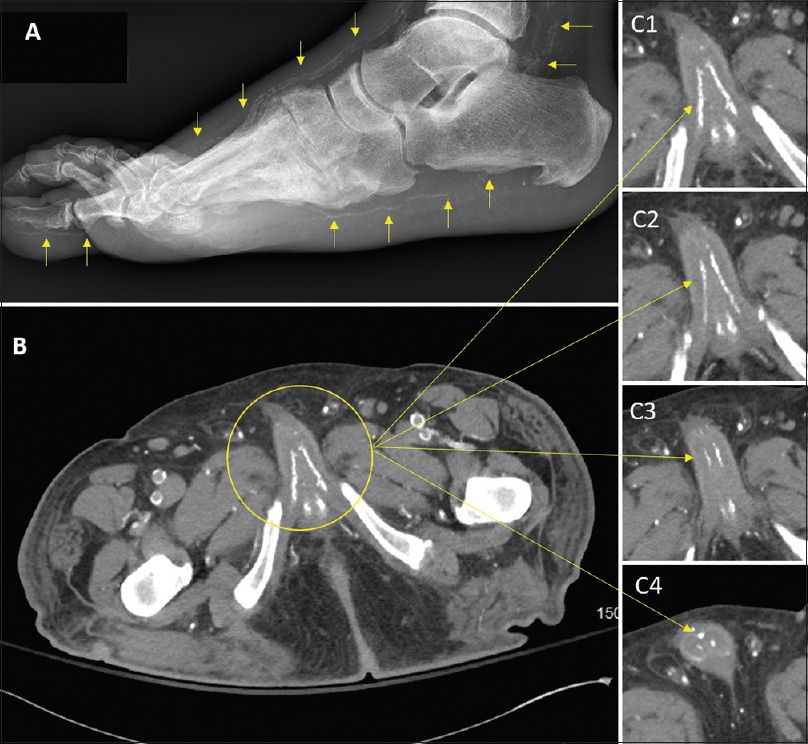
- (A) Foot X-ray showing calcification of posterior and anterior tibial arteries. (B and C) Coronal view showing calcification of penile vessels and tissues
CUA is a rare and fatal complication of ESRD commonly involving legs, abdomen, and buttocks. Penis and, breast have been rarely reported as a site of CUA in the medical literature. Other common differentials of penile lesions are balanitis, bechet's syndrome, sexually transmitted diseases, malignancy, Peyronie's disease, syringoma calcification and so on.[2] Jain et al. reported a concurrent occurrence of vasculitis and CUA in their patient which underscores the importance of considering combination of possibilities in a single case.[1] Vasculitis workup was negative in our case. Diagnosis of CUA usually involves skin biopsy, however the same is contraindicated in suspected case of penile CUA due to the fear of worsening necrosis.[3] Review on penile CUA done by Ohta et al. (17 patients) and Cohen et al. (11 patients) showed poor outcome.[45] It is important for the readers to know how to differentiate penile CUA from necrotic fasciitis and monckeberg medial calcific sclerosis.[6]
Treatment approach involves: (a) Treatment of electrolyte abnormalities with noncalcium phosphate binders like sevelamer and lanthanum (for hyperphosphatemia), cinacalcet (for hyperparathyroidism) with target Ca2+× P042+of <55 mg2/dL2(b) Injection of 25 g sodium thiosulphate intravenously thrice every week on the days of HD (c) Control of penile pain with narcotics (d) Surgical approach involves penectomy with or without parathyroidectomy (for refractory hyperparathyroidism).
The overall mortality of penile CUA has been reported as 64% by Karpman et al.[7] None of the treatments have shown better outcomes than the other.[8] Calcium deposition in vital organs can potentially compromise the system functionality.[9] Several novel therapies are being tried (hyperbaric oxygen, tissue plasminogen activator, intracavernosal prostaglandin and so on) with variable success rate.
The important take-home points from our case are: (a) All penile lesions in an ESRD on HD should be evaluated for penile CUA (b) Once common causes are ruled out, penile CUA is considered among differentials, and usually penile biopsy is not recommended (c) Despite best efforts, penile CUA is associated with high mortality rate.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Digital Gangrene in a Dialysis Patient Due to Calciphylaxis and Systemic Polyarteritis Nodosa: A Diagnostic Dilemma. Indian J Nephrol. 2019;29:143-4.
- [Google Scholar]
- Priapism as the Presenting Manifestation of Multiple Myeloma. Indian J Hematol Blood Transfus. 2017;33:133-6.
- [Google Scholar]
- Biopsy is contraindicated in the management of penile calciphylaxis. J Sex Med. 2014;11:2611-7.
- [Google Scholar]
- Penile necrosis by calciphylaxis in a diabetic patient with chronic renal failure. Intern Med. 2007;46:985-90.
- [Google Scholar]
- Necrotizing Fasciitis: Challenges in diagnosis and management. QJM 2019 Jun 28:pii: hcz163. doi: 10.1093/qjmed/hcz163. [Epub ahead of print] PubMed PMID: 31251353
- [Google Scholar]
- Penile calciphylaxis: Analysis of risk factors and mortality. J Urol. 2003;169:2206-9.
- [Google Scholar]
- Calciphylaxis: Continues to surprise. Nephrology (Carlton) 2019 Sep 4 doi: 10.1111/nep. 13643. [Epub ahead of print] PubMed PMID: 31486258
- [Google Scholar]
- Fahr's syndrome: A case of unwanted calcium in the brain. Intern Emerg Med 2019 Jun 1 doi: 10.1007/s11739-019-02119-y. [Epub ahead of print] PubMed PMID: 31154614
- [Google Scholar]






