Translate this page into:
Rhinocerebral Mucormycosis in Patients with Kidney Disease Following Covid 19 Infection
Corresponding author: Manjusha Yadla, Department of Nephrology, Gandhi Medical College, Hyderabad, Telangana, India. E-mail: manjuyadla@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Yadla M, Manu, Ahmed T, Burri S, Yadav S, Shoban, et al. Rhinocerebral Mucormycosis in Patients with Kidney Disease Following Covid 19 Infection. Indian J Nephrol. 2024;34:369-73. doi: 10.25259/ijn_233_21
Abstract
Opportunistic infections saw a rise during the COVID-19 pandemic. We report rhinocerebral mucormycosis following COVID infection in six patients with kidney disease. Though there was a variable outcome with 50% mortality, it is prudent to assess the risk factors for development of life-threatening infection.
Keywords
CKD
COVID-19
Dialysis
Rhinocerebral mucormycosis
Transplant
Introduction
Rhinocerebral mucormycosis infections have been on the rise in the Indian subcontinent since the onset of the second wave of the COVID pandemic. Multiple plausible mechanisms have been elucidated for rampant occurrence of this infection, such as inappropriate usage of steroids, oxygen mask/humidifier, unhygienic maintenance of mask, uncontrolled sugars.1 Coexistence of severe immune dysregulation in patients infected with COVID-19 and the duration of ventilatory support, longer duration of hospitalization, and extended usage of steroids were proposed for an increasing prevalence of colonial fungi becoming opportunistic infection leading to high morbidity and mortality rates.2 At the same time, there are anecdotal reports claiming the occurrence in post-COVID patients without any such predisposing factors.
Kidney-disease patients are immunosuppressed due to underlying immune modulation because of underlying primary disease, immunosuppressive drugs, renal replacement therapies, etc. The premise that black fungus is secondary to overdose of steroids may not be true as the number of immunosuppressive drugs used by patients of nephrology is high compared to the number of steroids being given for COVID management. Despite the routine usage of immunosuppression, the number of patients presenting with mucormycosis is rare in transplant recipients. However, with the COVID pandemic, there has been an alarming rise in black fungus patients across India. Few reports of this fungal infection in kidney patients with COVID infection have been reported.
Results
Our hospital is a State Government-designated COVID hospital since March 2020. During the second wave of cases, we had 220 kidney referrals, of which 160 were dialysis patients, eight patients had acute kidney injury, and 45 patients had acute deterioration of underlying kidney disease. With the onset of black fungal infection, our hospital with a multidisciplinary unit was designated as a nodal center for the same. To date, we had 200 patients admitted with rhinocerebral mucormycosis. All the admitted patients were assessed clinically by appropriate departments. Management strategy included liposomal amphotericin according to weight, oral Posaconazole, and other supportive treatment. As per the hospital protocol, all the patients were subjected to functional endoscopic sinus surgery (FESS) before conventional surgery. Surgical management strategies included debridement, exploration, maxillectomy, enucleation, and delayed enucleation. Depending on the extent of involvement of soft tissue and the bony structures, patients were managed with debridement and exploration. None of our patients underwent surgery due to underlying critical conditions.
We had six patients with kidney disease with mucormycosis following COVID infection. Details of cases mentioned in Table 1.
