Translate this page into:
Relapsing Calciphylaxis of the Breast: Glucocorticoids – Friend or Foe?
Corresponding Author: Ravikiran Shankarappa T, No 80, 2nd Cross, 3rd Main, Income Tax Layout, Attiguppe, Bengaluru – 560 040, Karnataka, India. E-mail: ravinay91@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Shankarappa TR, Jairam A, Kedlaya PG, Satish R. Relapsing Calciphylaxis of the Breast: Glucocorticoids – Friend or Foe? Indian J Nephrol. 2024;34:522-3. doi: 10.4103/ijn.ijn_201_23
Abstract
Calciphylaxis is a rare life-threatening condition characterised by systemic medial calcification of arterioles causing tissue ischemia with subsequent necrosis. Calciphylaxis occur in areas of increased adiposity like abdomen, proximal extremities, buttocks and breast. We report an elderly lady with end-stage kidney disease who presented with severe mastalgia with breast nodules and overlying skin changes. Calciphylaxis was diagnosed based on clinical, mammography and histo-pathological findings. Poor response to standard conservative management prompted us to use glucocorticoids showing dramatic improvement. She had a relapse after 3 months necessitating glucocorticoids again. We report the use of glucocorticoids as an option in recalcitrant, recurrent breast calciphylaxis.
Keywords
Calciphylaxis
End-stage renal disease
Glucocorticoids
Introduction
Calciphylaxis, the term introduced by Selye in 1962, has an annual incidence of 4% and mortality of 45%–80% among hemodialysis patients.1,2 Etiology remains unclear, and glucocorticoids have been implicated as a risk factor.3 We report a case of relapsing calciphylaxis of the breast treated with glucocorticoids with satisfactory response each time, along with other supportive care.
Case Report
A 67-year-old obese lady with diabetic nephropathy for 10 years (baseline creatinine of 4–4.5 mg/dl) had been on warfarin (3 mg/day) since 5 months for chronic atrial fibrillation. She was a nonsmoker. She presented with severe pain in both the breasts with erythematous, violaceous, excoriated skin lesions involving the nipple-areola region, and tender lumps bilaterally. There was no history of inciting trauma to the breasts or similar lesions elsewhere in the body. There was no personal or family history of breast disease or cancer. She also had uremic symptoms. Ultrasonography of breasts showed features suggestive of mastitis, along with multiple linear calcifications in bilateral breasts suggestive of vascular calcifications. Mammography demonstrated extensive linear vascular calcifications [Figure 1] and there was no evidence of tuberculosis, fungal infection, or malignancy. Skin biopsy revealed tissue and vascular calcification [Figure 2]. Her biochemical profile showed corrected serum calcium 11.4 mg/dl, phosphorous 5.1 mg/dl, 25(OH)-vitamin D 29 ng/ml, and Intact parathyroid hormone (iPTH) 86 pg/ml. She was on oral calcium, vitamin D, and active vitamin D supplements. Based on the above findings, diagnosis of breast calciphylaxis was made. Warfarin, calcium, and vitamin D were stopped. She was initiated on hemodialysis. Sodium thiosulfate could not be used due to nonavailability. Intravenous pamidronate was administered three weekly (two doses). She received antibiotics for 3 weeks. After 3 weeks, due to persistent pain and poor wound healing, she was given prednisolone (40 mg/day), which showed dramatic response and was tapered over a month.

- Diagnostic mammogram demonstrating extensive linear branching vascular calcifications with additional distinct tissue calcifications throughout the left breast.
