Translate this page into:
Percutaneous injection of acrylic glue into renal allograft pseudoaneurysm for control of intractable post-biopsy hematuria
Address for correspondence: Dr. A. Lal, Department of Radiodiagnosis, Postgraduate Institute of Medical Education and Research, Chandigarh - 160 012, India. E-mail: dralal@rediffmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
We report a 44-year-old male, renal allograft recipient of 1-year duration who had two episodes of steroid responsive acute rejection. He presented with graft dysfunction for which a graft biopsy was performed and was suggestive of mixed rejection. At 2 weeks post-biopsy, patient developed severe pain over the graft site with anuria and graft hydronephrosis (HDN). The HDN and anuria intermittently settled with the passage of blood clots per-urethra. Contrast enhanced computerized tomography was suggestive of pseudoaneurysm in the graft kidney. The case was successfully managed with ultrasound guided percutaneous cyanoacrylate glue injection into the pseudoaneurysm.
Keywords
Allograft biopsy
glue
percutaneous
pseudoaneurysm
rejection
renal transplant
Introduction
Vascular injury during biopsy of renal allograft is not uncommon and poses a unique problem because of single functioning kidney that already is compromised. At times it leads to pseudoaneurysm formation and recurrent hemorrhage requiring radiological or surgical interventions. Transcatheter embolization is preferred over surgical interventions as this is less invasive and preserves the remaining functional renal tissue. Transcatheter embolization involves use of microcatheters, and coils or particulate agents as embolic agents. However, the embolization process entails use of iodinated contrast that further compromises the renal function. Also, transcatheter embolization at times may be technically challenging due to unfavorable anatomy. An alternative to transcatheter embolization is direct percutaneous access with a thin needle and injection of liquid or particulate embolic agents to occlude the aneurysm. Superficial location of graft kidney is of advantage for ultrasound (USG) and Doppler evaluation and USG-guided needle placement into the pseudoaneurysm can easily be done. Percutaneous embolization is quick and effective with minimal damage to the remaining functioning kidney and also without the added risk of contrast nephropathy.
Case Report
A 44-year-old renal allograft recipient from his wife presented with delayed graft dysfunction and underwent graft kidney biopsy. He had received no induction agent and was on tacrolimus, mycophenolate mofetil and steroids. The kidney biopsy was suggestive of acute cellular rejection-1b (ACR) and was subsequently treated with pulse methylprednisolone. Patient responded to above therapy and was discharged with serum creatinine of 1.2 mg/dl.
At 7 months post-transplant, patient had recurrence of graft dysfunction (serum creatinine 3.4 mg/dl and graft sonography examination was within normal limits). Patient underwent another graft kidney biopsy, which was suggestive of acute humoral rejection (AHR) and subsequently, patient was treated with pulse glucocorticoids and serum creatinine came back to baseline (1.2 mg/dl).
At 10 months post-transplant, patient again developed graft dysfunction (serum creatinine 5.5 mg/dl) and underwent third graft kidney biopsy and was diagnosed as ACR+AHR. Pre-procedure USG imaging was normal diagnosed with ACR + AHR. Patient was treated with pulse glucocorticoids, but serum creatinine did not improve. Patient was offered second line therapy, but he refused the treatment due to financial constraints. Two weeks post-graft kidney biopsy patient had severe pain at the graft site with acute onset anuria (serum creatinine 4.5 mg/dl). An USG examination was performed at the admission that showed massive hydronephrosis (HDN) of graft kidney (caliceal dilatation 2.5 cm). The cause of ureteric obstruction was not clear on USG. Patient was planned for percutaneous nephrostomy (PCN) of graft kidney, but while shifting to the intervention suite the patient passed about 200 ml of fresh blood mixed with blood clots per-urethra and the pelvicaliceal system decompressed with relief of pain. The procedure was terminated in view of relief of obstruction, but 36 h later patient again developed severe pain and repeat USG showed massive HDN of graft kidney filled with blood clots. Computerized tomography (CT) angiography study was performed, that confirmed the presence of HDN and a pseudoaneurysm arising from interlobar artery in the graft kidney [Figure 1]. Patient HDN again subsided spontaneously with passing of about 150 ml of blood clots. In view of imaging findings, recurrent graft HDN and passage of blood clots per-urethra, a diagnosis of intermittent bleeding from the pseudoaneurysm causing ureteric obstruction due to blood clots was made. Patient was taken up for obliteration of the pseudoaneurysm by percutaneous glue injection as the Doppler examination clearly showed the pseudoaneurysm, which appeared to be easily accessible with the percutaneous route [Figure 2].
