Translate this page into:
PMMA Hemofilter in Patients with Sepsis/Septic Shock Requiring Renal Replacement Therapy in Comparison with Conventional Dialysis
Corresponding author: Santosh Kumar Ambekar, Department of Nephrology, Kamineni Academy of Medical Sciences and Research Center, Hyderabad, Telangana, India
-
Received: ,
Accepted: ,
How to cite this article: Ambekar SK, Vemuri SP, Suresh I. PMMA Hemofilter in Patients with Sepsis/Septic Shock Requiring Renal Replacement Therapy in Comparison with Conventional Dialysis. Indian J Nephrol. doi: 10.25259/ijn_442_23
Abstract
Background
Acute kidney injury (AKI) due to sepsis is associated with a high mortality rate. Exaggerated inflammatory response plays a major role in sepsis and is also associated with poor prognosis. Efficient removal of cytokines can improve the outcomes of these patients. Continuous hemofiltration can modulate systemic and tissue immune activation. We define the impact of the polymethylmethacrylate (PMMA) hemofilter in comparison with conventional dialysis in patients with sepsis.
Materials and Methods
It is an observational retrospective study of 32 patients with sepsis/septic shock from January 2020 to August 2023. Subjects were divided into Group A (PMMA hemofilter–HEMOFEELTM) and Group B (regular dialysis filter), with 16 subjects in each group. The standard treatment guidelines were followed. The parameters such as vasopressor requirement, SOFA scores, and serial measurements of IL-6, CRP, and procalcitonin were assessed.
Results
Group A subjects showed statistically significant improvement in systolic (p <0.001) and diastolic blood pressure (p=0.002) and a reduction in the mean SOFA score (p<0.001) after treatment. Interleukin-6, procalcitonin, and CRP showed statistically significant reduction (p<0.001) post-treatment in Group A. The PMMA hemofilter led to an increase in SBP and DBP, reduction in CRP, procalcitonin and lactate, drop in inotropes use, as well as lower mortality.
Conclusion
The use of cytokine adsorption technique using the PMMA hemofilter decreased vasopressor requirements, SOFA score, and showed reduction in inflammatory markers. Large-scale randomized controlled studies are needed to assess the clinical efficacy of these filters.
Keywords
Septic shock
Cytokine storm
PMMA hemofilter
Introduction
Cytokines play an important role in the pathology and genesis of sepsis and septic shock.1 Sepsis activates the innate immune system, leading to cascade activation of the cytokines. Proinflammatory cytokines like TNF-alpha, IL-1, and IL-6 cause increased TH 1 and TH 17 cell phenotype, increased vascular permeability, cellular infiltration into the organs, recruitment and activation of neutrophils, a cascade leading to further inflammation, tissue destruction, and further loss of function of the tissues with the end result being multiple organ failure. Anti-inflammatory cytokines–IL4, IL-10, IL-11, IL-13, TGF-BETA-TH2 cells, and TREG cells get activated, leading to decreased production of proinflammatory cytokines, suppression of TH1 cells, and reduced recruitment of inflammatory cells.2 Removal of cytokines has been shown to exert a therapeutic effect with remarkable recovery from sepsis.3 Recent literature has supported the application of high-volume hemofiltration (HVHF), which has the capability to remove excess humoral mediators,4 and it has been widely applied in the treatment of septic shock.5 Polymethyl methacrylate (PMMA) is has protein adsorption function that removes various inflammatory cytokines.6 In a study in patients with septic shock, the use of the PMMA hemofilter led to early improvement in hemodynamics, hypercytokinemia and blood lactate levels.7 Similar studies using Cytosorb® showed reduction in vasopressor requirement and inflammatory markers.8,9 Studies from Japan applied the PMMA continuous hemodiafiltration and noted improvement in both hypercytokinemia and dysoxia.10,11 Kishikawa et al. found that in comparison with the polysulfone (PS) membrane, PMMA had the capacity to adsorb around 79% of the cytokines more efficiently.6
A study from India found that early and timely use of PMMA hemofilters in severe COVID19 effectively reduced the cytokine storm.7 We studied the use of PMMA hemofilter in relation to conventional hemofilter in the removal of cytokines, especially focused on sepsis and septic shock cases.
