Translate this page into:
Susceptibility weighted imaging: An important tool for early diagnosis of tacrolimus toxicity
Address for correspondence: Dr. A. Verma, Department of Radiodiagnosis, Institute of Medical Sciences, Banaras Hindu University, Varanasi - 221 005, Uttar Pradesh, India. E-mail: drdnv5@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
A 57-year male kidney transplant recipient presented with headache, dizziness, fever and ataxia and weakness in left hand for the past 2 days. This was associated with unsteady gait and slurred speech. The patient was in confused and disoriented state but responsive to external stimulus, with normal vital parameters. Mild weakness in distal muscles of the left hand was noted, and the blood pressure was maintained on medications. Magnetic resonance imaging (MRI) of the brain revealed few small patches of altered signal on the T1- [Figure 1a and b] and T2-weighted images [Figure 1c and d] in bilateral parietal and frontal lobes, few of the lesions showing restricted diffusion on apparent diffusion coefficient maps [Figure 1e and f]. A diagnosis of recurrent cerebral ischemia with few acute infarcts was made, and the patient managed as such. However, a day after admission his neurological status rapidly worsened, and the patient went into coma. A repeat MRI, including susceptibility weighted imaging (SWI) was performed to identify any associated hemorrhage. Multiple areas of “blooming” punctate low signal foci were identified on SWI [Figure 1g and h] involving bilateral cerebral and cerebellar hemispheres as well as deep gray matter and brainstem that were occult on conventional MRI. MR angiography was within normal limits. A close scrutiny of the pattern and morphology led to the diagnosis of tacrolimus induced neurotoxicity. The tacrolimus trough level was 16.3 ng/ml, hence it was decided to discontinue this medication. Over the next few days, the patient's mental status improved drastically.
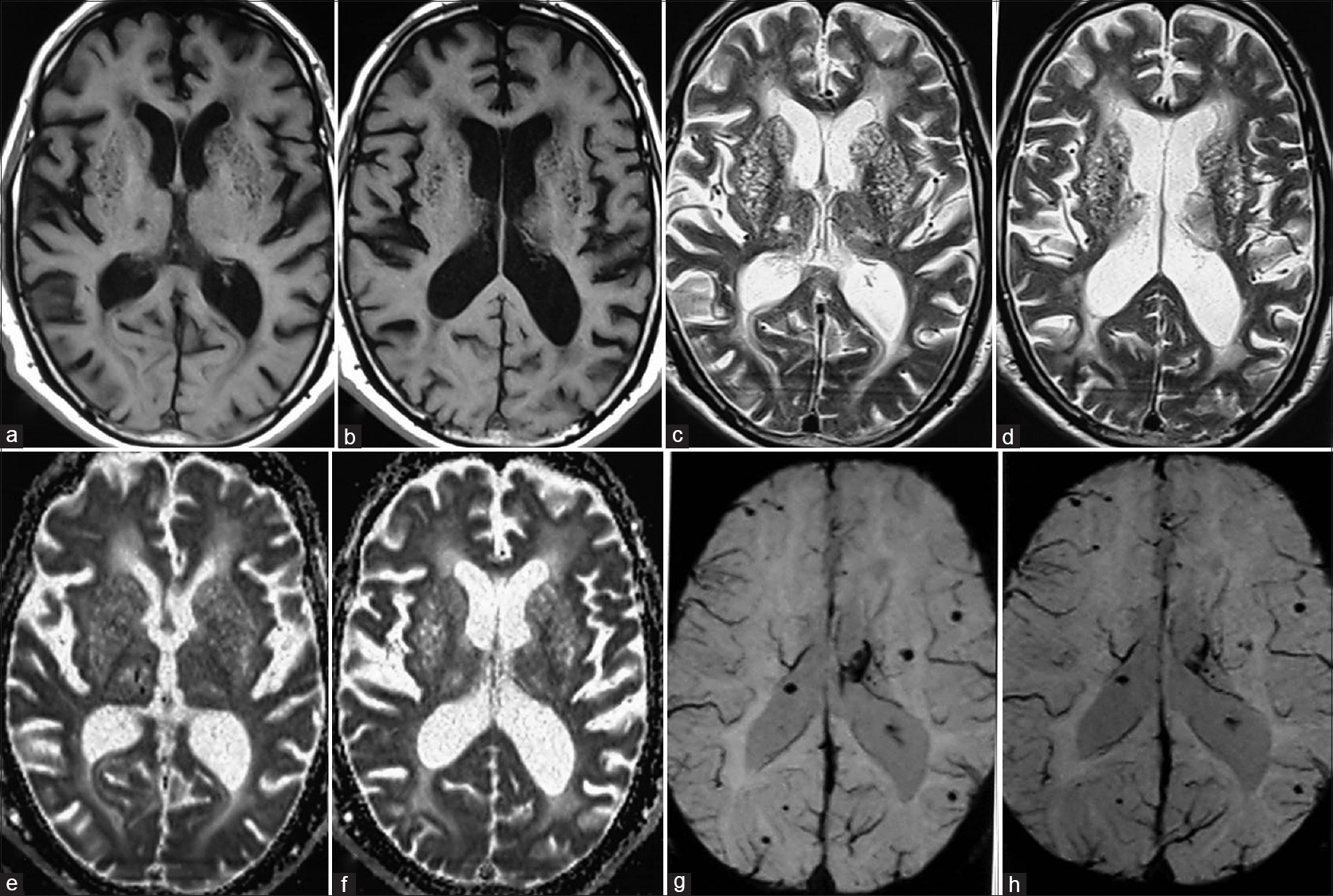
- Magnetic resonance imaging (MRI) showing foci of altered signal on the T1-weighted (a and b) and T2-weighted images (c and d) in cerebral hemispheres, suggesting evolving ischemic foci. Lesions in right thalamus show restricted diffusion on apparent diffusion coefficient maps (e and f). Susceptibility weighted imaging (g and h), shows areas of “blooming” low signal foci involving mainly the superficial subcortical areas of bilateral cerebral hemispheres, with only few lesions in deep gray matter and brainstem (which were occult on conventional MRI). These do not confirm to the typical pattern of hypertensive bleed or hemorrhagic transformation of posterior reversible encephalopathy syndrome
