Translate this page into:
TAFRO Syndrome Treated Effectively with Corticosteroids: A Case Report and Review of the Literature
Address for correspondence: Dr. Hasan Sozel, Department of Internal Medicine, Faculty of Medicine, Akdeniz University, Antalya, Turkey. E-mail: dr07hasan@hotmail.com
-
Received: ,
Accepted: ,
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
TAFRO (thrombocytopenia, anasarca, fever, renal dysfunction, and organomegaly) syndrome is a subtype of Castleman's disease and has been described in recent years. In this case, a middle-aged woman was admitted to our clinic with a 2-week history of fever, weakness, cough, shortness of breath and edema all over the body. Physical examination on admission revealed pale conjunctiva, tachycardia, coarse crackles over left lower lung fields, pitting edema in the extremities, tense ascites, axillar, and bilateral inguinal lymph nodes measuring less than 2 cm. Inguinal lymph node excisional biopsy was compatible with TAFRO syndrome. We started corticosteroid treatment. The patient's general condition and physical findings improved. Laboratory values returned to normal limits. This case will help understand the clinical course and treatment strategy in TAFRO syndrome.
Keywords
Castleman's disease
corticosteroid treatment
TAFRO syndrome
Introduction
Castleman's disease (CD) is a rare nonmalignant lymphoproliferative disorder and presents with lymph node hyperplasia.[1] Surgical removal of the node is necessary for the diagnosis of CD.[2] Based on the degree of lymph node involvement, the CD is classified as unicentric CD (UCD) or multicentric CD (MCD). MCD is divided into HHV-8-related MCD and HHV-8-negative or idiopathic MCD (iMCD) due to human herpes virus–8 (HHV-8). The etiology and risk factors of iMCD are not known, and it is a very rare syndrome. TAFRO (thrombocytopenia, anasarca, fever, renal dysfunction, and organomegaly) syndrome, POEMS (peripheral neuropathy, organomegaly, endocrinopathy, monoclonal gammopathy, and skin changes) syndrome, and iMCD–not otherwise specified (iMCD-NOS) are subtypes of iMCD.[34]
TAFRO syndrome, which was first reported in 2010, is a new disease concept, presenting as clinical features characterized by severe thrombocytopenia (T), massive fluid retention with anasarca (A), fever (F), renal dysfunction (R), and organomegaly (O), and multiple mild lymphadenopathies, with atypical CD histopathology.[356] Diagnostic criteria for TAFRO syndrome were published in 2016.[7] The median age of TAFRO syndrome onset is 50 years (range, 23–72)[3] Complete remission rates following corticosteroid therapy are lower in TAFRO syndrome than those in classical MCD.[6]
Herein, we present a typical case of a Turkish woman with TAFRO syndrome treated with glucocorticoid and a review of the literature. Her clinical symptoms, radiologic, and laboratory findings markedly improved after prednisolone treatment.
Case Presentation
A 50-year-old woman was admitted with a 2-week history of fever, weakness, cough, shortness of breath, and edema all over the body. Her past medical history was unremarkable, and she neither drank alcohol nor smoked. Physical examination on admission revealed pale conjunctiva, tachycardia (110/minute), coarse crackles over left lower lung field, pitting edema in the extremities, tense ascites, axillar and bilateral inguinal lymph nodes measuring less than 2 cm. Neither petechial nor purpuric lesions were present. Initial laboratory investigations are shown in Table 1. Bilateral effusion was observed on the chest X-ray of the patient [Figure 1a]. Abdominal ultrasonography showed hepatosplenomegaly and widespread acid. A positron emission tomography/computed tomography (PET/CT) was ordered with the suspicion of lymphoma or malignancy. In PET/CT, there were left submandibular, right subclavicular, bilateral axillary, left para-aortic, and bilateral inguinal hypermetabolic lymph nodes. A view was compatible with nonmetabolic effusion in the pericardial, bilateral pleural area and compatible with nonmetabolic acid in the pelvic area. Hepatosplenomegaly was present, and the spleen showed heterogeneous increased fluorodeoxyglucose (FDG) uptake (SUVmax: 6.4). In addition, mild diffuse heterogeneous FDG uptake was observed in the bone marrow [Figure 2].