Materials and Methods
This retrospective study was done at the Department of Nephrology, Kamineni Hospitals Hyderabad, Telangana, India, from January 2020 to August 2023 after approval by the Institutional ethical committee. It included 32 patients diagnosed with sepsis/septic shock, AKI with volume overload, severe metabolic acidosis, and electrolyte abnormalities, which could not be corrected by medical management, requiring renal replacement therapy (RRT). Septic shock was defined according to The American College of Chest Physicians/Society of Critical Care Medicine (ACCP/SCCM) consensus criteria established in 1992.12 The standard treatment guidelines for sepsis and acute kidney injury (AKI) requiring RRT have been followed. Thirty-two subjects were divided into Group A (PMMA hemofilter–HEMOFEELTM) and Group B (regular dialysis filter), with 16 subjects in each group. The subjects in Group B were the patients who were diagnosed with sepsis/septic shock and underwent RRT before the availability of the PMMA hemofilter. Vasopressor requirement, SOFA scores, and serial measurements of IL-6, CRP, and procalcitonin were assessed. Patients with severe heart failure (New York Heart Association: NYHA class IV) were excluded. All patients underwent sustained low-efficiency dialysis (SLED)/extended duration dialysis (EDD).
Statistical analysis
Categorical data were represented as frequencies and proportions. Chi-square test and Fischer’s exact test were used as appropriate. Yates correction was applied wherever chi-square rules were not fulfilled. Normality of the continuous data was tested by Kolmogorov–Smirnov test and the Shapiro–Wilk test. Continuous data were represented as mean and standard deviation. Independent t-test was used as the test of significance to identify the mean difference between groups. P-value of <0.05 was considered statistically significant. MS Excel and SPSS version 22 (IBM SPSS Statistics, Somers NY, USA) were used to analyze the data.
Results
The duration of the dialysis sessions in the PMMA group was 8–12 hours, requiring one to three sessions, whereas in the conventional group, the dialysis sessions were for 8–12 hours, requiring 1–4 sessions. All parameters were assessed before the initiation of dialysis and after the final session of dialysis. Acinetobacter Spp, followed by E. coli and Klebsiella spp were isolated in most cases. The relevant data are enclosed in the Supplementary Files.
In Group A, the mean SBP was 89.38 ± 12.37 mmHg before dialysis, which was lower than the mean SBP of 91.25 ± 23.06 mmHg in Group B. After dialysis, both groups experienced an increase in mean SBP, and this increase was more pronounced in Group A, with a mean SBP of 128.13 ± 14.24 mmHg, compared to 98.75 ± 24.19 mmHg in Group B. Similarly, Group A had a pre-dialysis DBP value of 57.50 ± 10.65 mmHg, slightly lower than the mean DBP of 58.75 ± 12.58 mmHg in Group B. After dialysis, both groups experienced an increase in mean DBP, but Group A exhibited a greater increase, with a mean DBP of 73.75 ± 5.00 mmHg, compared to 61.88 ± 13.28 mmHg in Group B. These results demonstrate that the use of the PMMA hemofilter led to a substantial and statistically significant increase in SBP (p <0.001) and DBP (p= 0.002) when compared to conventional dialysis [Table 1].
| Subjects (N=32) | Group A (N=16) | Group B (N=16) | p-valuea | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
|
SBP (in mmHg) |
Pre-dialysis | 89.38 | 12.37 | 91.25 | 23.06 | 0.776 |
| Post-dialysis | 128.13 | 14.24 | 98.75 | 24.19 | <0.001* | |
| p-valueb | <0.001* | 0.097 | ||||
|
DBP (in mmHg) |
Pre-dialysis | 57.50 | 10.65 | 58.75 | 12.58 | 0.764 |
| Post-dialysis | 73.75 | 5.00 | 61.88 | 13.28 | 0.002* | |
| p-valueb | <0.001* | 0.352 | ||||
a: Independent t-test, b: Paired t-test, * Statistically significant, SBP: systolic blood pressure, DBP: diastolic blood pressure
Vasopressor requirement
We compared the need for noradrenaline (NA) and vasopressin (VP) pre- and post-dialysis. Prior to dialysis, [Figure 1] 93.8% of individuals in Group A and 75.0% in Group B required NA. After dialysis, these percentages decreased to 37.5% in Group A and 68.8% in Group B. There was a greater reduction in the need for NA in Group A. Half of the individuals in both groups required VP before dialysis. However, after dialysis this proportion decreased to 12.5% in Group A and increased to 56.3% in Group B. We also assessed the doses of both NA and VP and noted that only the group receiving the PMMA hemofilter exhibited a significant reduction in dosage after dialysis. When comparing the two groups, the statistical significance in dosage reduction was observed exclusively after PMMA dialysis (NA: p =0.004, VP: p=0.029) [Table 2].