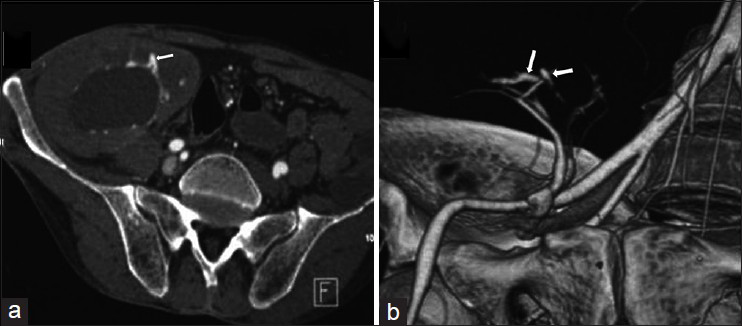
- Axial (a) and volume rendered (b) computerized tomography angiographic images show a lobulated pseudoaneurysm (arrow) arising from interlobar artery in graft kidney. Note the dilated pelvicaliceal system of renal graft in Figure 1a
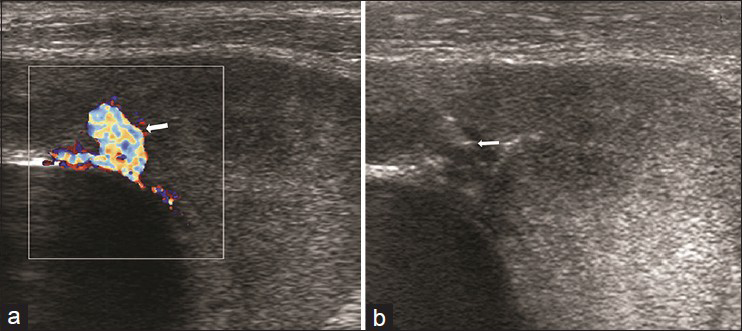
- Color-Doppler image (a) clearly demonstrates the pseudoaneurysm (arrow). Ultrasound image (b) shows spinal needle tip (arrow) within the pseudoaneurysm
A volume of 0.5 ml 1:1 mixture of N-butylcyanoacrylate (Nectaryl, Dr.ReddyLaboratories, India) and iodophendylate oil (Lipiodol, Laboratories Guerbet, France) was injected into the aneurysm through a 22G spinal needle (VygonSA, Ecouen, France). Placement of needle into aneurismal sac was USG guided and subsequent Doppler USG showed complete obliteration of blood flow in the pseudoaneurysm after the glue injection [Figures 2 and 3]. PCN was carried out after the above procedure in view of persisting anuria. Post-embolization was uneventful and the urine output (blood tinged) was 1 L/24 h through PCN and nil per-urethra. Subsequently within a couple of days, the blood clots largely cleared from the ureter and the pelvicalyceal system and patient continued to pass 1L clear urine per-urethra. Ureteric patency was confirmed with contrast injection through the PCN catheter and CT nephrostogram [Figure 4]. The PCN catheter was removed subsequently. The patient did not experience any further bouts of hematuria and was discharged 10 days after the procedure.