| Patient No. | Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 |
|---|---|---|---|---|---|---|
| Age | 22 | 33 | 29 | 45 | 58 | 52 |
| Gender | Male | Male | Male | Male | Male | Male |
| COVID/Post COVID | COVID | COVID | Post COVID | COVID-one week in isolation | COVID | Post COVID |
| Latency of presentation of fungus infection | Simultaneous | Simultaneous | 10 days later | 1 week | Simultaneous | 1 week |
| Nature of Kidney disease | VUR-CIN-CKD 5ND | LRRT -mild Graft dysfunction | CKD-5D on HD X5 years | Hypertension | CKD-5ND | Acute on CKD |
| CKD-5D | ||||||
| Immunosuppression drugs | Nil | CNI, MMF, Steroids | Nil | Nil | Nil | Nil |
| Diabetes/Denovo diabetes | No | Denovo | Denovo | Nil | Denovo | Known diabetes |
| Appropriate Steroid dosage | Yes | Yes | Yes | Yes | Yes | Yes |
| Clinical symptoms | Swelling of face with periorbital swelling, decreased vision [Figure 1] | Epistaxis, Fever, cough. During hospital stay, had left facial pain, swelling, headache, altered sensorium | Swelling of left eye, jaw pain, jaw swelling | Swelling of left half of face | Swelling of face with significant periorbital edema and oral ulcers | Swelling of left half face |
| Altered sensorium | Decreased vision. | |||||
| Left proptosis | ||||||
| Mucor symptom onset | At admission | 3 days after admission | At admission | 2 days after admission | 5 days after admission | At admission |
| Radiological evidence | B/L Ethmoidal sinusitis with underlying erosion of bones | Thickening of sinuses lining in bilateral ethmoidal, sphenoidal sinuses. | Thickening of Left frontal, ethmoidal, bilateral sphenoid sinuses lining, left maxillary sinus Pre mandibular soft tissue swelling | B/L Ethmoidal sinusitis with underlying erosion of bones | Thickening of right frontal, maxillary anterior, middle ethmoid, right sphenoid | Pansinusitis with erosion of right orbital wall |
| CTSS of COVID | 12/25 | 11/25 | 16/25 | 7/25 | 3/25 | 9/25 |
| Severity of Infection | Moderate | Moderate | Moderate | Mild | Mild | Moderate |
| Oxygen support | Yes | Increased Need during hospitalization | No | No | No | No |
| Needed after worsening due to IC bleed | ||||||
| Hemoglobin/TLC/Platelets | 6.8/3100/1.5 L | 8.8/4200/1.4 L | 9.2/6000/1.3 L | 9.8/9700/2.2 L | 8.8/5600/2.1 L | 10.1/5300/2.8 L |
| Se.creatinine (mg/dl) | 9.4 | 1.8->3.1->4 | 6.6 | 10.4 | 6.7 | 2.8 |
| Antiviral drugs | Remdesivir | Remdesivir | No | No | Remdesivir | Remdesivir |
| Antibiotics | Yes | Yes | Yes | Yes | Yes | Yes |
| Antifungal drugs | AmBisome | AmBisome | AmBisome | AmBisome | AmBisome | Posaconazole |
| FESS | No | Yes | No | No | No | No |
| Surgery | No | Planned | No | No | No | No |
| Outcome | Death | Death | Recovered | Death | Recovered | Developed intracerebral bleed |
| Possible cause of death | Severe infection, Surgery could not be done | Severe infection, No response to AmBisome | Had seizure, CNS involvement could not be assessed | Died | ||
| Progressing Graft dysfunction |
VUR: vesicouretric reflux, CIN-CKD: chronic interstitial nephritis-chronic kidney disease, LRRT: Live RElated Renal Transplant, CNI: calcineurin inhibitor, MMF: mycophenolate mofetil, CKD-5D: Chronic Kidney Disease-5D, CKD: chronic kidney disease, TLC: total leucocyte count, SE: serum electrolytes, FESS: functional endoscopic sinus surgery, B/L: bilateral, HD: hemodialysis, CNS: central nervous system, CTSS: computed tomography-severity score, X5: for 5 years
Discussion
During the second wave of the COVID pandemic, rhinocerebral mucormycosis was reported widely from India. Kidney-disease patients are immune-dysregulated due to underlying kidney disease or treatment or immunosuppressive drugs. COVID infection in this group is known to be associated with a high risk of morbidity and mortality. In the background of immune system abnormalities, it is expected that the number of mucor cases would be high in kidney-disease patients.
Prevalence of mucor among renal admissions was 3%, and prevalence of kidney patients among mucor admissions was 3%. Four patients had ongoing COVID infection, and two patients had a history of COVID infection. Symptoms of mucormycosis were present at admission in three patients, and three patients developed during hospital stay (between 2 and 5 days) [Figures 1 to 4]. Those patients with active COVID infection were given remdesivir (100 mg before dialysis session) along with other supportive treatment. Variable severity of COVID infection was noted in our group. Severity of COVID infection did not show any relation with the degree of mucormycosis. All patients had extensive involvement of sinuses though few had only mild infection with low CT scan severity score (CTSS). Vision was affected due to oculomotor nerve palsy in two patients.
