Translate this page into:
Rhabdomyolysis induced acute renal failure secondary to statins
Address for correspondence: Dr. Rapur Ram, Department of Nephrology, Nizam’s Institute of Medical Sciences, Punjagutta, Hyderabad, India. E-mail: ram_5_1999@yahoo.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Rhabdomyolysis is a syndrome characterized by muscle necrosis and the release of intracellular muscle contents into the systemic circulation. We report a patient with chronic kidney disease who had deterioration of renal function due to combination of risk factors like hypothyroidism and interaction of amlodipine and clopidogrel with statins.
Keywords
Acute renal failure
amlodipine
clopidogrel
hypothyroidism
rhabdomyolysis
statins
Introduction
Rhabdomyolysis is characterized by muscle necrosis and the release of intracellular muscle contents into the systemic circulation. The spectrum of the syndrome ranges from asymptomatic serum muscle enzymes elevation to life-threatening extreme enzyme elevations, electrolyte imbalances, and acute renal failure. We report an elderly lady with a combination of risk factors who developed rhabdomyolytic acute renal failure.
Case Report
A 65-year-old lady was suffering from type 2 diabetes for the past 30 years, hypertension for the past 20 years, and coronary heart disease for the past 10 years. She was diagnosed chronic kidney disease about 6 months ago. Her serum creatinine was stable at 2.0 mg/dL. The medications included clopidogrel 75 mg/day, amlodipine 10 mg/day, frusemide 40 mg bds, and insulin. A week before presenting to us, a cardiologist had added atorvastatin 10 mg/day to her prescription. She presented to us with complaints of severe generalized myalgia, difficulty in assuming upright posture from sitting position, and difficulty in walking of 1 week duration. She also complained of swelling of feet, face, nausea, loss of appetite and noticed decreased urine output, and reddish discoloration to urine for the last 3 days. There was no fever, history of trauma, viral exanthem, severe exercise, seizure, uncontrolled blood glucose, and use of herbal medication preceding the illness. On examination, she was well-built and well-nourished, and had pedal edema and facial puffiness. There was no icterus, no clubbing, and no lymphadenopathy. She was afebrile with pulse rate of 60 beats per min and blood pressure of 160/90 mm Hg. Neurological examination showed 2/5 power in all four limbs, absent deep tendon reflexes, and muscle tenderness with no sensory involvement. Examination of cardiovascular, respiratory, and gastrointestinal systems was unremarkable. The investigations are presented in Table 1.
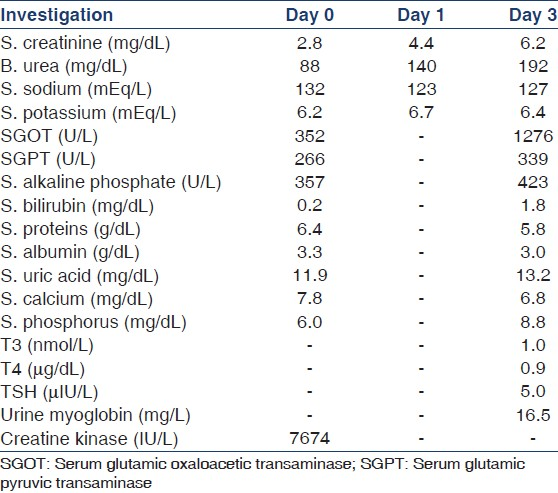
Urinalysis showed glucose 2+, ketone bodies negative, blood positive, red blood cells nil, and white blood cells 1-2/hpf. Her hemoglobin was 11.4 g/dL, total leukocyte count 18, 300 per mm3, platelet count 5.0 lakh per mm3, ESR 20 mm after 1 h, electrocardiogram showed tall peaked and widened T waves with proximal limb steeper than distal limb, and the chest radiograph was normal. Ultrasound abdomen showed right kidney 9.3 × 3.7 cm and left kidney 9.2 × 3.2 cm. The urine and blood cultures were sterile, HIV, HBsAg, anti-HCV antibodies, anti-HAV IgM, and anti-HEV IgM were negative.
