Translate this page into:
Physical Activity and Quality of Sleep Among Patient with Chronic Kidney Disease on Hemodialysis: A Cross-Sectional Study
Corresponding author: Nimarta Rana, Department of Medical Surgical Nursing, College of Nursing, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India. E-mail: nimartarana@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Choudhary S, Rana N, Kumar A, Bajpai NK, Gangadevi P. Physical Activity and Quality of Sleep Among Patient with Chronic Kidney Disease on Hemodialysis: A Cross-Sectional Study. Indian J Nephrol. 2024;34:350-6. doi: 10.25259/ijn_56_23
Abstract
Background:
Chronic kidney disease (CKD) patients on hemodialysis face issues like poor quality of sleep and reduced physical activity, which can impair their quality of life. This study aimed to assess the physical activity and quality of sleep among CKD patients on hemodialysis.
Materials and Methods:
This cross-sectional study was conducted at All India Institute of Medical Sciences (AIIMS), Jodhpur. Data from 66 participants selected consecutively using self-reported standardized tools, namely, Global Physical Activity Questionnaire (GPAQ) and Pittsburgh Sleep Quality Index (PSQI), were collected, along with sociodemographic variables. After receiving written informed consent, questionnaires were administered through face-to-face interviews.
Results:
The majority of the individuals, 45 (68.2%), were found to be physically active with a mean score of 2280.8 metabolic equivalents (MET)-min/week. The average PSQI score was 9.24 ± 4, and 49 (74.2%) participants had a PSQI score as higher than 5, suggesting poor quality of sleep. Physical activity and quality of sleep were found to have a significant relationship (P = 0.03). Physical activity was found to have a significant relationship with age (P = 0.01), whereas quality of sleep was associated with smoking status (P = 0.04), alcohol consumption (P < 0.01), and body mass index (BMI; P = 0.03).
Conclusion:
Contrary to many studies where CKD patients on hemodialysis were found to be physically inactive, the present study showed a substantial portion of them to be physically active. Poor quality of sleep was common; hence, interventions to promote sleep quality recommended.
Keywords
Chronic kidney disease
Hemodialysis
Physical activity
Quality of sleep
Introduction
Chronic kidney disease (CKD) is characterized by a progressive deterioration in renal function,1 ultimately leading to end-stage kidney disease (ESKD; that necessitates dialysis or transplantation for survival.2
CKD’s mortality rate increased to 41.5% between 1990 and 2017, changing its position from 17th to 12th among the leading causes of death.3 According to a survey, 17.5% of Indians have CKD, while the International Society of Nephrology’s renal disease data study center estimates that the prevalence of CKD in different parts of India ranges from 1% to 13%.4
Several issues can impair the quality of life of hemodialysis (HD) patients, including poor sleep quality and reduced physical activity due to a sedentary lifestyle and extreme exhaustion.5 It is important to analyze a patient’s physical activity to detect high-risk mortality, benefits from prevention strategies and therapeutic approaches, as well as to monitor the deterioration in physical function over time, which might indicate a new health concern.6 It was discovered that patients undergoing HD therapy had lower levels of physical activity than healthy, inactive individuals. Sedentary patients under dialysis had a 62% greater risk of death than nonsedentary ones.7
Many HD patients have poor sleep quality, which can impair a person’s health, including personal emotions, cognitive processes, motives, and capacity to focus, leading to loss of appetite, unease, worry, and despair. Inadequate sleep quantity and quality, as well as daytime dysfunction, exhaustion, and insomnia are all symptoms of sleep disorders.8
The study was conducted with the objectives to assess the physical activity and quality of sleep of CKD patients on HD.
Materials and Methods
Study design, setting, and sample size calculation
This cross-sectional study was conducted at All India Institute of Medical Sciences (AIIMS), Jodhpur, Rajasthan, India. The study population consisted of patients with CKD on HD since 3 months or more at AIIMS, Jodhpur. Consecutive patients with CKD on HD since ≥ 3 months, aged 18 years and above, willing to participate in the study, and who are able to understand Hindi or English language were included. Participants incapable of performing physical activity were excluded. The sample size was calculated by prevalence of previous study.7 The sample size was 66.
