Translate this page into:
Renal lymphangiectasia: One disease, many names!
Address for correspondence: Dr. B. Sureka, Department of Radiology and Interventional Radiology, Institute of Liver and Biliary Sciences, New Delhi - 110 070, India. E-mail: binitsurekapgi@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
A 40-year-old female operated for uterine fibroid and endometriosis 2 years back presented with pain in bilateral flank and lower abdomen for the past 1 year. The clinical examination was normal except for mild tenderness in lower abdomen. Laboratory investigations revealed low hemoglobin (7.7 g/dl); however, total leukocyte counts were normal. Patient had a previous ultrasound done outside, which suggested bilateral hydronephrosis due to mass effect of bulky uterus. Kidney function tests and urine examination were also normal. The patient subsequently underwent imaging to assess the cause of abdominal pain and distension.
Ultrasound examination of the abdomen demonstrated bilateral, almost symmetrical, multicystic fluid collections in the peripelvic spaces insinuating into the renal sinuses and splaying the bilateral pelvicalyceal system [Figure 1]. Both kidneys were normal in size, shape and echo-texture with preserved corticomedullary differentiation and no evidence of hydronephrosis on either side. No cysts or masses were identified in other organs.
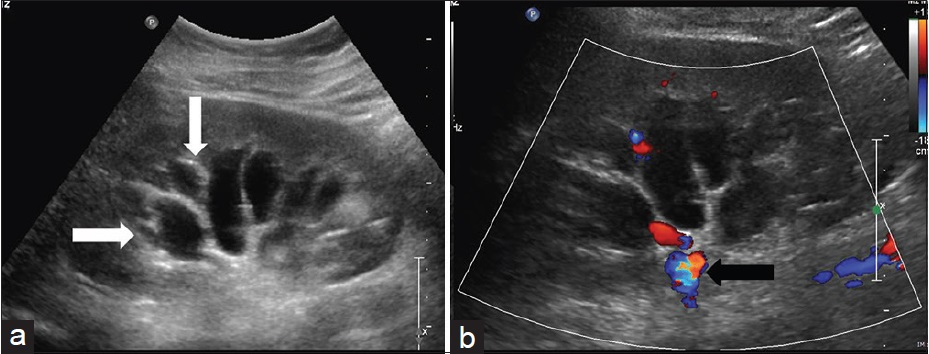
- (a) Ultrasound images showing anechoic fluid-filled multi-septated cystic spaces (arrows) insinuating the renal sinuses. (b) Color Doppler shows absence of color uptake (arrow) by these cystic structures
A contrast-enhanced computed tomography (CT) of the abdomen revealed bilateral hypodense nonenhancing fluid attenuation collections with densities varying between 5 and 10 Hounsfield units in the peripelvic space [Figure 2a]. Both renal cortices showed normal enhancement with normal corticomedullary differentiation. No soft tissue or fat density masses were present within the fluid collections. Delayed scans obtained after 15 min showed normal excretion, but splayed pelvicalyceal systems due to intervening fluid collections within the sinuses [Figure 2b]. There was no hydronephrosis on either side. Renal arteries and veins were showing normal contrast enhancement with splaying of the pelvic vasculature. Subsequent magnetic resonance imaging confirmed the CT findings of multicystic collections in bilateral peripelvic spaces consistent with renal pelvic lymphangiectasia [Figure 2c].

- (a) Axial contrast-enhanced computed tomography (CT) scan showing nonenhancing multi-cystic structures in bilateral peripelvic region. (b) Delayed axial image showing splaying of contrast-filled pelvicalyceal system separate from these cystic structures. (c) Axial T2-weighted fat sat images showing T2 hyperintense multicystic structures separated by fine septae in the peripelvic region
Renal lymphangiectasia is a benign, rare disorder of renal lymphatic system seen both in children and in adults.[1] The nomenclature of this disorder is varied and has evolved in recent years, including “renal lymphangiomatosis,” “renal lymphangioma,” peripelvic lymphangiectasia, and renal peripelvic multicystic lymphangiectasia.[2] “Renal lymphangiectasia” is the preferred name, as the disorder is characterized by ectatic perirenal, peripelvic, and intrarenal lymphatic channels.[3] Lymphangiectasia may be unilateral or bilateral. The pathophysiology is speculative with various reports suggesting it to be a result of congenital or acquired insult as a result of impaired renal sinus drainage.[4] Pathologically, only cortex is involved and it is characterized by dilatation of endothelial-lined spaces without glomerular or tubular abnormalities. Patient may present with flank pain, hematuria, and abdominal pain. The differential diagnosis of renal lymphangiectasia includes hydronephrosis, polycystic kidney disease, urinoma, and lymphoma. Excretory urography is confirmatory for hydronephrosis, which shows excretion of contrast into the pelvicalyceal system. Adult polycystic kidney disease demonstrates varying size scattered intra-parenchymal cysts, and associated liver and pancreatic cysts. Lymphoma shows soft tissue characteristics on imaging as opposed to fluid attenuation seen with lymphangiectasia. The diagnosis of renal lymphangiectasia is usually made confidently on imaging, as in our case. Aspiration is usually not required but in atypical cases, when done, shows chylous fluid. Treatment is usually not necessary as these lesions may regress spontaneously. Complicated cases are treated with nephrectomy, percutaneous drainage, and marsupialisation.[5] Associations with renal vein thrombosis, hypertension, and pregnancy-related veno-lymphatic obstruction has been described. Patient's current symptoms were attributed to endometriosis, and renal lymphangiectasia was an incidental finding and is on regular follow-up.
Acknowledgement
Dr. Nitesh Agrawal, Senior Resident, Department of Radiology.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Retroperitoneal lymphangiectasia associated with bilateral renal vein thrombosis. Nephrol Dial Transplant. 1997;12:1701-3.
- [Google Scholar]






