Translate this page into:
Plasma cell myeloma in a renal transplant recipient: A case report and review of literature
Address for correspondence: Dr. Seema Sharma, Type V B/ 13, SGPGI Campus, Raebareli Road, Lucknow-226 014, Uttar Pradesh, India. E-mail: ssharma@sgpgi.ac.in
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Post-transplant lymphoproliferative disorders are mostly B-cell neoplasms that develop as a consequence of immunosuppressive therapy. Plasma cell myeloma occurring after solid organ transplant is rare. We report here a case of plasma cell myeloma variant of post-transplant lymphoproliferative disorders developing after 15 months of live related renal transplant in a 41-year-old female. We compare clinicopathological features of this case with few cases reported in literature.
Keywords
Renal transplant
myeloma
PTLD
Introduction
Post-transplant lymphoproliferative disorders (PTLD) encompass a heterogeneous spectrum of conditions ranging from reactive plasmacytic hyperplasia to malignant lymphoma. The overall incidence of PTLD is about 1.5% in all solid organ transplant recipients.[1] Multiple myeloma is rarely seen after solid organ transplantation , estimated as <4% of all PTLD.[2] In a large series of PTLD after renal transplants, the incidence of myeloma was reported as 0.2%.[3] There are single case reports of plasma cell myeloma PTLD that meet the criteria for myeloma as defined in the nontransplant-related cases. We report case of multiple myeloma in a 41-year-old female presenting 15 months after renal transplantation.
Case Report
In March 2006, a 41-year-old female with chronic renal failure secondary to diffuse glomerulosclerosis with crescents received a renal transplant from her 39-year-old sister. She had 3 HLA antigen match with her sister. After transplant, she was placed on triple immunosupression - cyclosporine, prednisolone, and mycophenolate mofetyl. In post-transplant period, she showed no evidence of rejection. She complained of severe back pain in upper dorsal vertebral region 2 months after transplant. Her bone scan showed increased tracer uptake over D5 vertebra due to collapse, which was thought likely to be secondary to steroid-induced osteonecrosis. She was advised conservative management by bed rest and bracelet belt.
In May 2007 (15 months after renal transplant), she was admitted for investigation of pain in back radiating to right lower limb and bone pain. Her laboratory investigation findings were as follows: Hb 12.5g/dL, TLC 10,500/uL, platelet 225,000/uL, serum creatinine 1.4 mg/dL, serum calcium 8.9 mg/dL, phosphate 3.59 mg/dL, total serum protein 8.9 mg/dL and serum albumin 4.4 mg/dL, serum β-2 microglobulin 3.5 mg/L. MRI [Figure 1] spine showed partial destruction of L4 and L2 with a soft tissue mass on thecal sac and right half of sacrum. Epstein-Barr virus (EBV) serology was negative. A biopsy from soft tissue mass at sacrum and bone marrow trephine was done. Bone marrow aspirate revealed 60% plasma cells and trephine biopsy showed diffuse infiltration by plasma cells [Figure 2]. Biopsy from sacral mass also showed plasmacytoma. Serum electrophoresis and immunofixation revealed Ig A lambda monoclonal paraprotein (2.54 g/dL).