Data collection
The data was collected using standardized tools, namely, Global Physical Activity Questionnaire (GPAQ) and Pittsburgh Sleep Quality Index (PSQI), as well as sociodemographic variables in 66 participants selected by consecutive sampling.
This section consisted of description of sociodemographic variables with 19 items (age, gender, religion, educational status, marital status, occupational status, family income, residential area, smoking status, alcohol consumption, bedtime rituals, body mass index [BMI], patient on HD since, duration of HD session, HD cycles in a week, HD access, comorbid health conditions, history of renal transplantation, and laboratory indices including blood urea nitrogen, hematocrit, hemoglobin [Hb], serum albumin, serum creatinine). This section was validated by experts, and suggestions were incorporated and the tool was modified accordingly.
GPAQ is a standardized tool used to collect data on physical activity in three domains (activity at work, travel to and from places, and recreational activities) as well as sedentary behavior, comprising 16 questions (P1–P16). GPAQ is administered via face-to-face interviews.
Metabolic equivalents (METs) are commonly used to express the intensity of physical activities as well as for the analysis of GPAQ data. Total physical activity MET-min/week is equal to the sum of the total MET-min of activity computed for each setting. If P total < 600, it means that the respondent does not meet the World Health Organization (WHO) recommendations on physical activity for health and is considered inactive. If P total > 600, it means that the respondent meets the WHO recommendations on physical activity for health and is considered active. The reliability range of GPAQ is 0.53– 0.83, which is generally acceptable.9
PSQI is a standardized, self-rated questionnaire which assesses sleep quality and disturbances over a 1-month time interval in adults. The permission to use this tool was taken from the Pittsburgh University.
PSQI contains 19 self-rated questions and five questions rated by the bed partner or roommate (if available). Only self-rated questions are included in the scoring. The 19 self-rated items are combined to form seven “component” scores. The index has scores for seven items: quality of sleep, delay in falling asleep, effective duration of sleep, sleep efficacy, sleep disorders, needed amount of sleep-inducing pills, and daytime performance. Each item has a score of 0–3 (0 indicates no difficulty and 3 indicates severe difficulty) and these items give an overall score of 0–21. Score of 0 indicates no difficulty and 21 indicates severe difficulty in all areas.
The total “global” PSQI questionnaire score is calculated as the total sum of all seven groups of questions. PSQI score > 5 indicates poor quality of sleep, whereas a score ranging between 0 and 5 indicates good quality of sleep. A high score indicates poor quality of sleep, meaning they are inversely proportional. Cronbach’s alpha reliability of PSQI is 0.726.10
Ethical approval for the current study was taken from the Institutional Ethical Committee of AIIMS, Jodhpur (AIIMS/IEC/2021/3602). After receiving written informed consent, questionnaires were administered through face-to-face interviews. Each interview took about 20 min to complete.
Statistical analysis was performed by using the IBM Statistical Package for Social Sciences program (SPSS) Version 20. Descriptive statistics and inferential statistics (Fisher’s exact test and Chi-square test) were used for data analysis. Results were considered significant with P < 0.05.
Results
The sociodemographic characteristics of CKD patients on HD are shown in Table 1. Of the 66 participants, 26 (39.4%) were aged between 36 and 50 years, with male participants accounting for 39 (59.1%). Out of all participants, 50 (75.8%) were married and about 40 (60.6%) were resided in urban area. Further, a good proportion of the participants, 56 (84.8%) was nonsmokers and 56 (84.8%) did not consume alcohol. In addition, more than half of the participants 39, (59.1%) followed bedtime routines, and 15 (38.4%) of them taking bedtime milk.
