Translate this page into:
Rare Histologic Coexistence of Infection-Related Glomerulonephritis and Thrombotic Microangiopathy
Corresponding author: Anila Abraham Kurien, Department of Pathology, Renopath, Center for Renal and Urological Pathology, Chennai, Tamil Nadu, India. E-mail: anila_abraham08@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Malathi CV, Prema KS J, Aralapuram K, Krishnamoorthy V, Kurien AA. Rare Histologic Coexistence of Infection-Related Glomerulonephritis and Thrombotic Microangiopathy. Indian J Nephrol. 2025;35:109-10. doi: 10.25259/IJN_304_2024
Infection-related glomerulonephritis (IRGN) is the result of an immune-mediated glomerular injury following an extra-renal infection. Thrombotic microangiopathy (TMA) is characterized by microangiopathic hemolytic anemia, thrombocytopenia, and fibrin thrombi in the microvasculature leading to ischemic tissue injury. TMA in renal biopsy occurs due to diverse pathological conditions. Simultaneous occurrence of IRGN and TMA in the kidney biopsy is extremely rare.1 We detected this combination in renal biopsies of two patients.
A 26-year-old female presented with anuria, pedal edema, and new onset hypertension. The patient is a known diabetic who developed upper respiratory tract infection 2 weeks back. Baseline blood investigations showed anemia (Hb–9.8g/dl), leukocytosis (14.99×103/µl), and mild thrombocytopenia (140×103/µl). The patient had elevated serum creatinine (7.8mg/dl), antistreptolysin O titer (407IU), and hypocomplementemia (C3–21.9mg/dl).
The second patient, a 65-year-old male, who is hypertensive and nondiabetic, presented with oliguria and pedal edema. Patient had skin infection 1 month back. Patient had worsening serum creatinine (5.82→10.91mg/dl) and hypocomplementemia (C3–36 mg/dl).
Hemodialysis was initiated in both patients, and renal biopsy was performed. Light microscopy of the two renal biopsies [Figures 1 and 2] had diffuse endocapillary hypercellularity and neutrophilic infiltrate in the glomeruli, consistent with IRGN. Fibrin thrombi were seen occluding some of the afferent arterioles. There were no features of chronic renal parenchymal injury in both biopsies. Immunofluorescence (IF) study showed coarse granular positivity of C3 and IgG along the glomerular capillary loops and mesangium.
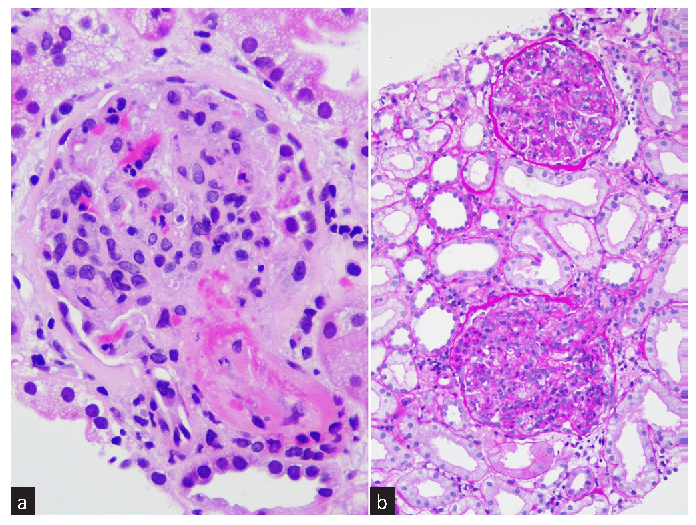
- Renal biopsy of patient 1. (a) Fibrin thrombus occludes the afferent arteriole and some of the capillary lumen. There is endocapillary hypercellularity and neutrophilic infiltration in the capillary tuft (H&E, ×400). (b) The glomeruli show diffuse and global endocapillary hypercellularity, consistent with IRGN (PAS ×100). IRGN: Infection-related glomerulonephritis, H&E: Hematoxylin and eosin, PAS: Periodic acid-Schiff.
