Translate this page into:
Retrospective analysis of 271 arteriovenous fistulas as vascular access for hemodialysis
Address for correspondence: Dr. Parag Sahasrabudhe, Plot 82, Lane 2, Natraj Society, Karvenagar, Pune - 411 052, Maharashtra, India. E-mail: drparags@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
This report describes our experience of arteriovenous fistula (AVF) creation as vascular access for hemodialysis (HD). Study has been carried out in Deenanath Mangeshkar Hospital, Pune from January 2004 to December 2009. A total of 271 AVFs were created in 249 patients. Maximum follow up was 7 years and minimum was 1 year. In this study of 271 cases of AVFs, there were 196 (72.3%) successful cases and 75 (27.7%) failures. Basilic vein was used in 77 (28.4%) cases, cephalic vein in 186 (68.6%), and antecubital vein in 8 (3%) cases. End (vein) to side (artery) anastomosis was done in 170 (63%) cases. Side to side anastomosis was done in 100 (37%) cases. On table bruit was present in 244 (90%) and thrill in 232 (85.6%) cases. During dialysis, flow rate >250 ml/min was obtained in 136 (50.4%) cases. In complications, 16 (5.9%) patients developed distal edema, 32 (11.8%) developed steal phenomenon. Presence of on table thrill and bruit are indicators of successful AVF. If vein diameter is <2 mm, chances of AVF failure are high. During proximal side to side fistula between antecubital/basilic vein and brachial artery, breaking of first valve toward wrist helps to develop distal veins in forearm by retrograde flow. This technique avoids requirement of superficialization of basilic vein in arm.
Keywords
Arteriovenous fistula
chronic kidney disease
hemodialysis
vascular access
Introduction
End stage renal disease (ESRD) patients depend on lifelong renal replacement therapy (dialysis or renal transplant) to sustain their lives. After Scribner shunt in 1960, Cimino and Brescia described the creation of subcutaneous arteriovenous fistula (AVF) constructed between the radial artery and an adjacent vein in 1966. Cimino fistulas are currently accepted as the best mode of vascular access for hemodialysis (HD).[1]
This is single center, single surgeon retrospective study comparing preoperative vein and artery diameters, presence of on table bruit and thrill, role of postoperative anticoagulants and suture used to postoperative outcome and patency.
Materials and Methods
This retrospective observation study was carried out in our institute in patients who underwent surgical AVF creation between January 2004 and December 2009.
During this period, AVF was created in 421 patients but we could follow up only 249 patients during January to July 2011. Follow up was obtained in collaboration with dialysis unit staff by telephonic calls and personal visits to the patients. The data extracted from hospital records included patient demographics, co-morbidities, details of previous access, location and type of AVF, operative details, patency, morbidity, and mortality. The data collection was difficult and took time of 6 months as some patients were taking dialysis at some other centers. Some were lost to follow up and others could not be reached.
A total of 271 AVFs were placed in 249 patients. Maximum follow up was 7 years and minimum follow up was 1 year. Twenty-two patients required repeat procedure due to failure of previous fistula.
Patients were advised surgery for AVF when their Modified Diet for Renal Disease estimated Glomerular Filtration Rate (MDRD eGFR)[2] was below 15 ml/min. HD catheter was inserted only in cases who presented late and required HD before maturation of fistula.
History of diabetes mellitus, anticoagulant therapy for coagulation disorder, cardiovascular disease, heart valve disease or prosthesis, previous dialysis access, previous central venous or peripheral catheter were noted. Physical exam of the arterial system (peripheral pulses, Allen test, bilateral upper extremity blood pressure) was performed along with physical exam of the venous system (edema, arm size comparability, collateral veins, tourniquet venous palpation with vein mapping, examination for previous central or peripheral venous catheters, evidence of arm, neck, or chest surgery/trauma). Dominance of hand was examined and preference was given to nondominant hand for vascular access creation.
Preoperative color Doppler of upper limb veins and arteries was done in selected patients to look for size and patency. It was done in patients with insufficient clinical examination like in cases with obesity, absent or feeble pulses, multiple previous access surgeries, indwelling dialysis catheter on same side, and history suggestive of thrombophlebitis.
