Translate this page into:
Rhabdomyolysis and Pigment Nephropathy – An Uncommon Manifestation of Eucalyptus Oil Consumption
Corresponding author: Dr. Sabarinath Shanmugam, Department of Nephrology and Renal Transplantation, KG Hospital and Postgraduate Medical Institute, Coimbatore, Tamil Nadu, India.
-
Received: ,
Accepted: ,
How to cite this article: Shanmugam S, Sethuraman R, Chakravarthy T, Krishnan G, Kavitha B, Shakila J, et al. Rhabdomyolysis and Pigment Nephropathy – An Uncommon Manifestation of Eucalyptus Oil Consumption. Indian J Nephrol. 2024;34:516-7. doi: 10.25259/ijn_390_23
Abstract
Eucalyptus oil consumption is well known to cause adverse effects on central nervous system like seizures, ataxia and unconsciousness. No antidote is available and treatment is largely supportive. We report a case of rhabdomyolysis with pigment cast nephropathy and acute kidney injury in a young female following eucalyptus oil consumption and its successful management.
Keywords
Cast nephropathy
Eucalyptus Oil
Rhabdomyolysis
AKI
Introduction
Intentional or unintentional consumption of Eucalyptus oil is uncommon in adults. The consumption of even a minimal amount of this oil has serious adverse effects on the central nervous system like drowsiness, ataxia, loss of consciousness, and seizures, occurring within 15 minutes.1,2 Severe acute kidney injury due to cast nephropathy secondary to rhabdomyolysis is rarely reported. Convulsions are commonly reported in children, but rare in adults.3 No antidote is available and treatment is largely supportive care.
Case Report
A 21-year-old female was admitted with a history of consuming about 4 to 5 mL Eucalyptus oil. She developed progressive drowsiness and two generalized tonic-clonic seizure episodes. She was taken to a nearby hospital, where she was intubated due to poor glascow coma score (GCS) and shifted to our tertiary care center. On admission, her GCS was 10, pupils were reacting to light, on the ventilator. Her blood pressure was 128/88 mmHg, SpO2 was 98%, afebrile. No further episodes of seizure activity were noted. She was loaded with intravenous antiepileptic (levetiracetam) and the maintenance dose was continued. Her investigations showed severe metabolic acidosis (high anion gap). Serum creatinine was 1.2 mg/dL on day 1. Her urine output on the day of admission was adequate. Her magnetic resonance imaging (MRI) of brain was normal. The echocardiographic report showed normal left ventricular (LV) wall thickness with a systolic function of 65%. On day 2, she passed brown-colored urine with a gradual drop in urine output. The serum creatinine was 3.15 mg/dL. A workup was done, and an ultrasound showed normal-sized kidneys. Serum creatinine phosphokinase (normal values 20-180 U/L) was very high (37928 U/L) on day 2 and peaked up to 167092 U/L on day 4, serum LDH was 2412 U/L (normal values 135-214 U/L), serum calcium was 7.6 mg/dL, and phosphorus was 5.7 mg/dL. She was extubated from ventilator on day 3. She developed progressive oliguria and underwent two sessions of hemodialysis. A kidney biopsy was done after optimization on day 7 given the rapidly worsening renal function. The kidney biopsy report showed 17 glomeruli, without any significant pathologic changes in the glomerulus. Tubules contained atypical red globular casts which stain positively for myoglobin on immunohistochemical study and there was diffuse attenuation of the proximal tubular epithelial cells with cytoplasmic vacuolization and variable loss of the brush borders. There was no interstitial fibrosis or tubular atrophy. The arteries show mild intimal fibrosis. Arterioles are normal [Figure 1]. Immunofluorescence showed granular mesangial staining of the glomeruli for IgA (1+), C3 (1+), kappa (1+), and lambda (1+) light chains. [Figure 1].
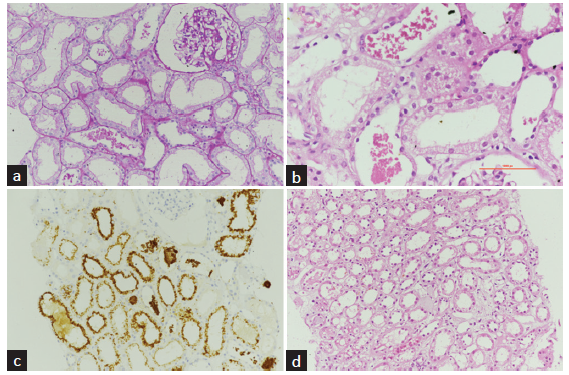
- Light microscopic and immunofluorescence findings of kidney biopsy. (a) 20x, PAS: Renal cortex showing normal glomerulus. Few tubules contain atypical globular casts with associated acute tubular injury. (b) 40x, H and E: Tubules containing atypical red globular casts with attenuation of the proximal tubular epithelial cells, cytoplasmic vacuolization, and variable loss of the brush borders. (c) 20x: The atypical intratubular casts and some of the tubular epithelial cells stain positively for myoglobin immunohistochemistry. (d) 20x, H and E: Mild edema and interstitial inflammation.