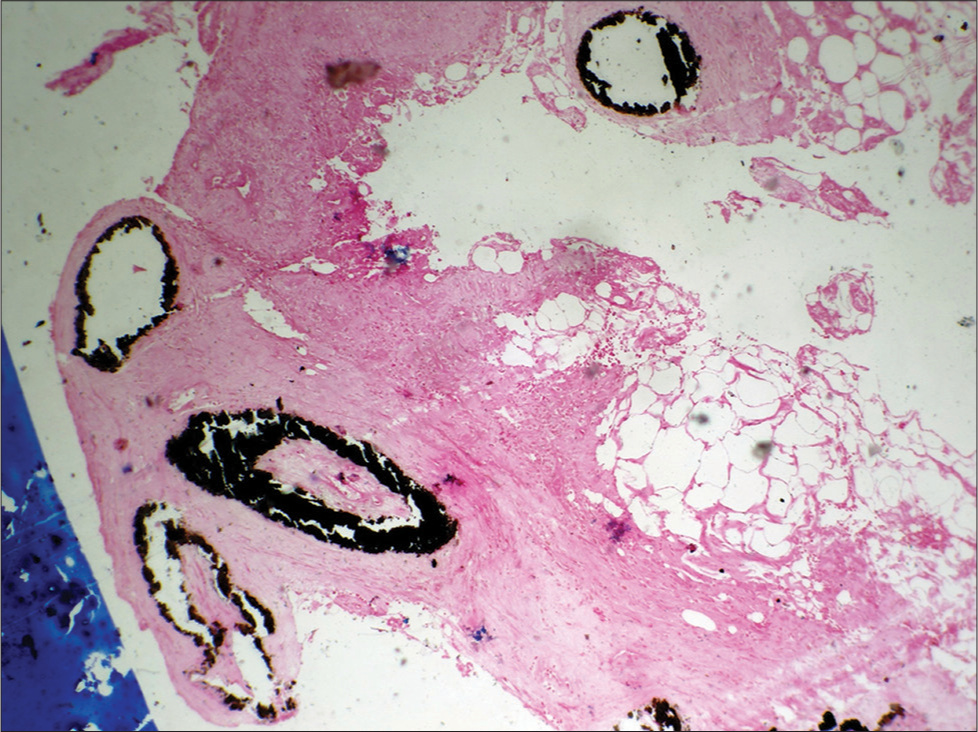
- von Kossa stain showing deposits of calcium within dermal vessel wall.
Three months later, she presented again with right breast abscess and multiple tender breast lumps bilaterally. Despite optimal Chronic Kidney Disease-Mineral Bone Disorder (CKD-MBD) management and wound care, she showed no response. She improved dramatically to prednisolone again (20 mg/day tapered over 2 weeks).
Discussion
Calciphylaxis is a small vessel vasculopathy characterized by intimal proliferation, medial calcification, and endovascular fibrosis,2 which is seen in CKD patients.1,2,4 Intractable pain and skin lesions are attributed to microvascular fibrin thrombi4 and respond poorly to analgesics.2 In addition to several traditional and uremia-related risk factors, medications like warfarin, calcium, vitamin D, and steroids have been implicated as risk factors.1-3
Our patient had female gender, obesity, dyslipidemia, diabetes mellitus, uremia, medications like warfarin, calcium, and vitamin D as risk factors. Warfarin reduces vitamin K-dependent γ-carboxylation of matrix γ-carboxyglutamic acid protein, a major calcification inhibitor.2 High clinical suspicion, diagnostic mammography, and biopsy of the lesion showing characteristic histopathologic lesions expedited the diagnosis of calciphylaxis.
There is no definitive treatment for calciphylaxis, and management is largely supportive. Offending drugs like Ca-based binder, vitamin D, and warfarin should be stopped, as was done in our case. Aggressive wound management, intensified dialysis with low dialysate calcium, long-term sodium thiosulfate, and hyperbaric O2 therapy should be empirically employed.4 Sodium thiosulfate, which possibly reduces the calcification burden by chelating calcium salts and forming a more soluble product (calcium thiosulfate), reduces reactive oxygen species, and causes vasodilation,4 could not be used for our patient due to nonavailability.
Glucocorticoids are implicated as a risk factor for calciphylaxis.1 A case of uremic calciphylaxis treated successfully with oral prednisone has been described.5 Glucocorticoids tend to reduce serum calcium level by inhibiting osteoclast activity, decreasing intestinal calcium absorption, and increasing renal calcium excretion.6 The dramatic response seen in our case was attributed to the anti-inflammatory and calcium-lowering properties of glucocorticoids.
Conclusion
It is important to consider calciphylaxis in a CKD patient with associated risk factors presenting with classical skin lesions. Tender breast lumps in a setting of CKD should raise the possibility of calciphylaxis. Timely diagnosis and treatment, prevention and management of sepsis is vital in obviating mortality. Vitamin K antagonists should be administered with caution in patients with CKD. We further postulate that glucocorticoids could have a possible beneficial role in treating calciphylaxis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
References
- Calciphylaxis: A report of six cases and review of literature. Ren Fail. 2012;35:163-9.
- [CrossRef] [PubMed] [Google Scholar]
- Emerging biomarkers for evaluating cardiovascular risk in the chronic kidney disease patient: How do new pieces fit into the uremic puzzle? Clin J Am Soc Nephrol. 2008;3:505-21.
- [CrossRef] [PubMed] [Google Scholar]
- Calciphylaxis and kidney disease: A review. Am J Kidney Dis. 2023;81:232-9.
- [CrossRef] [PubMed] [Google Scholar]
- Calcifying panniculitis with renal failure: A new management approach. Dermatology. 1996;192:156-9.
- [CrossRef] [PubMed] [Google Scholar]