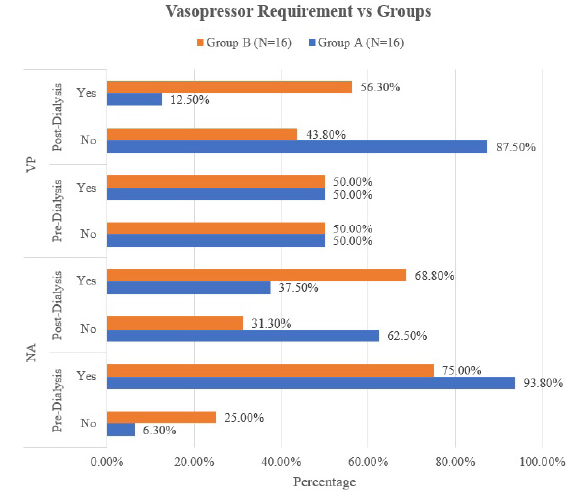
- Bar diagram comparing the requirement of vasopressors before and after the dialysis among the study subjects between the groups, Na: Noradrenaline, VP: Vasopressin.
| Subjects (N=32) | Group A (N=16) | Group B (N=16) | p-valuea | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
|
NAc (in mL/h) |
Pre-dialysis | 12.31 | 7.39 | 10.63 | 8.15 | 0.544 |
| Post-dialysis | 3.00 | 5.66 | 14.44 | 13.46 | 0.004* | |
| p-valueb | <0.001* | 0.076 | ||||
|
VPd (in mL/h) |
Pre-dialysis | 1.31 | 1.42 | 1.13 | 1.20 | 0.699 |
| Post-dialysis | 0.38 | 1.05 | 1.29 | 1.20 | 0.029* | |
| p-valueb | 0.011* | 0.381 | ||||
a: Independent t-test, b: Paired t-test, c: Each milliliter of NA contains 160 mcg of NA, d: Each milliliter of VA contains 1 unit of VA, * Statistically significant, NA: noradrenaline, VP: vasopressin.
SOFA score
Before dialysis, the mean SOFA score in Group A and B were 13.50 ± 2.63 and 12.00 ± 4.47 respectively. No significant difference was observed between the two groups. Following dialysis, Group A exhibited a significant reduction in the mean SOFA score, with a mean value of 7.75 ± 5.03. Conversely, Group B experienced a substantial increase in the SOFA score (14.06 ± 4.97). The comparison between the two groups revealed a statistically significant difference (p<0.001) [Table 3].
| Subjects (N=32) | Group A (N=16) | Group B (N=16) | p-valuea | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| SOFA | Pre-dialysis | 13.50 | 2.63 | 12.00 | 4.47 | 0.257 |
| Post-dialysis | 7.75 | 5.03 | 14.06 | 4.97 | 0.001* | |
| p-valueb | <0.001* | 0.024* | ||||
a: Independent t-test, b: Paired t-test, * Statistically significant, SOFA- Sequential Organ Failure Assessment
Laboratory parameters
Before dialysis, the mean IL-6 level was notably high at 953.55 pg/mL. However, following the cytokine adsorption with hemofeel dialyzer, there was a significant reduction in IL-6 (99.49 ± 146.49 pg/mL). The mean C-reactive protein (CRP) level showed a substantial decrease from an initial value of 40.63 ± 10.50 mg/dL before dialysis to 14.25 ± 9.52 mg/dL after dialysis. The PMMA hemofilter lowered the mean procalcitonin levels from a baseline value of 42.53 ± 33.41 ng/mL to 6.66 ± 6.21 ng/mL [Table 4].
| Group A (N=16) | Pre-Dialysis | Post-Dialysis | p-value# | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
|
Interleukin-6 (in pg/mL) |
953.55 | 725.93 | 99.49 | 146.49 | <0.001* |
|
C-Reactive protein (in mg/dL) |
40.63 | 10.50 | 14.25 | 9.52 | <0.001* |
|
Procalcitonin (in ng/mL) |
42.53 | 33.41 | 6.66 | 6.21 | <0.001* |
#Paired t-test, * Statistically significant, PMMA : polymethylmethacrylate
Clinical outcome
The mortality rate among subjects who received the PMMA hemofilter (Group A) was 31.3%, which was considerably lower compared to the mortality rate of 75.0% in Group B [Figure 2].
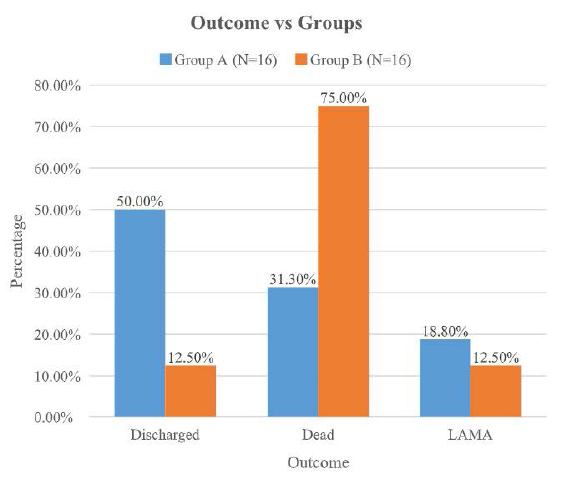
- Bar diagram comparing the clinical outcome based on mortality status among the study subjects between the groups. LAMA - left against medical advice.