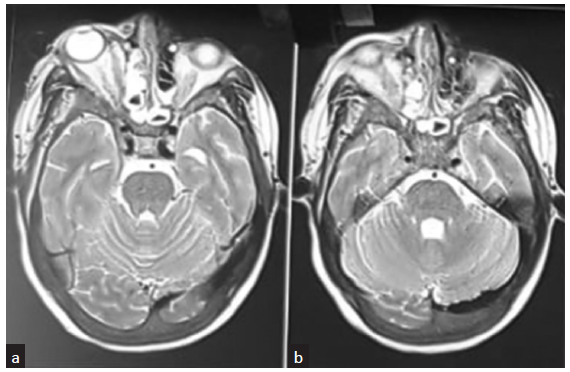
- (a) MRI brain of patient 1 showing the periorbital edema, edema of ocular muscles and changes in paranasal sinuses. (b) MRI brain showing inflammation of paranasal sinuses. MRI: magnetic resonance imaging.
Based on hospital protocol, all patients were given liposomal preparation of amphotericin for 2 weeks (3 mg/kg), followed by oral posaconazole for 6 weeks. One patient received only posaconazole for the complete course. Three patients died with severe infection, no response to antifungal drugs; one patient died after the development of intracerebral bleed. Though surgical exploration and debridement were planned, it could not be done in view of the critical condition of the patients. FESS was done in one patient [Figure 3b–c] which showed black necrotic tissue in bilateral sinuses, confirmed fungal mycelia on KOH mount and culture-grown aspergillus. With the given treatment, two patients recovered completely and were continued with posaconazole treatment. One patient had intracerebral bleed which was thought to be due to progressing mucormycosis, though the association could not be proved.
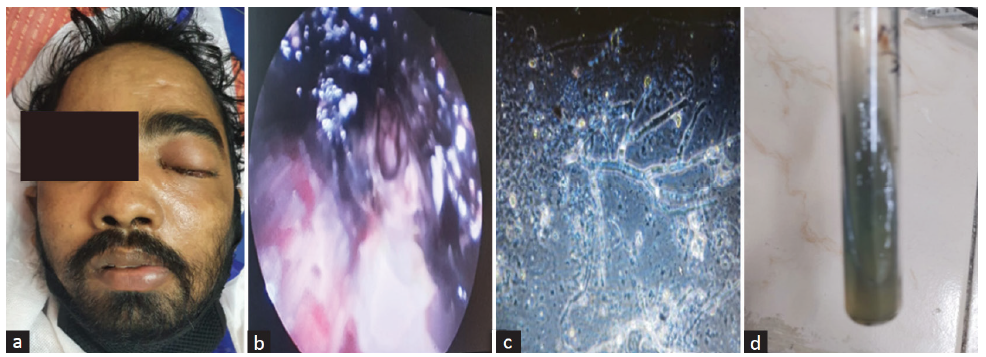
- (a) Patient with abnormal swelling of left half of face. (b) FESS showing black necrotic tissue. (c) Calcofluor immunofluorescence showing fungal hyphae (d) Fungal growth on SDAe. FESS: functional endoscopic sinus surgery, SDA: sabarouds dextrose agar.