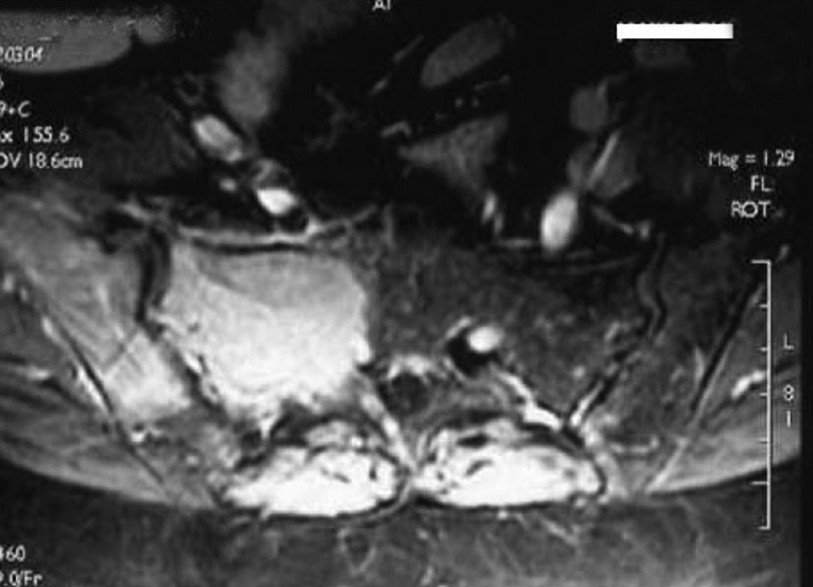
- Large homogenous enhancing soft tissue mass is seen in right half of sacrum, right iliac blade and patchy oval enhancing lesion seen on left iliac balde on post contrast scan
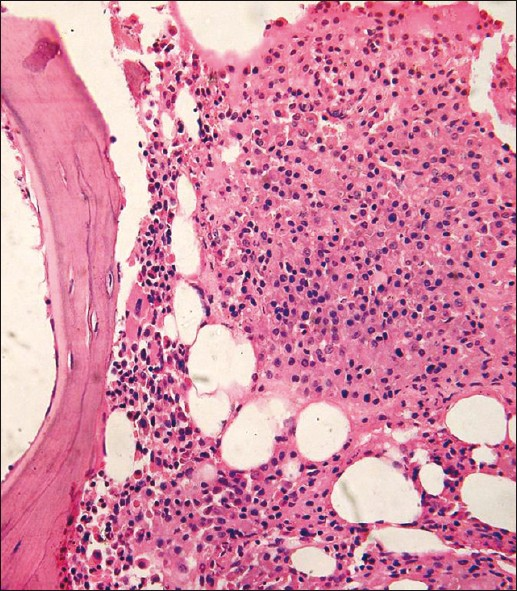
- Bone marrow biopsy showing diffuse infiltration by plasma cells (H and E, ×100)
She was started on VAD (vincristine 0.4 mg/day, adriamycin 9 mg/m2, and dexamethasone 40 mg/day) regimen. After completion of six cycles of chemotherapy, repeat bone marrow showed residual disease with 25% plasma cells though serum electrophoresis did not show M band. Her graft function was normal though proteinuria persisted. She was started on second line of drugs - thalidomide in dose of 100 mg bid and continued on triple immunosupression regimen. She is alive after 2 years and still in follow-up.
Discussion
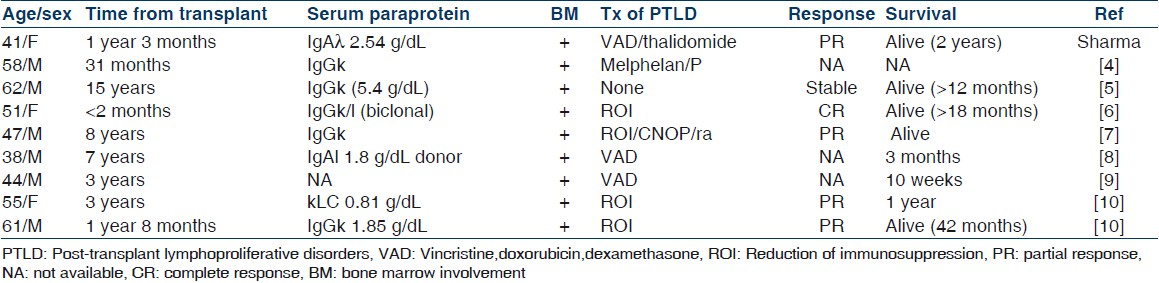
PTLD are mostly Epstein-Barr virus-related, B-cell tumors that develop as a consequence of immunosuppressive therapy in recipients of solid organ or bone marrow transplants. These disorders range from reactive, polyclonal plasmacytic hyperplasia to those that are morphologically and genotypically indistinguishable from typical non-Hodgkin's lymphomas. Cacciola et al.[4] reported the first case of myeloma in a renal transplant patient. Plasma cell myeloma occurring after renal transplant is extremely rare. In a large series of PTLD after renal transplants, the incidence of myeloma was reported as 0.2%.[2] In case reports, it is usually reported 2-7 years after transplantation.[4–10] In some case reports, myeloma and polymorphic PTLD have been reported in <2 months to 15 years following solid organ transplant. Passweg et al.[6] have reported transient multiple myeloma within 2 months of kidney transplant [Table 1].
We here present a rare case of PTLD myeloma that developed within one and half years after renal transplantation. The possibility of missed myeloma at the time of renal transplant was thought of but no evidence of bone pain and tenderness before transplant, native kidney biopsy was suggestive of diffuse global sclerosis with crescents and no evidence of myeloma cast nephropathy and relatively young age of patient did not favor it. The odd features for myeloma include sciatic pain suspected as postherpetic neuralgia, and nuclear bone scan study suggestive of steroid-related osteonecrosis, proteinuria without cast nephropathy or amyloidosis, or light chain deposit disease on graft biopsy. This possibility though may not be entirely excluded as on literature search, we found a single case report by Sirsat et al.[11] of multiple myeloma presenting as proliferative (crescentic) glomerulonephritis.