Tacrolimus (FK506) may precipitate neurotoxicity in 10–28% cases[1] usually manifesting as posterior reversible encephalopathy syndrome (PRES)[2] characterized by vasogenic edema predominantly involving posterior parts of the brain.[3] However, with increased clinical experience and advances in MRI technology, other nontypical patterns have been encountered and are thought to represent earlier stages and different pathophysiological events induced by tacrolimus. These include the presence of intraparenchymal hemorrhages, isolated brainstem involvement, lesions without posterior predilection and evidence of cytotoxic edema.[4] Multifocal punctate intraparenchymal hemorrhages in a patient receiving tacrolimus is an entity distinct from the hemorrhagic transformation of PRES and is seen in early “potentially reversible” stages of drug toxicity. This represents vasculitis caused directly due to toxic effects of the drug.[24] SWI is a new MR sequence that is being increasingly used to detect minimal and early intracranial bleed.[5] In one case series, plasma drug level measurements had a low sensitivity of 27% for suspecting the complication while MRI suspected the diagnosis with 80% sensitivity.[45] As high incidence of microhemorrhages has been associated with this syndrome, SWI should always include in procuring the diagnosis of tacrolimus toxicity.
References
- Brain MR imaging abnormalities in kidney transplant recipients. AJNR Am J Neuroradiol. 2005;26:2282-9.
- [Google Scholar]
- Neurotoxicity of calcineurin inhibitors: Impact and clinical management. Transpl Int. 2000;13:313-26.
- [Google Scholar]
- Reversible tacrolimus-induced neurotoxicity isolated to the brain stem. AJNR Am J Neuroradiol. 2000;21:1251-4.
- [Google Scholar]
- Posterior reversible encephalopathy syndrome, part 1: Fundamental imaging and clinical features. AJNR Am J Neuroradiol. 2008;29:1036-42.
- [Google Scholar]
- Detection of microhemorrhage in posterior reversible encephalopathy syndrome using susceptibility-weighted imaging. AJNR Am J Neuroradiol. 2012;33:896-903.
- [Google Scholar]