Subclavian vein catheterization was avoided for temporary access in all patients due to the risk of central venous stenosis, which compromises entire ipsilateral arm for vascular access. Arm veins suitable for vascular access placement were preserved, and patients and dialysis staff were instructed not to prick selected arm.
Operative technique
All patients were admitted on the day of surgery. All cases were done under local anesthesia using 10 cc 2% Xylocaine by single surgeon under loupe magnification using microvascular instruments. ‘S’ shape 2.5–3 cm. long incision was used. Vein and artery were mobilized adequately. Arteriotomy size in all cases was 7–8 mm. Anastomosis was done by taking continuous running suture using 7-0 polypropylene or 8-0 ethilon depending upon vessel wall thickness [Figure 1]. For distal and mid forearm fistula, end of cephalic vein to side of radial artery anastomosis was performed [Figure 2]. For proximal fistula, we performed side to side anastomosis between anticubital or basilic vein and brachial artery [Figure 3]. Before anastomosis was completed, we dilated distal vein using venous dilator to break the first valve toward the wrist end to allow retrograde flow into forearm veins. This technique avoided requirement of superficialization of basilic vein in arm in cases where forearm veins fail to develop in spite of good bruit and thrill. In cases where antecubital vein was used, both cephalic and basilic veins got arterialized and could be cannulated. Skin closure was done with 3-0 ethilon in single layer. Noncompressive dressing was given. Bruit was heard and thrill was felt on operation table end of dressing. In cases where bruit was absent but there was good venous filling, we started anticoagulation with low molecular weight heparin subcutaneously for 3–5 days, (doses according to creatinine clearance), and tablet aspirin 75 mg. once a day for 3-5 days. Patient was discharged on same day or next day. Relevant instructions about care of operated side arm were given to the patients and their relatives. They were told to avoid AVF arm vein blood collection, avoid blood pressure cuffs, not to use tight clothing or jewellery, and avoid prolong pressure on operated arm. Written instructions about how to feel for thrill were given and patients were asked to report any coldness, numbness, ulcers, discoloration at fingertips. Hand ball exercises were taught to patients before discharge.
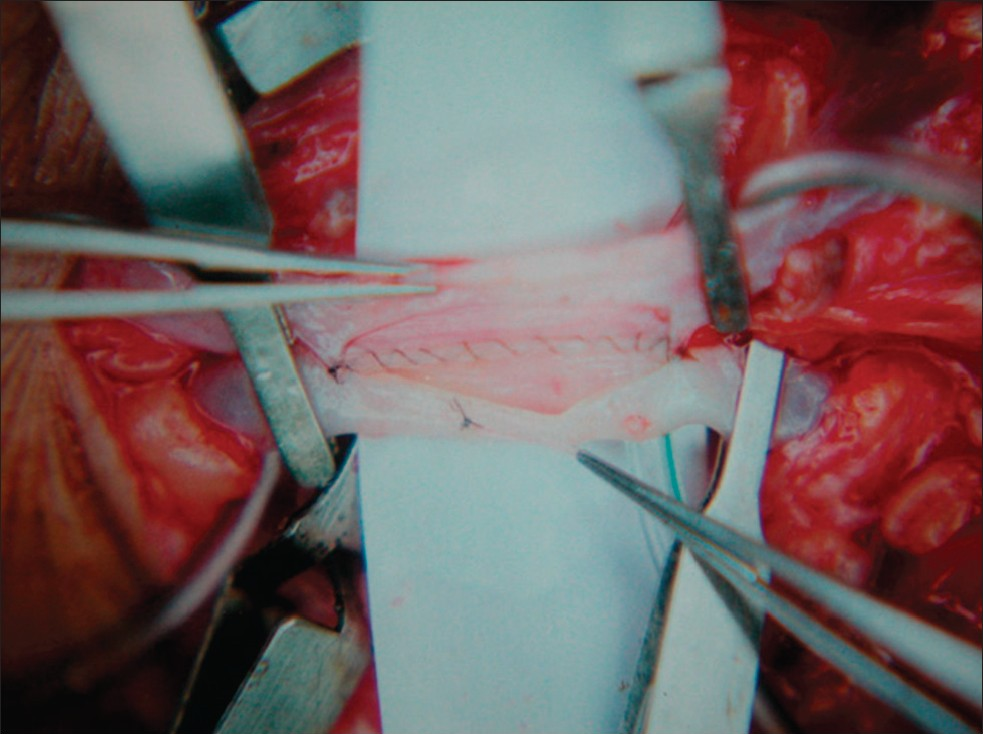
- Intraoperative picture postwall complete with 8 0 ethilon

- End to side radiocephalic fistula

- Proximal AVF side to side anast brachiobasilic
Fistula maturation and its cannulation for use of dialysis was decided by nephrologist based on visible enlarged vein and well felt thrill which required 4–6 weeks after construction. We considered 250 ml/min as a flow rate obtained on HD machine during HD, which was sustained for minimum of 3 hours as acceptable flow during HD.