| Personal variables | f (%) |
|---|---|
| Age (in years) | |
| 36–50 | 26 (39.4) |
| 18–35 | 22 (33.3) |
| >51 | 18 (27.3) |
| Gender | |
| Male | 39 (59.1) |
| Female | 27 (40.9) |
| Religion | |
| Hindu | 60 (90.9) |
| Muslim | 6 (9) |
| Education status | |
| No formal education | 9 (13.6) |
| Primary | 8 (12.1) |
| Secondary | 13 (19.7) |
| Senior secondary | 18 (27.3) |
| Graduation and above | 18 (27.3) |
| Marital status | |
| Married | 50 (75.8) |
| Unmarried | 16 (24.2) |
| Occupational status | |
| Unemployed | 22 (33.3) |
| Self-employed | 19 (28.8) |
| Homemaker | 15 (22.7) |
| Private job | 10 (15.2) |
| Family income (monthly) | |
| 10,002–29,972 | 25 (37.9) |
| ≤10,001 | 20 (30.3) |
| >49,962 | 16 (24.2) |
| 29,973–49,961 | 5 (7.6) |
| Residential area | |
| Urban | 40 (60.6) |
| Rural | 26 (39.4) |
| Smoking status | |
| Nonsmoker | 56 (84.8) |
| Ex-smoker | 10 (15.2) |
| Alcohol consumption | |
| No | 56 (84.8) |
| Yes | 10 (15.2) |
| Bedtime ritualsa | |
| Yes | 39 (59.1) |
| Take bedtime milk | 15 (38.4) |
| Listen to music | 11 (28.2) |
| Other | 13 (33.3) |
| No | 27 (40.9) |
aMultiple response questions. CKD: chronic kidney disease, f: frequency.
The clinical profile of CKD patients on HD is shown in Table 2. Half of the subjects, or 33 (50%), had a normal BMI (18.5–24.9 kg/m2). About 31 (47%) participants were on HD for 3–6 months. All participants had HD session for 3–4 h and most of them, 50 (75.8%), had two cycles of HD in a week. Arteriovenous fistula as HD access was present in 36 (54.5%) participants. Majority of the CKD patients, 61 (92.4%), had associated comorbid health conditions, with hypertension accounting for 91.8% (n = 56) of them. Lab indices showed that the mean Hb level of participants was 8.0 g/dl, which was suggestive of anemia. Blood urea nitrogen (BUN) level had an average of 49.1 mg/dl, which was increased along with S. creatinine levels of 7.3 mg/dl.
| Clinical variables | f (%) |
|---|---|
| BMI (kg/m2) | |
| 18.5–24.9 | 33 (50) |
| <18.5 | 17 (25.8) |
| 25–29.9 | 8 (12.1) |
| ≥30 | 8 (12.1) |
| Patient on HD since | |
| 3–6 months | 31 (46.9) |
| >1 year | 24 (36.4) |
| 6 months–1 year | 11 (16.7) |
| Duration of HD session | |
| 3–4 h | 66 (100) |
| HD cycles in a week | |
| Two | 50 (75.8) |
| Three | 16 (24.2) |
| HD access | |
| Arteriovenous fistula | 38 (57.6) |
| Central venous catheter | 28 (42.4) |
| Comorbid health conditionsa | |
| Yes | 61 (92.4) |
| Hypertension | 56 (91.8) |
| Others | 20 (32.8) |
| Diabetes | 11 (18) |
| No | 5 (7.6) |
| History of renal transplantation | |
| No | 65 (98.5) |
| Yes | 1 (1.5) |
| Lab indices | Mean ± SD |
|---|---|
| BUN (mg/dl) | 49.1 ± 21.7 |
| HCT (%) | 25.3 ± 4.5 |
| Hb (g/dl) | 8.0 ± 1.3 |
| S. creatinine (mg/dl) | 7.3 ± 2.7 |
| S. albumin (g/dl) | 3.3 ± 0.7 |
Figure 1 depicts the physical activity of CKD patients on HD, which is categorized as inactive (participants who do not meet the WHO recommendations for physical activity; total MET-min/week < 600) and active (participants who meet the WHO recommendations for physical activity; total MET-min/week > 600). It was found that 45 (68.2%) were active and met the WHO criteria for physical activity, whereas 21 (31.8%) were inactive.
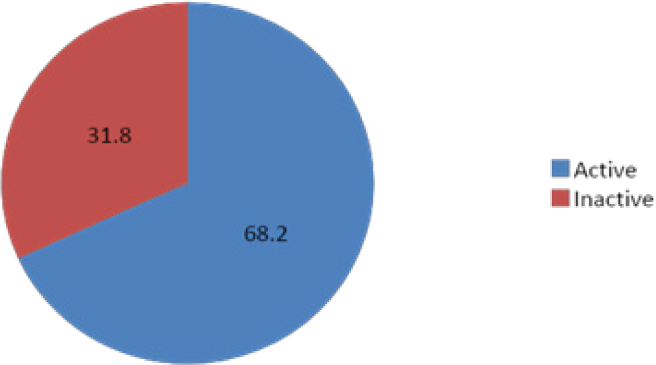
- Physical activity among CKD patients on hemodialysis. CKD: chronic kidney disease.