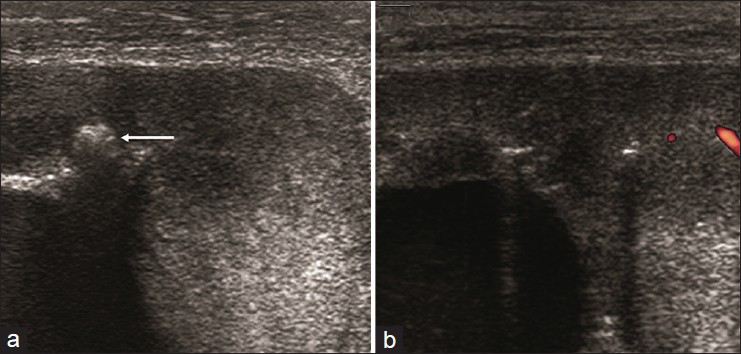
- Ultrasound image (a) shows glue cast as echogenic contents (arrow) within the aneurysm sac. Color Doppler image (b) shows no flow within the aneurysm after embolization
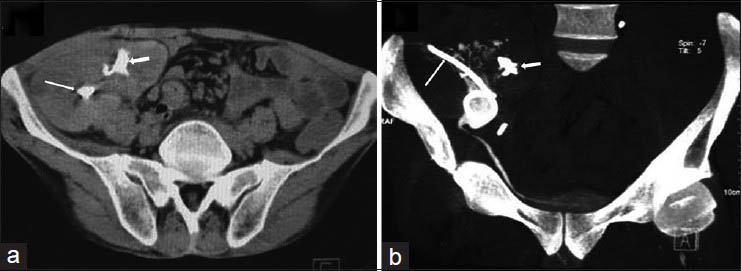
- Axial (a) non-contrast computerized tomography (CT) shows radio-opaque glue cast (shortarrow) within the pseudoaneurysm. Part of the percutaneous nephrostomy catheter (longarrow) is seen within the pelvicaliceal system. CT-nephrostogram (b) shows patency of the graft ureter. Note blood clots as filling defects within the pelvicaliceal system of graft kidney
Discussion
The incidence of complication after percutaneous renal biopsy has decreased after USG guidance and smaller gauge biopsy needles. Renal allograft biopsies are known to have a higher incidence of gross hematuria, hematoma formation and arteriovenous fistulae.[1] Hematuria requiring hospitalization and some sort of active management is seen in about 2.8% cases of graft biopsies.[2]
Renal pseudoaneurysm is a rare complication of renal biopsy, but is of great significance due to risk of rupture. The symptoms include abdominal pain with tenderness, hematuria, hypertension and shock. Endovascular selective angioembolization is the treatment of choice. Surgery may be indicated when hemostasis and repair of the arterial wall defect are required.[3]
USG-guided percutaneous injection of Gelfoam (Pharmacia and Upjohn Company, NY, USA), cyanoacrylate or other thrombogenic material into aneurismal sac is an option for cases with unfavorable vascular anatomy or patients who have contraindications for intravenous contrast agents.[45] Percutaneous thrombin injection was used for treatment of pseudoaneurysm (including renal) from 1986. However, thrombin injection may be complicated with reperfusion within the pseudoaneurysm, thromboembolic episodes and allergic reactions. Polymerization of cyanoacrylate monomers forms a glue cast and efficiently occludes the pseudoaneurysm without side effects that are experienced with thrombin. This has been successfully used for many years for endoluminal treatment of extra and intracranial vascular malformations.[3] The largest series of percutaneous embolization into renal pseudoaneurysm included 14 patients who were treated with direct injection of Gelfoam into aneurismal sac under USG guidance.[5] Thirteen patients had resolution of hematuria with no further intervention. The authors of the above study suggested that percutaneous embolization could potentially replace angioembolization as first-line treatment for renal pseudoaneurysms. We had earlier reported successful percutaneous cyanoacrylate glue injection into renal pseudoaneurysm after failed thrombin injection to control hematuria after percutaneous nephrolithotomy.[6] Our patient had severe pain abdomen secondary to bleed from renal pseudoaneurysm causing recurrent ureteric obstruction by blood clots. In this case the choice of percutaneous glue injection was influenced by the direct easy access of the pseudoanurysm, successful percutaneous embolization of previous cases and also cost-effectiveness as compared with transcatheter coil angioembolization. The choice of embolic agent was acrylic glue to minimize the chances of recanalization.
Conclusion
We report the first successful case of percutaneous acrylic glue embolization of pseudoaneurysm in a renal allograft. Percutaneous therapy should be considered as a quick and effective alternative method to transcatheter coil embolization for management of pseudoaneurysm in a renal allograft.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Evaluation of complications due to percutaneous renal biopsy in allografts and native kidneys with color-coded Doppler sonography. Clin Nephrol. 1995;43:303-8.
- [Google Scholar]
- Safety of kidney biopsy in pediatric transplantation: A report of the controlled clinical trials in pediatric transplantation trial of induction therapy study group. Transplantation. 1999;67:544-7.
- [Google Scholar]
- Postpyelolithotomy renal artery pseudoaneurysm management with percutaneous thrombin injection: A case report. Cardiovasc Intervent Radiol. 2008;31:422-6.
- [Google Scholar]
- Direct percutaneous embolization of renal pseudoaneurysm. J Endourol. 2009;23:875-8.
- [Google Scholar]
- Percutaneous cyanoacrylate glue injection into the renal pseudoaneurysm to control intractable hematuria after percutaneous nephrolithotomy. Cardiovasc Intervent Radiol. 2009;32:767-71.
- [Google Scholar]