We followed the NKF-K/DOQI Vascular Access Clinical Practice Guidelines 2000.[3] However, few guidelines could not be followed, for example, early reference, timing of access placement (1–4 months before anticipated HD), Doppler ultrasound in all cases and early intervention in failing fistulas. Above limitations were due to poor patient compliance and affordability in Indian scenario.
The data was analyzed using SPSS (statistical package for social sciences) version 20. Student’s t-test was used to find the differences. Chi square test was used to look at the association. Regression was used to find predictors or risk factors.
Results
In the present series of 271 fistulas (baseline characteristics of patients are given in Table 1), 86 were proximal fistulas, 180 were distal fistulas, and 5 were mid forearm fistulas. Eighty-one fistulas were done on right side and 190 were done on left side. Basilic vein was used in 77 cases, cephalic vein was used in 186 cases, and antecubital vein was used in 8 cases. Vein anastomosis was done with radial artery in 187 cases and brachial artery in 84 cases. End (vein) to side (artery) anastomosis was done in 171 cases. Side (vein) to side (artery) anastomosis was done in 100 cases. In 17 cases vein diameter was <2 mm and in 18 cases arterial diameter was <2 mm. Bruit was heard in 244 cases and thrill was felt in 232 cases on operation table.

During HD, flow rate >250 ml/min was obtained in 136 cases. It was sufficient to perform successful HD in these patients as it sustained for period of at least 3 hours during 4 hours of HD. The flow rate >250 ml/min was not flow across fistula, as measured by radiological or any other means, but actual flow rate obtained on blood pump during HD.
In complications, 16 patients developed distal edema [Figure 4], 32 developed steal phenomenon. We did not find aneurysm, operative site infection, and major bleeding requiring intervention during follow up period. There were 69 deaths during follow up period and none were attributable to a direct complication of vascular access operations.

- Venous hypertension.
Fistula is six times more likely to be successful when thrill was felt on operation table. This result is significant at P = 0.004 when adjusted with bruit, vein <2 mm, artery <2 mm, suture, age, and site of fistula. Also more cases were successful when bruit (P = 0.003) was present on operation table.
The result also showed that vein <2 mm is significantly (P = 0.008) less likely to be successful [Table 2]. Artery and vein ≥2 mm showed success in about three-fourth of the patients as compared with artery and vein <2 mm (P = 0.028, P < 0.0001, respectively). Univariate logistic regression showed that cases with bruit heard on operation table were 3.2 times (P = 0.0005), thrill felt on operation table were 4.79 times (P < 0.0001), vein ≥2 mm were 7.26 times (P < 0.0001) and artery ≥2 mm were 2.83 times (P = 0.035) likely to be associated with success of AVF. In multivariate logistic regression, when adjusted with all above mentioned variables, vein ≥2 mm was 5.26 times (P < 0.0001) more likely to be associated with success of AVF.

Though the results were not statistically significant, it was observed that proximal fistulas had high success rate than distal (76% vs 70%), side to side than end to side (76% vs 70%), brachial artery than radical artery (75% vs 71%), and nondiabetic patients than diabetic (30% vs 25%). Postoperative heparin was given in 238 cases, of which 173 were successful. Out of 33 nonheparinized cases 23 were successful (P value −0.719).