Patient was initiated on hemodialysis. Myalagia, reddish discoloration to urine, deterioration of renal function, elevated SGOT, creatinine kinase, and increased urine myoglobin led to the diagnosis of rhabdomyolysis. Atorvastatin was stopped. Levothyroxine replacement was initiated at a dose of 50 μg/day, increased after 15 days to 100 μg/day. The following three risk factors for the onset of rhabdomyolysis were identified: Use of statin, undiagnosed hypothyroidism, and co-administration of amlodipine and clopidogrel. Amlodipine and clopidogrel were also withheld. Frusemide was stopped as she had hypokalemia before the onset of illness which was again a risk factor for rhabdomyolysis. After seven sessions of hemodialysis the urine output improved and serum creatinine stabilized at 3.2 mg/dL. Creatine kinase and SGOT levels returned to normal. She regained power in all limbs. Deep tendon reflexes appeared again.
Discussion
In randomized controlled trials, statin myopathy incidence is about 1.5–5.0%.[12] However, it is difficult to directly compare the incidence of statin myopathy in clinical trials with real world clinical practice given the inconsistent definitions. The common risk factors for the development of a statin-induced myopathy include high dosages, increasing age, female sex, renal and hepatic insufficiency, diabetes mellitus and concomitant therapy with fibrates, cyclosporine, macrolide antibiotics, warfarin, and digoxin.[3]
Individual statins differ in their risk of inducing rhabdomyolysis, with some patients developing this syndrome when switching from one statin to another. Other patients developed rhabdomyolysis when exposed to any statin. It is probable that genetic factors play a role in the pathogenesis of this syndrome. The temporal relation between statin therapy and the onset or resolution of myopathy is not fully defined. A retrospective study of 45 patients with statin myopathy at a tertiary center revealed a mean therapy duration of 6.3 months before symptom onset and a mean duration of 2.3 months for symptom resolution after discontinuation of statin therapy.[4] Patients in PRIMO study developed muscle symptoms after a median of 1 month after initiation of statin therapy, ranging up to 12 months after initiation.[5]
The combinations of risk factors present in this patient were not widely reported.[6] Hypothyroidism was reported as a predictor of statin-associated myopathy (OR 1.71; CI, 1.10-2.65) in PRIMO study.[5] Hypothyroidism could itself be a risk factor for renal impairment. The likely mechanisms of renal impairment in hypothyroidism are the reduction in glomerular filtration rate due to the lower cardiac output and renal blood flow,[7] thyroxine may mediate tubular secretion of creatinine,[8] hypothyroidism may increase creatinine release from muscle,[9] and rhabdomyolysis.[10]
Amlodipine, atorvastatin, and clopidogrel are metabolized by hepatic CYP450 3A4. It is possible for two different substrates of the same metabolizing enzyme to compete for catalytic sites on the same enzyme; through competitive inhibition, one substrate may gain access to these sites whereas the other is excluded. This process results in metabolism of the drug that successfully accesses the catalytic sites of the enzyme, whereas the excluded drug is metabolized at a significantly slower rate.[1112] In the present patient there were three drugs which might have competed for the hepatic CYP450 3A4 enzyme. The metabolism of atorvastatin might have been slowed.
The present patient provided a caution that hypothyroidism and interaction with other drugs should be considered when patients were going to be initiated on statins.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Statin safety: An overview and assessment of the data - 2005. Am J Cardiol. 2006;97:6C-26.
- [Google Scholar]
- Outcomes in 45 patients with statin-associated myopathy. Arch Intern Med. 2005;165:2671-6.
- [Google Scholar]
- Mild to moderate muscular symptoms with high-dosage statin therapy in hyperlipidemic patients - The PRIMO study. Cardiovasc Drugs Ther. 2005;19:403-14.
- [Google Scholar]
- A case of rhabdomyolysis induced acute renal failure secondary to statin-fibrate-derivative combination and occult hypothyroidism. Clin Nephrol. 2005;64:391-3.
- [Google Scholar]
- Correlation between severity of thyroid function and renal dysfunction. Clin Endocrinol. 2005;62:423-7.
- [Google Scholar]
- Creatine and creatinine metabolism in thyrotoxicosis and hypothyroidism; a clinical study. Acta Med Scand Suppl. 1957;331:1-70.
- [Google Scholar]
- Do statins inhibit clopidogrel’s antiplatelet activity? 2003. Pharm Times. 10:1-2. Available from: www.http://hanstenandhorn.com/hh-article10-03.pdf
- [Google Scholar]
- Clopidogrel-precipitated rhabdomyolysis in a stable heart transplant patient. Ann Pharmacother. 2007;41:133-7.
- [Google Scholar]







