Translate this page into:
Salmonella Aortitis in a Kidney Transplant Patient
Corresponding author: Pradnya Harshe, Department of Nephrology, Kokilaben Dhirubhai Ambani Hospital, Andheri, Maharashtra, India. E-mail: drpradnyaharshe21@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Harshe P, Lad V, Raut A, Kulkarni N. Salmonella Aortitis in a Kidney Transplant Patient. Indian J Nephrol. doi: 10.25259/ijn_166_21
Abstract
Aortitis due to salmonella is a rare complication in kidney transplant recipients. In the general population, mortality among those with salmonella aortitis stands at 60%. We report a case of a kidney transplant recipient diagnosed with Salmonella aortitis affecting the bifurcation of the abdominal aorta. He underwent successful excision of the affected aorta with aortoiliac bifurcation graft replacement along with long-term antibiotic therapy.
Keywords
Salmonella
Renal Transplant
Aortitis
Introduction
Salmonella typhi and S paratyphi are known to infect only humans. Nontyphoidal salmonella (NTS) has a much broader host range, including humans and many vertebrate animals, and is also acquired through food products. In immunocompromised individuals, NTS strains may cause severe invasive disease. In renal transplant recipients, NTS infections may cause invasive infections like urinary tract infections, septic arthritis, pneumonia, lung abscess, and mycotic aneurysms.
Case Report
A 60-year-old man with long-standing diabetes mellitus, hypertension, and chronic kidney disease (CKD) stage 5 due to autosomal dominant polycystic kidney disease underwent a living-related renal transplantation with basiliximab as an induction agent. His postoperative course was uneventful, with a baseline serum creatinine of 1.2 mg/dl. He was on maintenance immunosuppression comprising of tacrolimus (2.25 mg BID), mycophenolate (2gm/day), and prednisolone (5mg OD). Tacrolimus levels were maintained at around 5 ng/ml. Two years after renal transplantation, he presented with low-grade fever and left-sided flank pain of one-month duration. He presented to the emergency in a state of shock.
His serum creatinine was 1.8 mg/dl. His total leukocyte count was 11,210/µL with 87% neutrophils. Hemoglobin (13.2 g/dl) and platelet count (325,000/µL). His tarolimus drug levels were 10.60 ng/ml, and hence the dose was decreased gradually to maintain a trough level of 3–5 ng/ml. Urine culture showed no growth. His blood culture revealed Salmonella, with microbiological tests favoring a nontyphoidal strain sensitive to cephalosporins, ciprofloxacin, piperacillin, and azithromycin and resistant to ampicillin. A computed tomography (CT) scan [Figure 1] showed 8 mm diffuse paraaortic soft tissue in the distal abdominal aorta before its bifurcation, consistent with an infective etiology.
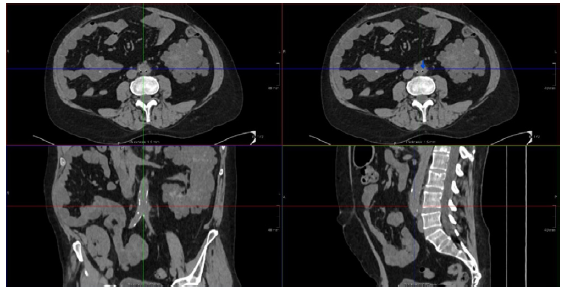
- CT scan image of aortitis. CT: computed tomography.
After empirical antibiotics, based on the antibiotic sensitivity report, he was started on injectable ceftriaxone. He was advised urgent surgical resection of the infected segment of the aorta, but the patient refused. He continued intravenous ceftriaxone for six weeks, at the end of which he returned with the intent to proceed with the surgery. Blood cultures were negative for Salmonella. A CT aortogram [Figure 2] revealed a saccular aneurysm 2.5 cm in diameter along the left posterolateral aspect involving the infrarenal abdominal aorta just before its bifurcation and involving the left common iliac artery. An urgent surgery was recommended.
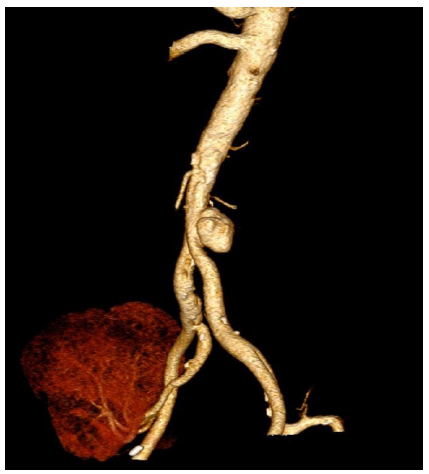
- CT scan image showing aortic aneurysm. CT: computed tomography.
He underwent excision of the infrarenal aorta, its bifurcation, and bilateral common iliac arteries with aortobifemoral reconstruction. Histopathology of the excised specimen revealed [Figure 3] acute transmural inflammation of the aneurysm wall, showing dense neutrophilic infiltrate with numerous histiocytes. Culture of the excised tissue was negative.
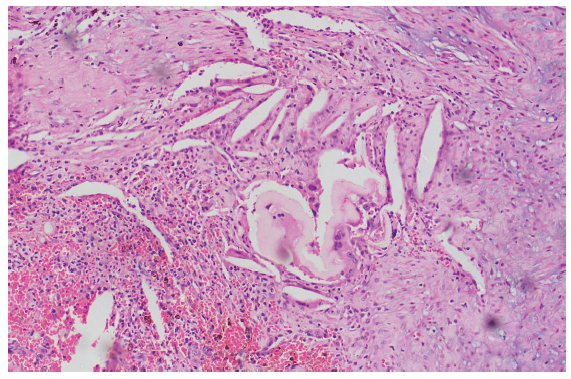
- H&E staining of excised aortic wall. H&E: hematoxylin and eosin.
He was discharged with a serum creatinine of 1.51 mg/dl and continued on ciprofloxacin for six months. He was doing well one year later with a stable renal allograft function.
Discussion
The incidence of nontyphoidal salmonellosis reported in renal transplant recipients is 3.9% in the USA and 3.4% in Saudi Arabia. Soraia-Dunand reviewed 140 cases of salmonella aortitis in 1991. Only one case of post liver transplant and three cases of post renal transplant salmonella aortitis have been reported so far.1
Nearly all cases of aortitis due to salmonella result in aneurysm formation or extension of a preexisting aneurysm.2 Antibiotics alone are not effective and are associated with high mortality. Urgent surgical resection of the infected aorta with wide debridement and interposition grafting is the definitive treatment. Endovascular aortic repair is another option available with lesser mortality but higher recurrence rate. Our patient had an NTS vascular infection (NTSVI) score of 1 and thus at 10.6% risk of developing a vascular infection.3
Conclusion
Almost all patients with infective aortitis will develop aneurysm, therefore early surgery coupled with prolonged antibiotic therapy is highly recommended. This strategy reduces mortality from 96% to 40%.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
References
- Aortitis due to salmonella: Report of 10 cases and comprehensive review of the literature. Clin Infect Dis. 1999;29:862-8.
- [CrossRef] [PubMed] [Google Scholar]
- Evolution of salmonella aortitis towards the formation of abdominal aneurysm. EurRadiol. 1997;7:54-6.
- [CrossRef] [Google Scholar]
- Non-typhoidal salmonella aortitis in a transplant patient. Saudi J Kidney Dis Transpl. 2002;13:501.
- [PubMed] [Google Scholar]







