Translate this page into:
Stent Graft Placement for Treatment of Prosthetic Graft Outflow Stenosis, a Viable Long-term Solution: A Case Report
Address for correspondence: Dr. Pranay Pawar, Department of Vascular Surgery, Sri Ramachandra Medical College, Chennai, Tamil Nadu, India. E-mail: pranay584@yahoo.co.in
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Failing prosthetic grafts in patients undergoing hemodialysis is a common problem. Balloon angioplasty is the first line in treating these stenoses, but it is associated with poor patency rates due to recoil and subsequent restenosis. The use of stent graft implantation has shown very promising early and long-term results as per recent literature. We describe a case of arteriovenous graft outflow stenosis, which led to complete thrombosis of the graft, which was rescued by surgical thrombectomy and stent graft placement across the venous end of the anastomosis with good results.
Keywords
Arteriovenous grafts
hemodialysis
outflow stenosis
stent grafts
Introduction
Prosthetic graft outflow stenosis is a significant complication that may lead to thrombosis unless it is properly managed. Frequent and rapid restenosis associated with balloon angioplasty remains a significant problem. The results of stent graft usage in these patients yield superior results. We describe a case in which we have used a stent graft for a prosthetic graft outflow stenosis with good results along with a review of literature.
Case Report
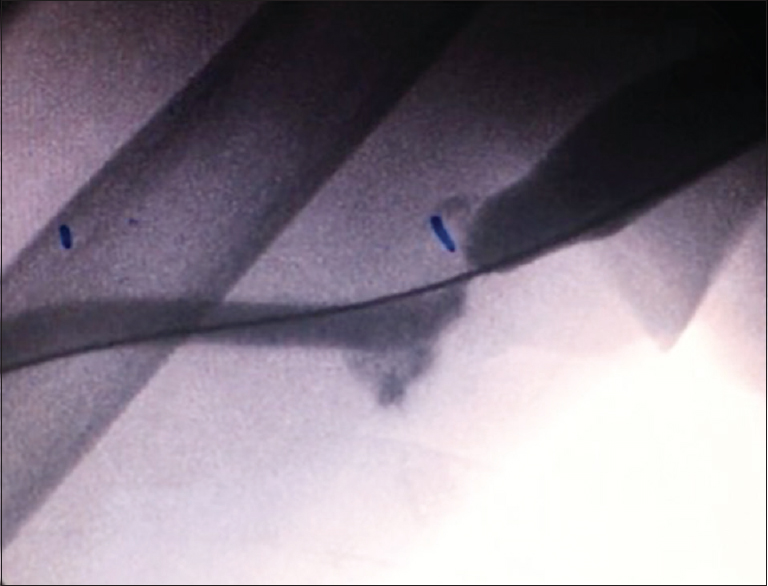
A 68-year-old lady had been on maintenance hemodialysis since 2011 for end stage kidney disease secondary to diabetic nephropathy. She has had multiple fistula failures over the past 5 years and has used tunneled catheters in bilateral internal jugular, subclavian, and femoral veins for a considerable time period. She underwent a right brachiocephalic fistula angioplasty in May 2016, but the fistula thrombosed after 5 months and no further efforts were made to rescue it. In February 2017, she underwent a right brachial artery-axillary vein prosthetic graft procedure with a 6 mm × 30 cm standard wall polytetrafluoroethylene (PTFE) graft. The graft was cannulated after 2 weeks and she had uneventful thrice-weekly hemodialysis till October 2017, when the graft flow abruptly ceased and she was referred to our department for further management. A duplex ultrasound examination showed thrombosis of the graft, with a patent brachial artery and axillary vein. She was taken up for a graft thrombectomy, but post thrombectomy poor back bleed was noted indicating an outflow obstruction to be the cause for the thrombosis. A 6-French (F) sheath was placed in the graft and a check venogram was taken which showed a tight stenosis at the venous outflow of approximately 95% [Figure 1]. A 0.035-inch hydrophilic guide wire and a 4-F diagnostic catheter were used to cross the lesion. After successful crossing, a 6 × 60 balloon catheter was used to dilate the stenosis. Post dilatation, there was significant rate-limiting stenosis with stasis of dye in the graft [Figure 2]. We then used a 7 × 80 self-expanding stent graft (vascular prosthesis with an expanded PTFE encapsulating a nitinol stent framework) across the lesion. Post deployment, we post dilated the stent graft to relieve any residual stenosis. The post procedure contrast runs were normal with complete resolution of the stenosis [Figures 3 and 4]. At 7 months post - procedure, she is doing well with thrice-weekly hemodialysis sessions with 550-600 mL/min blood flow rates and with no increase in venous pressures. She has undergone a venous duplex ultrasound and there is no abnormality reported. She remains on clopidogrel once daily.