Causes of 75 failures were injury (1 patient), hypotension (4 patients), thrombosis (3 patients), and not known (reported) for 67 patients. There were significantly more deaths in AVF failure cases (P - 0.031).
In proximal fistula, bruit was heard in 97.7% cases and thrill was felt in 94.2% cases on operation table. In distal fistulas, bruit was heard in 86% and thrill was felt in 81.1% on operation table. Hence success rate was more (75.6%) in proximal than in distal (70.6%) fistulas.
Complication like edema and steal phenomenon were more (9.3% and 16.3%, respectively) in proximal than in distal (4.4% and 10%, respectively) fistulas.
Discussion
Successful HD depends on creation and maintenance of adequate vascular access. Due to general population aging, median age at onset of ESRD has been progressively increased over last few decades. More than 20% of people have diabetes as a cause of ESRD and average age is 58.8 years.[4] In our study of 271 cases, average age of presentation was 55 years and 48.7% patients had diabetes as a cause of ESRD.
Patients who receive dialysis across a functional AVF have lower complication rates and longer duration of event-free patency than patients with catheter access[5–8] and arteriovenous grafts (AVGs).[69] Thus construction of a native AVF on arm or forearm is considered a good practice over prosthetic grafts and central venous catheters. There were no AVGs created in the present series. There is vast data proving that native AVFs are superior to grafts as a form of vascular access for dialysis.[6] It has been demonstrated that early referral to nephrologist and good collaboration with microvascular surgeon reduce the need for temporary dialysis access for first dialysis and increase the rate of successful AVF placement.[10] However, central venous catheters are primary method of choice for temporary access in which there is urgent need for HD and no other vascular access is available or has failed.[8] However, these devices suffer from several complicating factors as infection, thrombosis, venous stenosis, and damage to proximal vessels.[11] We performed AVF in all our CKD patients as first choice of vascular access.
The most common operative procedure was the creation of the distal radio cephalic fistula, initially described by Brescia, et al. in 1966.[1] This operation is still considered to be the gold standard for vascular access for HD[12] and it accounted for 180 (66.4%) of our operative procedures. High radio cephalic (mid forearm) and brachial-basilic AVFs were reserved for patients with previously failed Brescia - Cimino AVFs or where patent adequate size vessels at wrist level were not available for anastomosis. The outcomes of the classic Brescia - Cimino operation were accompanied by acceptable rates of morbidity.[1314]
Most large-volume centers report 15-30% primary failure rates for distal radio cephalic AVF.[1314] The reported incidence of primary failure in the medical literature varies from 9%[15] to 40%[16] and our results were comparable with 29.4% primary failures. The NKF/DOQI (National Kidney Foundation Disease Outcome Quality Initiative) Work Group did not recommend the use of primary failure as an index of quality because it would discourage attempts at AVF construction in patients with complex vascular anatomy.[2]
American Institute of Ultrasound in Medicine (AIUM) Practice Guideline 2011[1718] states that arterial diameter <2 mm and venous diameter <2.5 mm were associated with high failure rate. This study also proves that arterial and venous diameters <2 mm are associated with significantly high failure rates (P −0.028 and 0.0001, respectively).
In India, because of illiteracy, poor follow up, and poor socioeconomic status, fistula salvage by early detection of failing fistula and intervention by exploration, embolectomy, or radiological intervention like percutaneous transcutaneous angioplasty for venous outflow stenosis[3] is not cost effective. Hence we prefer to perform new fistula in such situations. In our series no patients required any such salvage procedures.
AVF creation in all (100%) patients with ESRD in our institution far exceeds the target goals of 50% set forward by the NKF/DOQI[3] and the CMS (Centres for Medicare and Medicaid Services) Fistula First Breakthrough Initiative.[19] This was being achieved with acceptable rates of morbidity (27%), no operative mortality and good primary patency (72%). However, early detection of complications by patient education can help to improve long-term patency rates.
In conclusion, we found that
-
Vein diameter <2 mm. showed very high failure rate (P value less than 0.05). Hence, we recommend use of alternative method of access placement in such patients.
-
Thrill felt on operation table has direct relation with success of fistula operation (P −0.004).