Table 3 shows the physical activity of CKD patients on HD in MET-min per week. The findings reveal that none of the participants were engaged in any vigorous physical activity. Participants put in an average of 1384.1 MET-min/week at work, but spent an average of 257.9 MET-min/week traveling from places. The work domain consisted majorly of household chores and physical activity at the work place. Participants spent an average of 638.8 MET-min/week on recreational activities and it included walking and yoga majorly. It was also noted that mean physical activity of male participants (2695.2 MET-min/week) was more than that of females (1815.2 MET-min/week).
| Domain | Male | Female | Overall | |||
|---|---|---|---|---|---|---|
| Mean | Median (25th-75th)a | Mean | Median (25th-75th)a | Mean | Median (25th-75th)a | |
| Work | 1402 | 420 (0–1680) | 1358 | 560 (0–2400) | 1384.1 | 490 (0–1740) |
| Travel | 342 | 120 (0–560) | 135.5 | 0 (0–80) | 257.9 | 0 (0–435) |
| Recreational activities | 951.2 | 560 (300–1260) | 357.7 | 0 (0–280) | 638.8 | 420 (0–840) |
| Total | 2695.2 | 420 (0–840) | 1815.2 | 0 (0–560) | 2280.8 | 1400 (420–3495) |
Figure 2 depicts the overall quality of sleep of 66 CKD patients on HD as per their total PSQI score (0–21). A good proportion of participants, 49 (74.2%), had poor quality of sleep with a total PSQI score of more than 5, whereas 17 (25.8%) participants had a good quality of sleep with a PSQI score between 0 and 5.
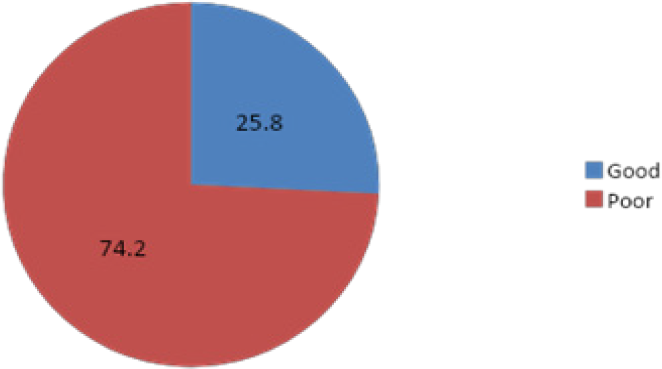
- Quality of sleep among CKD patients on HD. CKD: chronic kidney disease; HD: hemodialysis.
Table 4 shows that there was a substantial (P = 0.03) relationship between physical activity and quality of sleep among CKD patients on HD. The data indicate that the majority of inactive patients, 19 (90.4%), and more than half of active patients, 30 (66.6%), had poor quality of sleep, which is consistent with the significant link established between physical activity and quality of sleep.
| Physical activity | Quality of sleep | Total | P | |
|---|---|---|---|---|
| Poor f (%) | Good f (%) | |||
| Inactive | 19 (90.5) | 2 (9.5) | 21 | 0.03* |
| Active | 30 (66.7) | 15 (33.3) | 45 | |
| Total | 49 | 17 | 66 | |
Table 5 shows the association between physical activity and quality of sleep with the sociodemographic variables among CKD patients on HD. Among all the sociodemographic variables studied, age was found to have a significant relationship (P = 0.01) with physical activity. Quality of sleep and certain sociodemographic characteristics, such as smoking status (P = 0.04), alcohol intake (P < 0.001), and BMI (P = 0.03), were negatively associated.
