Translate this page into:
Post-renal transplant Kaposi's sarcoma of skin
Address for correspondence: Dr. Dinesh N. Gera, Department of Nephrology and Clinical Transplantation, Institute of Kidney Diseases and Research Center - Dr. H L Trivedi Institute of Transplantation Sciences [IKDRC-ITS], Civil Hospital Campus, Asarwa, Ahmedabad - 380 016, Gujarat, India. E-mail: dineshgera@ymail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
A 35-year-old male underwent live-related renal transplantation in December 2005, his mother was a donor. His pre-transplant serology was negative for hepatitis B surface antigen and for anti-hepatitis C virus as well as anti-human immunodeficiency virus antibody. His plasma IgG for cytomegalovirus (CMV) was positive and IgM was negative indicating previous infections by CMV. Human Herpes virus-8 (HHV-8) testing was not performed in the donor or the recipient. Transplantation was without any complication. He was on triple immunosuppressant and maintaining baseline serum creatinine of 1.5 mg/dL. In August 2010, he was admitted with graft dysfunction and on renal biopsy was found to have tacrolimus toxicity with chronic allograft nephropathy. His tacrolimus dose was reduced to 3 mg/day and he was discharged with serum creatinine of 2.5 mg/dL.
In March 2011, he presented with well-defined elevated violacious nodular lesions on middle and ring finger of left hand for 2 months, there were two nodules on both fingers [Figure 1]. There were no other similar lesions anywhere on the body. There was no history of hemoptysis or melena. This time his serum creatinine was 4.5 mg/dl and was on tacrolimus 3.0 mg/day; mycophenolate (MMF) 1.5 g/day; and prednisolone 10 mg/day. Skin biopsy showed proliferation of small- to medium-sized vessels lined by endothelial cells suggestive of Kaposi's sarcoma (KS) [Figure 2]. His chest X-ray and computed tomography scan of thorax and abdomen were normal. HHV-8 testing was not carried out. The immunosuppressive therapy was tapered to prednisolone 10 mg daily, tacrolimus and MMF were totally withdrawn. Radiation therapy was delivered by linear accelerators in dose of 3 Gy per fraction for a total of 10 fractions. He responded well to the treatment and all his lesions regressed. At present he is on maintenance hemodialysis and is enrolled in deceased donor transplant waiting list.

- Well-defined elevated violecious nodular lesions on dorsal aspect of middle and ring finger of left hand
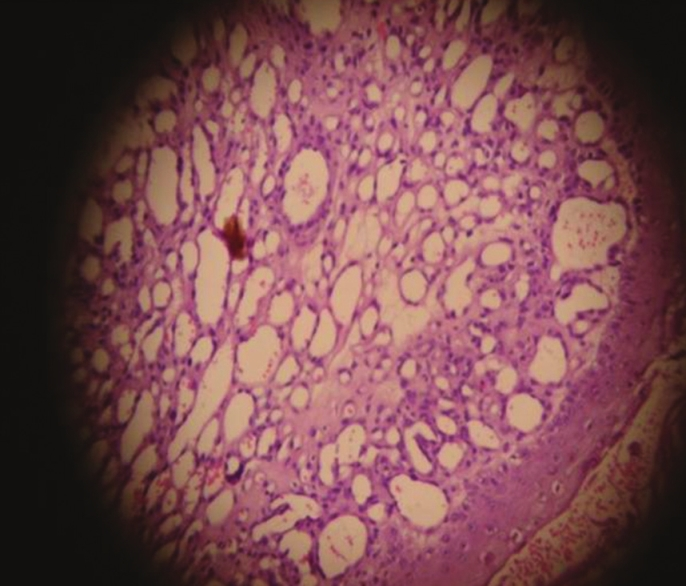
- Photomicrograph showing proliferation of small- to medium-sized vessels lined by endothelial cell and spindle-shaped cells suggestive of Kaposi sarcoma
KS is a soft tissue cancer arising from endothelial cells of blood vessels involving; skin, lymph node, gastrointestinal tract, and lungs; characterized histologically by endothelial-lined vascular spaces and spindle-shaped cells.[1] Rare in general population, risk of its development is substantially increased in immuno-compromised persons like patients with acquired immune deficiency syndrome, solid organ transplant recipients, and in patients on chemotherapy for lymphoma.[2] Genetic predisposition and ethnic difference in incidence has been reported. It is endemic in African countries, has higher prevalence in people of Arabian countries and other Mediterranean descent, but it is rare in Indian ethnicity.[2] Infection with HHV-8 is very commonly associated with patients of KS, antibody against this virus are found in 70-90% of immune-compromised patients and in about 100% of non-immunocompromised patients having KS.[3] The incidence of KS in transplant recipients correlates with prevalence of HHV-8 in general population.[4] A small Indian study screened 108 samples of sera from blood bank for HHV-8 antibody and reported prevalence of 4%.[4] In healthy population, prevalence of HHV-8 is 11% in USA, 12% in Thailand, and 15% in Malaysia.[4]
First case of post-renal transplant KS in India was reported in 1998 from Kerala.[5] There is scarcity of data and rarity of occurrence of post-transplant KS in the Indian continent. Onset of KS usually occurs within first 2 years of transplantation. Here, we report a case of KS of skin in a renal transplant recipient occurring after 5 years of transplantation and was successfully treated with withdrawal of immunosuppressant and local radiotherapy.
Acknowledgment
The authors would like to acknowledge Hargovind L. Trivedi, and Aruna V Vanikar, for their contribution and permission to publish the case report.
References
- Viral infections affecting the skin in organ transplant recipients: Epidemiology and current management strategies. Am J Clin Dermatol. 2006;7:13-29.
- [Google Scholar]
- Seroprevalence of Human herpesvirus 8 (HHV-8) and incidence of Kaposi's sarcoma in Iran. Infect Agent Cancer. 2011;6:5.
- [Google Scholar]
- Human herpesvirus-8 (Hhv-8) comparative sero-prevalence in U.S.A., India, Thailand, Malaysia, and its association with malignancies. J Acquir Immune Defic Syndr Hum Retrovirol. 1998;17:A25.
- [Google Scholar]