-
Postoperative anticoagulation has no major beneficial role in eventual patency rates (P −0.719).
-
During creation of proximal fistula by side to side anastomosis between anticubital/basilic vein and brachial artery, dilatation of distal vein to break the first valve helps to develop distal veins in forearm by retrograde flow avoiding need for superficialization of basilic vein in arm. In none of our patients with proximal fistula superficialization of basilic vein in arm was needed.
Acknowledgment
The author would like to thank Consultants of Department of Medicine, Consultants and staff of Department of Nephrology, Dr. Amit Jadhav, Dr. Sheetal Londhe (Residents, Department of Plastic Surgery), Dr. Joshi Veena, Department of Research at Deenanath Mangeshkar Hospital, Pune and Dr. Shaunak Sule. (Consultants, Plastic Surgeon, Pune).
Source of Support: Nil
Conflict of Interest: None declared.
References
- Chronic hemodialysis using venipuncture and a surgically created arteriovenous fistula. N Engl J Med. 1966;275:1089-92.
- [Google Scholar]
- Chronic Kidney Disease Epidemiology Collaboration. Expressing the Modification of Diet in Renal Disease Study equation for estimating glomerular filtration rate with standardized serum creatinine values. Division of Nephrology, Tufts-New England Medical Center, Boston, MA 02111, USA. Clin Chem. 2007;53:766-72.
- [Google Scholar]
- III. NKF-K/DOQI Clinical Practice Guidelines for Vascular Access: Update 2000. Am J Kidney Dis. 2001;37:S137-81.
- [Google Scholar]
- Primary vascular access in diabetic patients: An audit. Nephrol Dial Transplant. 2000;15:1317-25.
- [Google Scholar]
- Current topic on vascular access for hemodialysis. Minerva Urol Nefrol. 2004;56:223-35.
- [Google Scholar]
- Hemodialysis vascular access preferences and outcomes in the Dialysis Outcomes and Practice Patterns Study (DOPPS) Kidney Int. 2002;61:2266-71.
- [Google Scholar]
- Improving quality of vascular access care for hemodialysis patients. Jt Comm J Qual Saf. 2003;29:191-8.
- [Google Scholar]
- Vascular access in hemodialysis: Issues, management, and emerging concepts. Cardiol Clin. 2005;23:249-73.
- [Google Scholar]
- Temporary vascular access for first dialysisis common, undesirable and usually avoidable. Clin Nephrol. 1999;51:228-32.
- [Google Scholar]
- Approach to patients with end-stage renal disease who need an arteriovenous fistula. Nephrol Dial Transplant. 2003;18(Suppl 5):v50-2.
- [Google Scholar]
- Complications of arteriovenous fistulas for hemodialysis. Arch Surg. 1975;110:708-12.
- [Google Scholar]
- Hemodialysis angioaccess choice and survival in a tertiary care Saudi Arabian center from 1993 to 2004. Nephro-Urology Monthly. 2011;3:69-73.
- [Google Scholar]
- Initial five years of arterio-venous fistula creation for hemodialysis vascular access in Maiduguri, Nigeria. Internet J Cardiovasc Res. 2007;4:1-6.
- [Google Scholar]
- Hemodialysis arteriovenous fistula patency revisited: Results of a prospective, multicenter initiative. Clin J Am Soc Nephrol. 2008;3:714-9.
- [Google Scholar]
- A strategy for increasing use of autogenous hemodialysis access procedures: Impact of preoperative noninvasive evaluation. Department of Surgery, University of Medicine and Dentistry of New Jersey, New Jersey Medical School, Newark 07103-2714, USA. J Vasc Surg. 1998;27:302-7. discussion 307-8
- [Google Scholar]
- ACR-AIUM-SRU practice guideline for the performance of peripheral arterial ultrasound using color and spectral Doppler. Reston (VA): American College of Radiology (ACR); 2010. p. :5.
- Fistula first initiative: Advantages and pitfalls. Department of Medicine, Division of Nephrology, Toronto General Hospital, Toronto, Ontario, Canada. Clin J Am Soc Nephrol. 2007;2:1043-53.
- [Google Scholar]