Discussion
Septic shock has been found to be associated with high mortality and has been associated with AKI. The only modality left over to remove the cytokine burden from the blood is through the application of HVHF, which can remove the inflammatory mediators. The PMMA hemofilter is known to increase high arterial pressure, and decrease lactate levels, procalcitonin, and CRP. The appearance of low level of cytokines has been noted after the application of PMMA hemofilter.
The present study found that the application of the PMMA hemofilter is associated with an increase in SBP and DBP, compared to conventional dialysis. Our results were supported by a study done by Matsumura et al., which found a significant improvement in the hemodynamics and survival rate in septic shock patients with the application of the PMMA hemofilter.13 The main priority in sepsis is to maintain the hemodynamics through fluid resuscitation, and inotropic and vasopressor therapy.14 In our study, we noticed that the dosage of ionotropes had significantly reduced in both dialysis groups. We would like to emphasize that the application of the PMMA hemofilter has shown more prominent results, reducing the use of inotropes in a significant manner compared to conventional dialysis.15
High SOFA score indicates the severity of sepsis. It has been associated with the poor outcome of the treatment. Our study revealed that the application of the PMMA hemofilter has been seen associated with low SOFA score with better survival rate compared with conventional dialysis. A study from Nakada also pointed out the importance of SOFA score reduction and better survival rate in a study conducted in Japan.15 Similarly, we have noticed prime reduction in hematological sepsis markers such as CRP, procalcitonin along with the lactate.13 A reduction in the mortality rate has been noticed in Group A than in Group B, indicating the importance of using the PMMA hemofilter. Our results were supported by a study conducted by Sakamoto et al. which found a significant reduction in death rate through the application of the PMMA hemofilter.16
Conclusion
PMMA hemofilter improved clinical outcomes, decreased vasopressor requirements, and showed significant reduction in inflammatory markers in patients with sepsis and septic shock and AKI. PMMA hemofilter could be a promising treatment modality in tackling the cytokine storm. Larger randomized trials are needed to define the potential benefits of this new treatment modality in addition to standard treatment protocols in sepsis/septic shock.
Conflicts of interest
There are no conflicts of interest.
References
- Physiology and immunology of the cholinergic antiinflammatory pathway. J. Clin. Invest. 2007;117:289-96.
- [CrossRef] [PubMed] [Google Scholar]
- Immunomodulatory therapies in sepsis. Intensive Care Med. 2000;26:S124-8.
- [CrossRef] [PubMed] [Google Scholar]
- High-volume haemofiltration in human septic shock. Intensive Care Med. 2001;27:978-86.
- [CrossRef] [PubMed] [Google Scholar]
- Continuous hemodiafiltration with cytokine-adsorbing hemofilter in the treatment of severe sepsis and septic shock. Contrib. Nephrol. 2007;156:365-70.
- [CrossRef] [PubMed] [Google Scholar]
- Comprehensive analysis of cytokine adsorption properties of polymethyl methacrylate (PMMA) membrane material. J Artif Organs. 2022;25:343-9.
- [CrossRef] [PubMed] [Google Scholar]
- Early and timely use of hemofiltration therapy with poly methyl meth acrylate (PMMA) filters in severe COVID-19 adult respiratory distress syndrome patients: A Single centre study in India. Int J Med Sci Clinical Res Studies. 2023;3:2717-22.
- [CrossRef] [Google Scholar]
- Hemoadsorption with CytoSorb in septic shock reduces catecholamine requirements and in-hospital mortality: A single-center retrospective “genetic” matched analysis. Biomedicines.. 2020;8:539. Available from: http://dx.doi.org/10.3390/biomedicines8120539
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Experience with hemoadsorption (CytoSorb®) in the management of septic shock patients. World J Crit Care Med. 2020;9:1-12.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Continuous hemodiafiltration with PMMA Hemofilter in the treatment of patients with septic shock. Mol Med. 2008;14:257-63.
- [CrossRef] [PubMed] [Google Scholar]
- Continuous hemodiafiltration with cytokine-adsorbing hemofilter in the treatment of severe sepsis and septic shock. ContribNephrol. 2007;156:365-70.
- [CrossRef] [Google Scholar]
- Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM consensus conference committee. American college of chest physicians/society of critical care medicine. Chest. 1992;101:1644-5.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of septic shock with continuous HDF using 2 PMMA hemofilters for enhanced intensity. Int J Artif Organs. 2012;35:3-14.
- [CrossRef] [PubMed] [Google Scholar]
- Continuous hemodiafiltration with PMMA Hemofilter in the treatment of patients with septic shock. Mol Med. 2008;14:257-63.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Selection of acute blood purification therapy according to severity score and blood lactic acid value in patients with septic shock. Indian J Crit Care Med. 2010;14:175-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]