| Sociodemographic variables | Physical activity | Quality of sleep | ||||
|---|---|---|---|---|---|---|
| Active f (%) | Inactive f (%) | P | Good f (%) | Poor f (%) | P | |
| Personal variables | ||||||
| Age (in years) | ||||||
|
18–35 36–50 >51 |
20 (30.3) 15 (22.7) 10 (15.2) |
2 (3) 11 (16.7) 8 (12.1) |
0.01** |
9 (13.6) 5 (7.6) 3 (4.5) |
13 (19.6) 21 (31.8) 15 (22.7) |
0.24 |
| Gender | ||||||
|
Male Female |
30 (45.5) 15 (22.7) |
9 (13.6) 12 (18.2) |
0.10 |
12 (18.2) 5 (7.6) |
27 (40.9) 22 (33.3) |
0.39 |
| Religion | ||||||
|
Hindu Muslim |
41 (62.1) 4 (6.1) |
19 (28.8) 2 (3) |
0.53 |
17 (25.8) 0 (0) |
43 (65.2) 6 (9) |
0.49 |
| Educational status | ||||||
|
Secondary Senior secondary Graduation and above No formal education |
15 (22.7) 13 (19.7) 13 (19.7) 4 (6.1) |
6 (9.1) 5 (7.6) 5 (7.6) 5 (7.6) |
0.26 |
6 (9.1) 4 (6.1) 6 (9.1) 1 (1.5) |
15 (22.7) 14 (21.2) 12 (18.2) 8 (12.1) |
0.56 |
| Marital status | ||||||
|
Married Unmarried |
36 (54.5) 9 (13.6) |
14 (21.2) 7 (10.6) |
0.45 |
13 (19.7) 4 (6.1) |
37 (56.1) 12 (18.1) |
0.67 |
| Occupational status | ||||||
|
Unemployed Self-employed Private job Homemaker |
15 (22.7) 15 (22.7) 8 (12.1) 7 (10.6) |
7 (10.6) 4 (6.1) 2 (3) 8 (12.1) |
0.22 |
4 (6.1) 8 (12.1) 2 (3) 3 (4.5) |
18 (27.2) 11 (16.6) 8 (12.1) 12 (18.1) |
0.65 |
| Family income (monthly) | ||||||
|
≤10,001 10,002–29,972 >29,973 |
18 (27.3) 17 (25.8) 10 (15.1) |
6 (9.1) 8 (12.1) 7 (10.6) |
0.63 |
6 (9.1) 6 (9.1) 5 (7.6) |
18 (27.3) 19 (28.7) 12 (18.2) |
0.18 |
| Residential area | ||||||
|
Rural Urban |
17 (25.8) 28 (42.4) |
9 (13.6) 12 (18.2) |
0.78 |
10 (15.2) 7 (10.6) |
16 (24.2) 33 (50) |
0.08 |
| Smoking status | ||||||
|
Nonsmoker Ex-smoker |
37 (56.1) 8 (12.1) |
19 (28.8) 2 (3) |
1.00 |
12 (18.2) 5 (7.6) |
44 (66.6) 5 (7.6) |
0.04** |
| Alcohol consumption | ||||||
|
No Yes |
36 (54.6) 9 (13.6) |
20 (30.3) 1 (1.5) |
0.15 |
10 (15.2) 7 (10.6) |
46 (69.7) 3 (4.5) |
<0.001** |
| Bedtime ritualsa | ||||||
|
No Yes |
15 (22.7) 30 (45.5) |
12 (18.2) 9 (13.6) |
0.10 |
5 (7.6) 12 (18.2) |
22 (33.3) 27 (40.9) |
0.39 |
| Clinical variables | ||||||
| BMI (kg/m2) | ||||||
|
<18.5 18.5–24.9 >25 |
14 (21.2) 23 (34.8) 8 (12.1) |
3 (4.5) 10 (15.2) 8 (12.1) |
0.26 |
9 (13.6) 6 (9.1) 2 (3) |
8 (12.1) 27 (40.9) 14 (21.2) |
0.03** |
| Patient on HD since | ||||||
|
3–6 months 6 months–1 year >1 year |
21 (31.8) 9 (13.6) 15 (22.7) |
10 (15.2) 2 (3) 9 (13.6) |
0.57 |
8 (12.1) 2 (3) 7 (10.6) |
23 (34.8) 9 (13.6) 17 (25.8) |
0.93 |
| HD cycle in a week | ||||||
|
Two Three |
39 (59.1) 6 (9.1) |
14 (21.2) 7 (10.6) |
0.10 |
16 (24.2) 1 (1.5) |
37 (56.1) 12 (18.1) |
0.06 |
| HD access | ||||||
|
AV fistula Central venous catheter |
29 (43.9) 16 (24.2) |
9 (13.6) 12 (18.2) |
0.26 |
11 (16.7) 6 (9.1) |
27 (40.9) 22 (33.3) |
0.50 |
| Comorbid health conditionsa | ||||||
|
No Yes |
4 (6.1) 41 (62.1) |
1 (1.5) 20 (30.3) |
1.00 |
2 (3) 15 (22.7) |
3 (4.5) 46 (69.7) |
0.59 |
Table 6 shows that there was a substantial (P = 0.03) relationship between physical activity and quality of sleep among CKD patients on HD. The data indicate that the majority of inactive patients, 19 (90.4%), and 66.6% (n = 30) of the active patients had poor quality of sleep, which is consistent with the significant link established between physical activity and quality of sleep.