- Angiogram showing tight stenosis at the venous anastomosis end of the graft
- Non-resolution of the stenosis after balloon angioplasty

- Placement of a covered stent graft and its dilatation across the stenosis

- Complete resolution of the outflow stenosis post deployment
Discussion
A patent and well-functioning vascular access is paramount for patients undergoing long-term hemodialysis. Although an autogenous arteriovenous fistula is the most favorable type of access, some patients need an artificial graft due to fistula failures, inadequacies of the venous system, or advanced age. Prosthetic grafts are associated with a fair share of problems such as infection risk, thrombosis, and outflow obstruction.[12] In the United States, nearly 75,000 patients undergo hemodialysis treatment using a prosthetic hemodialysis graft. The primary patency of newly placed prosthetic grafts has been reported to be as low as 58% at 6 months and 33% at 18 months.[3] The majority of them develop neointimal hyperplasia which leads to stenosis at the venous anastomosis, which in turn leads to decrease in the blood flow, increase in venous pressures and ultimately thrombosis of the graft. Almost 90% of the graft failures are due to outflow stenosis at venous end of the anastomosis, which can be treated by surgical revision or endovascular procedures.[4] Percutaneous transluminal angioplasty (PTA) gained popularity due to its inherent benefits, but in spite of the initial promising results, long-term results of PTA have been disappointing even with the use of high-pressure balloons. The 6-month primary patencies have been reported from various studies to be as low as 20%–36%, which are well below as the patency expected by the K/DOQI guidelines.[56]
Multiple devices and approaches have been used for treating arteriovenous graft–related stenosis and have been reported in retrospective and prospective randomized trials, but to date none has shown any benefit over balloon angioplasty. These approaches have included angioplasty with cutting/high-pressure balloons, bare metal stenting, brachytherapy, cryotherapy, and anticoagulation therapy.[7] The use of stent graft provides additional support for the graft lumen and creates a mechanical barrier to cover the areas of neointimal hyperplasia thereby preventing the chance of restenosis. Due to the continual outward force of the covered stent graft vessel recoil, trans-stent endothelial ingrowth and in-stent restenosis are hampered. Once deployed, the stent graft converts an end-to-side anastomosis to an functional end-to-end anastomosis, leading to laminar flow and reduction in turbulence and shear stress which again by itself reduces the chance of venous outflow stenosis.[18] Several recent studies have shown increased primary patency of stent grafts when compared with balloon angioplasty. The 2-year results of the RENOVA study showed that stent graft usage provided a two-fold advantage over PTA in treatment area and overall access patency (26.9% vs. 13.5%).[9] A study by Yang et al. showed a post interventional primary patency at 1 year of 46.9% in the stent graft group versus just 7.8% in the balloon angioplasty group. Haskal et al. in their study showed that the patency of the access circuit was more in the stent graft group when compared with the balloon angioplasty group at 6 months (38% vs. 20%).[7] In our patient as the stenosis did not show any resolution after balloon angioplasty, we proceeded to use a stent graft to maintain patency. Although in the Indian scenario cost may be a factor, a decrease in the frequency of re-interventions, increased primary patency and access patency associated with stent graft usage offer a promising and effective solution.
Conclusion
Arteriovenous graft outflow stenosis is a serious and highly prevalent problem. The use of a stent graft is associated with higher patency of the access circuit and provides superior results when compared with balloon angioplasty alone.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- A prospective randomized study of stent graft placement after balloon angioplasty versus balloon angioplasty alone for the treatment of hemodialysis patients with prosthetic graft outflow stenosis. J Vasc Surg. 2018;68:546-53.
- [Google Scholar]
- Risk equation determining unsuccessful cannulation events and failure to maturation in arteriovenous fistulas (REDUCE FTM I) J Am Soc Nephrol. 2006;17:3204-12.
- [Google Scholar]
- Balloon angioplasty versus Viabahn stent graft for treatment of failing or thrombosed prosthetic hemodialysis grafts. J Vasc Surg. 2016;64:1400-10.e1.
- [Google Scholar]
- Patency of autogenous and polytetrafluoroethylene upper extremity arteriovenous hemodialysis accesses: A systematic review. J Vasc Surg. 2003;38:1005-11.
- [Google Scholar]
- NKF-K/DOQI clinical practice guidelines and clinical practice recommendations for 2006 updates: Hemodialysis adequacy, peritoneal dialysis adequacy and vascular access. Am J Kidney Dis. 2006;48:S1-322.
- [Google Scholar]
- Stent-grafts improve secondary patency of failing hemodialysis grafts. J Vasc Access. 2012;13:65-70.
- [Google Scholar]
- Stent graft versus balloon angioplasty for failing dialysis-access grafts. N Engl J Med. 2010;362:494-503.
- [Google Scholar]
- Venous neointimal hyperplasia in polytetrafluoroethylene dialysis grafts. Kidney Int. 2001;59:2325-4.
- [Google Scholar]
- Prospective, randomized, concurrently-controlled study of a stent graft versus balloon angioplasty for treatment of arteriovenous access graft stenosis: 2-year results of the RENOVA study. J Vasc Interv Radiol. 2016;27:1105-14. e3
- [Google Scholar]