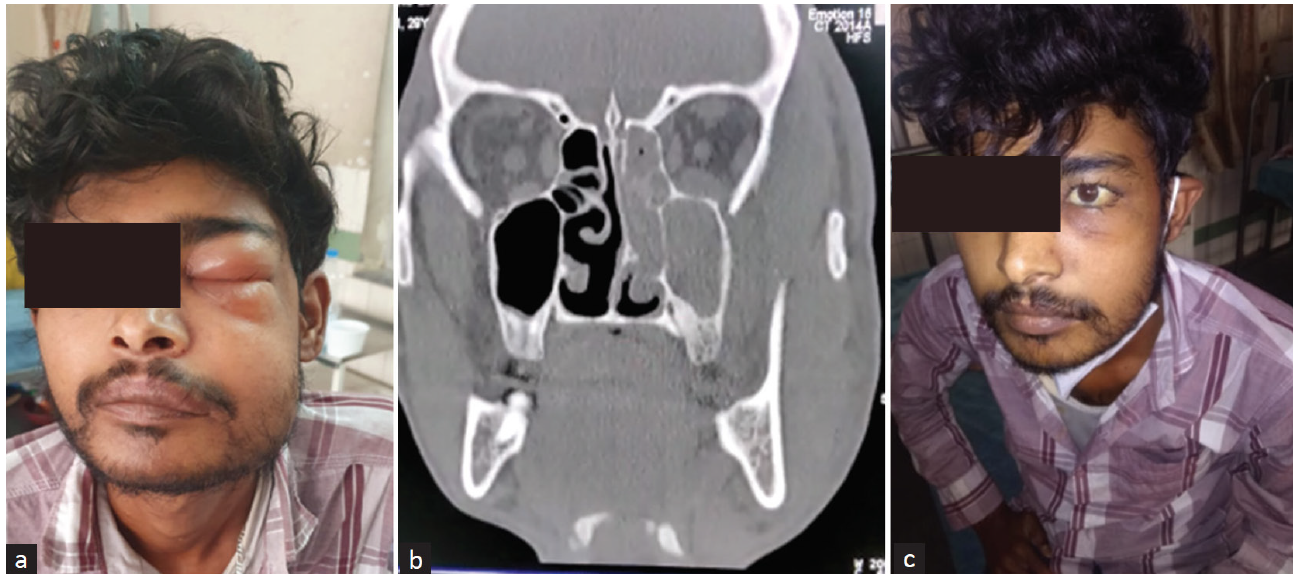
- (a) Dialysis patient with swelling of face and jaw. (b) CT scan image showing maxillary ethmoidal sinusitis (c) Complete recovery after antifungal treatment.

- Dialysis patient with facial swelling, one week after COVID infection.
The TRANSNET study reported that the cumulative incidence of fungal infections in solid organ transplant recipient (SOTR) was 0.07%.3 Coinfections of bacteria and fungi with COVID-19 infection have been on the rise.4 Possible pathophysiological mechanisms of increased fungal infections in COVID-infected patients was thought to be due to delayed resolving of lung parenchymal infection serving as a nidus for fungal infection,5 severe immune dysregulation due to COVID,6,7 prolonged ICU stay, and on mechanical ventilation (98; due to immunosuppressive drugs such as steroids, tocilizumab, and underlying diabetes status.8,9 Our search in PubMed did not show reports of rhinocerebral mucor in either transplant/dialysis patients with COVID infection. A report of heart transplant recipient with mucor and COVID-19 was reported.10
Conclusion
Rhinocerebral mucormycosis following COVID-19 infection is a life-threatening infection in kidney-disease patients. Timely detection and appropriate management with non-nephrotoxic drugs would salvage the immunocompromised patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
References
- Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475-81.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Bacterial and fungal ventilator associated pneumonia in critically ill COVID-19 patients during the second wave. J Infect Public Health. 2021;14:1375-80.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Invasive fungal infections among organ transplant recipients: Results of the Transplant-associated infection surveillance network (TRANSNET) Clin Infect Dis. 2010;50:1101-11.
- [CrossRef] [PubMed] [Google Scholar]
- Co-infections in people with COVID-19: A systematic review and meta-analysis. J Infect. 2020;81:266-75.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Essentials for radiologists on COVID-19: An update-radiology scientific expert panel. Radiology. 2020;296:E113-4.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Fungal co-infections associated with global COVID-19 pandemic: A clinical and diagnostic perspective from China. Mycopathologia. 2020;185:599-606.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Invasive fungal diseases during COVID-19: We should be prepared. J Mycol Med. 2020;30:100971.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- COVID-19 associated pulmonary aspergillosis (CAPA) in patients admitted with severe COVID-19 pneumonia: An observational study from Pakistan. Mycoses. 2020;63:766-70.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Epidemiology of invasive pulmonary aspergillosis among COVID-19 intubated patients: A prospective study. Clin Infect Dis 2020:ciaa1065.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Mucormycosis after Coronavirus disease 2019 infection in a heart transplant recipient – Case report and review of literature. J Mycol Med. 2021;31:101125.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]