| Physical activity | Quality of sleep | Total | P | |
|---|---|---|---|---|
| Poor f (%) | Good f (%) | |||
| Inactive | 19 (90.5) | 2 (9.5) | 21 | 0.03* |
| Active | 30 (66.7) | 15 (33.3) | 45 | |
| Total | 49 | 17 | 66 | |
Discussion
CKD has a significant impact on the patient’s body, particularly as it progresses to its final stage. HD procedure overwhelms the patient’s condition, affecting general physical condition, sleep, and lifestyle. WHO recommends that adults of age 18–64 years should perform at least 150 min of moderate-intensity aerobic physical activity like walking or at least 75 min of vigorous-intensity activity in a week or an equivalent combination of both. The activities performed should be at least 10 min long.11 This criterion was followed in the current study by using GPAQ. The physical activity assessed by using GPAQ showed that 68.2% of the participants in this study were physically active and met WHO’s recommendation, while 31.8% were inactive, which is similar to the findings by Bossola et al.,12 where 56.2% patients on chronic HD were active and 43.8% were inactive. The data of the aforementioned study was also collected by self-reported measures.
On the contrary, our findings differ from those of earlier studies that assessed physical activity in HD patients which suggested that the majority of the study participants were physically inactive. Filho et al. conducted a study on 108 HD patients to examine their level of physical activity using the International Physical Activity Questionnaire (IPAQ), with the results revealing that 77.8% of the participants were sedentary.7 But in our study, the HD patients turned out to be physically active, contradicting many of the previous studies. But there are high chances of recall bias as it was assessed by a self-reported questionnaire. The participants did physical activity mostly when doing household chores and at their workplace if they were self-employed. A few of the participants did yoga and walking, but none of them followed any routine exercise regimen. All the participants performed moderate-intensity exercises only. In epidemiological terms, the data of the current study can be viewed from the perspective that reveals prevalence of poor quality of sleep in 74.2% participants, evident by their high PSQI score (6–12), which is consistent with the findings of most publications on the same population.8,10,13-15 The study findings are congruent to those of a study by Samara et al., which revealed that 76.65% of the subjects had poor sleep quality, scoring more than 5 points on PSQI.10
In the present study, physical activity and quality of sleep were found to be significantly associated with each other. In another study by Theodorou et al.,2 the interrelationship between physical activity and quality of sleep was observed. Han M et al. also found in their study that patients were less active on dialysis days and experienced a poor quality of sleep.16 Therefore, our results are in concordance with those of similar studies.
In the present study, physical activity turned out to be significantly associated with age (P = 0.01), which is similar to some other studies that have shown positive correlation between age and fatigue level. On the other hand, there was no association of physical activity with education, occupation, marital status, and residential area. Contrary to our findings, place of residence, educational level, and employment status affected the fatigue level in HD patients. Patients residing in urban area were more fatigued compared to residents of suburban area. Unemployed patients and homemakers were more fatigued in comparison to self-employed patients and civil servants. According to the aforementioned study, marital status did not significantly affect the fatigue indices, which is in line with our findings. Also, women seemed to be more “tired” than men, which is similar to our findings as the overall mean physical activity MET score of women (617.1) was lesser than that of men (898.6).17
The current study shows negative association of quality of sleep with smoking status (P = 0.04), alcohol consumption (P < 0.01), and BMI (P = 0.03), whereas no association was found between quality of sleep with gender and HD cycle in a week. Many similar studies performed in the same field showed no relation with gender and quality of sleep, which is in line with the results of our study.10 In the same study, it was found that overweight and obese patients’ quality of sleep was poorer than that of those with normal BMI. In our study, quality of sleep also showed significant association with BMI. But there have been many similar studies which did not find any link between the two.10 In the present study, HD cycle in week did not have any association with quality of sleep, which aligns with the results of other similar researches. But Cengic et al. observed that more weekly dialysis sessions were linked to poor quality of sleep.18
A few limitations of the study should be mentioned. The study was confined to CKD patients on HD at a single center with a small sample size; hence, generalizability of the study findings is limited. Due to memory recall bias, the responses of participants may not have been accurate.