With supportive care, her urine output gradually improved. She developed recurrent pulmonary edema with unexplained tachycardia from day 9. Her Troponin I was 614 pg/mL (normal values - less than 15.6 pg/mL). The echocardiogram showed a new onset of severe LV dysfunction with an ejection fraction of 25%. She was managed with intravenous Dobutamine and diuretics. Her renal function gradually improved, and serum creatinine declined to 1.34 mg/dL on day 14. On 3 months of follow-up, her serum creatinine was 0.57 mg/dL and her LV ejection fraction improved to 55%. The lab investigations during her hospital course was tabulated in Table 1.
| Day 1 | Day 3 | Day 4 | Day 7 | Day 10 | Day 12 | Day 14 | Follow-up | |
|---|---|---|---|---|---|---|---|---|
| Hb (g/dL) | 13.7 | 12.6 | ||||||
| TLC (cells/cu.mm) | 14,800 | |||||||
| Platelet count (cells/cu.mm) | 3,62,000 | |||||||
| Urea (mg/dL) | 22 | |||||||
| Serum creatinine (mg/dL) | 1.24 | 3.97 | 5.07 | 5.08 | 3.21 | 2.3 | 1.35 | 0.57 |
| Serum Na (mEq/L) | 138 | 141 | 134 | 131 | 135 | 134 | ||
| Serum K (mEq/L) | 3.7 | 5.3 | 4.4 | 4.8 | 3.4 | 4.2 | ||
| Serum Calcium (mg/dL) | 7.6 | 8.2 | ||||||
| Serum Phosphorus (mg/dL) | 5.7 | 4.3 | ||||||
| Serum LDH (U/L) | 2412 | |||||||
| Serum CPK (U/L) | 37,928 | 16,7092 | 17,380 | 988 | 432 | |||
| SGOT (U/L) | 34 | |||||||
| SGPT (U/L) | 23 | |||||||
| Total Protein (gm/dL) | 7.4 | |||||||
| Serum Albumin (gm/dL) | 4.7 | |||||||
| Alkaline Phosphatase (U/L) | 67 |
Hb=Hemoglobin, TLC=Total leucocyte count, Na=sodium, K=potassium, LDH=Lactate dehydrogenase, CPK=Creatine phosphokinase, SGOT=Serum glutamic-oxaloacetic transaminase, SGPT=Serum glutamic-pyruvic transaminase
Discussion
Eucalyptus oil poisoning has been described in children. Central nervous system symptoms can occur within 30 minutes, although they may be delayed for up to 4 hours.1 In our case, she had rapid-onset symptoms with drowsiness and convulsions. The reason behind the adverse effect of eucalyptus oil may be hydrocyanic acid which is highly toxic and may cause drowsiness, seizures, and coma. The two unique features in our case were rhabdomyolysis (leading to pigment cast associated acute kidney injury) and myocarditis, probably toxin-induced. The clinical clue in our case was the passage of muddy urine. A kidney biopsy confirmed the diagnosis. The rhabdomyolysis can be attributed to seizures (or) eucalyptus oil itself. The major mechanism of renal tubular damage in rhabdomyolysis is mitochondrial-free radical production which induces lipid peroxidation.4,5 The features of myocarditis, which appeared after a week in our case, could be attributed to toxins present in eucalyptus oil. Over 1 month there was an improvement in LV function.
Conclusion
Eucalyptus oil consumption can have serious adverse events like seizures, rhabdomyolysis, pigment-cast–associated acute kidney injury, and myocarditis. A high index of clinical suspicion is needed for diagnosis and treatment.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
References
- Unintentional exposure of young children to camphor and eucalyptus oils. Paediatr Child Health. 2001;6:80-3.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Eucalyptus oil poisoning. Toxicol Int. 2015;22:170-1.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Bench-to-bedside review: Rhabdomyolysis: An overview for clinicians. Crit Care. 2005;9:158-69.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Mitochondrial free radical production induces lipid peroxidation during myohemoglobinuria. Kidney Int. 1996;49:741-51.
- [CrossRef] [PubMed] [Google Scholar]