This is the first case of multiple myeloma in renal transplant recipients among the 1628 patients transplanted from our center. The diagnosis of multiple myeloma was based on the presence of IgA monoclonal band in serum and urine, bone lesion in the form of collapse of D4 vertebra, plasmacytoma in iliac bone mass lesion, bone marrow biopsy, and aspiration study. The increased incidence of neoplasia in renal transplant recipients is well documented and can be due to the effect of immunosuppressive state.[12]
Shiel et al.[2], who reviewed more than 4000 renal transplant recipients over a period of 19 years, documented one case of myeloma among 167 nonskin malignancies. Howard et al.[12] described a patient in whom the diagnosis of multiple myeloma was confirmed following the histological demonstration of light chain nephropathy as the cause of graft dysfunction. In our case, the patient was presented with back pain, sciatica on right side without motor paralysis, and on evaluation had compression fracture of D4 vertebrae and tumor mass in iliac bone.
Patients with multiple myeloma, who have been transplanted with their disease in remission, have been observed to develop a recurrence of the disease in the allograft. Although myeloma is rare after transplantation, monoclonal gammopathies are seen frequently. Radl et al.[13] reported 30% incidence of monoclonal immunoglobulin abnormalities in patients undergoing immunosuppressive treatment after renal transplantation.
We classified this case as plasma cell myeloma PTLD as it showed all the clinical, laboratory, and radiologic features of myeloma as defined in nontransplant setting. The routine treatment of myeloma includes oral prednisolone and melphelan therapy, but in patients with renal involvement VAD regimen is better than melphalan and prednisolone regimen. The prognosis of IgA λ type is poor compared to those who had IgG κ type chain excretion. The response to chemotherapy is poor with IgA myeloma. Recent studies demonstrate the benefits of lenalidomide, a more potent and less toxic analogue of thalidomide, and the proteasome inhibitor bortezomib for the treatment of relapsed/refractory multiple myeloma, as well as initial therapy. High-dose chemotherapy followed by autologous stem cell transplantation has become the preferred treatment for younger patients.[14] However this option in our patient could not be considered because of financial constrains. Our patient is alive and in follow-up after 2 years of diagnosis though has shown partial response to therapy.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Clinicopathologic features of post transplant lymphoproliferative disorders. Ann Transplant. 1997;2:33-40.
- [Google Scholar]
- Cancer incidence in renal transplant patients treated with azathioprine or cyclosporine. Transplant Proc. 1987;19:2214-6.
- [Google Scholar]
- Myeloma, Hodgkin disease, and lymphoid leukemia after renal transplantation: characteristics, risk factors and prognosis. Transplantation. 2006;81:888-95.
- [Google Scholar]
- Multiple myeloma in a renal transplant recipient. Nephrol Dial Transplant. 1992;7:447-9.
- [Google Scholar]
- Transient multiple myeloma after intense immunosuppression in a renal transplant patient. Nephrol Dialysis Transplant. 1993;8:1393-4.
- [Google Scholar]
- Demonstration of Epstein-Barr virus in a case of multiple myeloma after renal transplantation. Haematologica. 2000;85:773-4.
- [Google Scholar]
- IgA myeloma of donor origin arising 7 years after allogeneic renal transplant. Br J Haematol. 2000;108:592-4.
- [Google Scholar]
- Multiple myeloma : a rare maliganacy in post transplant period. Indian J Nephrol. 2001;11:66-7.
- [Google Scholar]
- Post-transplant plasma cell myeloma and polymorphic lymphoproliferative disorder with monoclonal serum protein occurring in solid organ transplant recipients. Mod Pathol. 2004;17:389-94.
- [Google Scholar]
- Multiple myeloma presenting as proliferative (crescentic) glomerulonephritis. J Postgrad Med. 1994;40:92-3.
- [Google Scholar]
- Occurrence of multiple myeloma three years after successful renal transplantation. Am J Kidney Dis. 1987;10:147-50.
- [Google Scholar]
- Monoclonal gammopathies in patients undergoing immunosuppressive treatment after renal transplantation. Clin Immunol Immunopathol. 1985;37:98-102.
- [Google Scholar]
- Advances in multiple myeloma treatment: lenalidomide and bortezomib. Commun Oncol. 2009;6:53-8.
- [Google Scholar]