Conclusion
The sleep characteristics of HD patients should be assessed on a regular basis. Low quality of sleep and lack of physical activity have an impact on a person’s quality of life. Despite their importance, their significance may be disregarded because most patients do not adequately communicate symptoms that have a negative influence on their health required.
Further research is recommended to gain a better understanding of the causes attributed to reduced quality of sleep and for appropriate selection of interventions for these patients.
Acknowledgement
The authors appreciate the friendly cooperation of patients.
Conflicts of interest
There are no conflicts of interest.
References
- Chronic kidney disease: symptoms and causes. Available from: https://www.kidney.org/atoz/content/about-chronic-kidney-disease. [Last accessed on 2017 Dec 15]
- Physical activity and quality of sleep in patients with end-stage renal disease on hemodialysis: A preliminary report. Sleep Disord. 2020;2020:6918216. doi: 10.1155/2020/6918216
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Kidney disease statistics for the united states. Available from: https://www.niddk.nih.gov/health-information/health-statistics/ kidney-disease. [Last accessed on 2021 Jun 14]
- Prevalence and risk factors of chronic kidney disease in overweight and obese population in a tertiary 62 care hospital in north India. Saudi J Kidney Dis Tranpl. 2019;30:1431-8.
- [CrossRef] [PubMed] [Google Scholar]
- Preliminary study of an exercise programme for reducing fatigue and improving sleep among long-term haemodialysis patients. Singapore Med J. 2014;55:476-82.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Assessing physical function and physical activity in patients with CKD. Clin J Am Soc Nephrol. 2013;8:861-72.
- [CrossRef] [PubMed] [Google Scholar]
- Physical activity level of patients on hemodialysis: A cross-sectional study. Fisioter Pesqui. 2016;23:234-40.
- [Google Scholar]
- Sleep quality in patients undergoing long-term hemodialysis using the pittsburgh sleep quality index. Nephro-Urol Mon. 2017;9:e13137.
- [Google Scholar]
- Validity and reliability of the global physical activity questionnaire (GPAQ) Measurement Phys Educ Exerc Sci. 2013;17:221-35.
- [Google Scholar]
- An assessment of sleep quality and daytime sleepiness in hemodialysis patients: A cross-sectional study from Palestine. Sleep Sci Pract. 2019;3:4.
- [Google Scholar]
- Physical activity in hemodialysis patients measured by triaxial accelerometer. Biomed Res Int. 2015;2015:645645. doi: 10.1155/2015/645645
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Self-reported physical activity in patients on chronic hemodialysis: correlates and barriers. Blood Purif. 2014;38:24-9.
- [CrossRef] [PubMed] [Google Scholar]
- Sleep quality, daytime sleepiness and health-related quality-of-life in maintenance haemodialysis patients. J Int Med Res. 2016;44:698-709.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Depression and quality of sleep in maintenance hemodialysis patients. Srp Arh Celok Lek. 2014;142:437-43.
- [PubMed] [Google Scholar]
- Quality of sleep and its relationship to quality of life in hemodialysis patients. J Caring Sci. 2013;2:295-304.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Quantifying physical activity levels and sleep in hemodialysis patients using a commercially available activity tracker. Blood Purif. 2016;41:194-204.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of fatigue in end stage renal disease patients undergoing hemodialysis: Prevalence and associated factors. Med Arch. 2015;69:376-80.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Quality of sleep in patients undergoing hemodialysis. Int Urol Nephrol. 2012;44:557-67.
- [CrossRef] [PubMed] [Google Scholar]