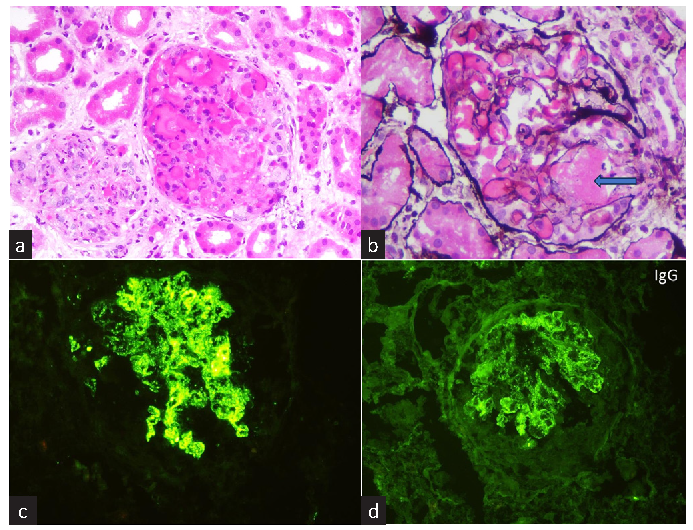
- Renal biopsy of patient 2. The glomerulus on the right shows dilated and congested capillaries with fibrin thrombus in some segments. (a) The glomerulus on the left displays endocapillary hypercellularity and neutrophilic influx (H&E ×200). (b) Fibrin indicated by blue arrow, occludes the afferent arteriole (Jones silver, ×400). (c and d) Immunofluorescence study demonstrates granular deposits of C3 (+3) and IgG (+2), respectively, on the glomerular capillary loops and mesangium, H&E: Hematoxylin and eosin.
The subsequent workup in the first case confirmed the presence of atypical hemolytic uremic syndrome (aHUS). Peripheral smear revealed microcytic erythrocytes, schistocytes, leukocytosis, and thrombocytopenia. LDH (342.7 U/l) was raised. Autoimmune workup was negative. The patient attained remission with antibiotics and steroids. There were no features of TMA in the clinical and laboratory evaluation of the second patient. Blood count showed leukocytosis (19.05×103/µl). Hemoglobin, platelet count, liver function test, and anticomplement factor H assays were within normal limits. TMA appears to be renal-limited. The patient improved clinically following steroid therapy.
TMA is associated with glomerular diseases, mainly IgA nephropathy, ANCA-associated vasculitis, membranous nephropathy, focal and segmental glomerulopathy, and C3 glomerulopathy.2 Cases of IRGN with histologic evidence of TMA in renal biopsy are limited.1,3-5
Both these diseases are mediated through the alternative complement pathway. aHUS is hypothesized to occur in persons with a genetic predisposition and subsequent activation of complement by a variety of causes, infection being a known trigger. Complement activation and endothelial injury could be the underlying mechanism for the deposition of fibrin in the renal microvasculature.1
The prognosis and outcome of IRGN in adults is guarded. Almost all the patients documented with aHUS with IRGN have recovered. The time taken for normalization of renal parameters ranged from 3 weeks to 1 year.1,3-5 The limited data available suggest that long-term eculizumab therapy for this form of aHUS is not warranted.1
The identification of TMA was incidental in our cases, as there was no clinical suspicion during the initial presentation. The two cases illustrate that TMA may complicate IRGN in adults. Careful histologic evaluation is essential to recognize this rare complication obscured in the setting of IRGN.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
References
- Post-streptococcal glomerulonephritis associated with atypical hemolytic uremic syndrome: To treat or not to treat with eculizumab? Clin Kidney J. 2016;9:90-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Thrombotic microangiopathy and the kidney. Clin J Am Soc Nephrol. 2018;13:300-17.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Hemolytic uremic syndrome complicating postinfectious glomerulonephritis in the adult. Am J Kidney Dis. 1995;25:336-9.
- [CrossRef] [PubMed] [Google Scholar]
- Simultaneous postinfectious glomerulonephritis and thrombotic microangiopathy: A renal biopsy study. Am J Kidney Dis. 1998;31:513-20.
- [CrossRef] [PubMed] [Google Scholar]
- Acute poststreptococcal glomerulonephritis associated with thrombotic microangiopathy in an adult. Clin Nephrol. 2000;54:169-73.
- [PubMed] [Google Scholar]