| Complete blood count | Serologic test | Biochemistry | |||
|---|---|---|---|---|---|
| Hemoglobin | 8.1 g/dL | HBsAg | (−) | BUN | 29.24 mg/dL |
| MCV | 82 fL | HCVAb | (−) | Creatinine | 1.41 mg/dL |
| White blood cells | 8.730/mm3 | HIV Ab | (−) | Uric acid | 10.7 mg/dL |
| Segmented | 78.8% | CMV IgM | (−) | ALT | 5 U/L |
| Lymphocytes | 11.9% | EBV IgM | (−) | AST | 16 U/L |
| Monocyte | 8.7% | HHV-8-DNA | (−) | LDH | 331 U/L |
| Platelet | 51000/mm3 | Parvovirus IgM | (−) | ALP | 204 U/L |
| Reticulocyte | 0.43% | Toxoplasma IgM | (−) | Total bilirubin | 0.4 mg/dL |
| Coagulation test | Brucella Agglutination | (−) | Glucose | 142 mg/dL | |
| Prothrombin time | 19.2 sec | Syphilis | (−) | CRP | 20.93 mg/dL |
| APTT | 42.2 sec | Rubella IgM | (−) | Ferritin | 243 ng/mL |
| INR | 1.44 | Immunologic test | Na | 142 mEq/L | |
| Fibrinogen | 752 mg/dL | IgG | 1,222 mg/dL | K | 4.9 mEq/L |
| D-dimer | 11.5 µg/dL | IgA | 230 mg/dL | Cl | 106 mEq/L |
| Antithrombin III | 65 | IgM | 228 mg/dL | Total protein | 5.56 mg/dL |
| Urine test | ANA | (−) | Albumin | 2.85 mg/dL | |
| Urine glucose | (−) | C3 | 149 mg/dL | Calcium | 7.65 mg/dL |
| Urine protein | (1+) | C4 | 31 mg/dL | ESR | 84 mm/h |
| Urine occult blood | (−) | IEP | (−) | Vitamin B12 | 306 mg/dL |
| Urine Ph | 5.5 | Coombs tests | (−) | Folate | 5.3 mg/dL |
MCV=mean corpuscular volume; APTT=activated partial thromboplastin; BUN=blood urea nitrogen; AST=aspartate aminotransferase; ALT=alanine aminotransferase; LDH=lactate dehydrogenase; ALP=alkaline phosphatase; CRP=C-reactive protein; HBsAg=hepatitis B antigen; HCVAb=hepatitis C virus antibody, HIV=human immunodeficiency virus; EBV=Epstein-Barr virus; CMV=cytomegalovirus; HHV-8=human herpesvirus-8; IEP=serum immunoelectrophoresis ; ANA=antinuclear antibody test ; IgG, A, M=immunoglobulin G, A, M; C3, 4=Complement 3, 4; ESR=erythrocyte sedimentation rate

- Chest X-ray imaging (a) at the admission and (b) 2 weeks after the beginning of corticosteroid treatment
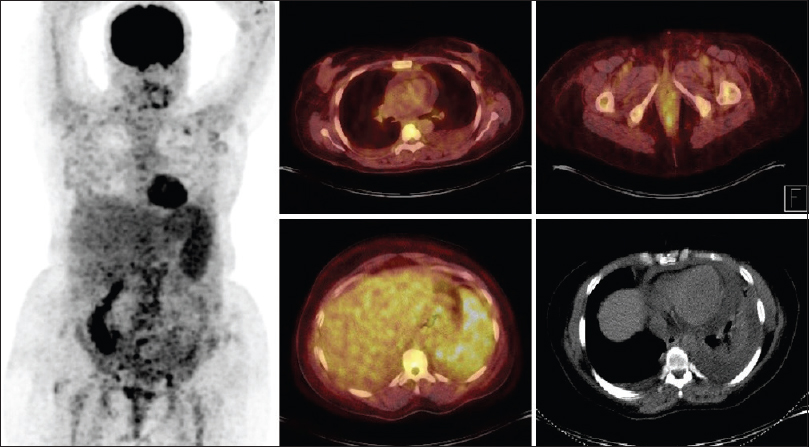
- Whole-body 18-F-fluorodeoxyglucose (FDG)–positron emission tomography/computed tomography at the admission revealed hepatosplenomegaly, the spleen with heterogeneous increased FDG uptake (SUVmax: 6.4), left submandibular, right subclavicular, bilateral axillary, left para-aortic, and bilateral inguinal hypermetabolic lymph nodes, and there was a view compatible with nonmetabolic effusion in the pericardial and bilateral pleural area
Bone marrow aspiration was attempted from the ilium but was a dry tap. Bone marrow biopsy revealed a normocellular marrow with increased megakaryocytes and no infiltration of atypical lymphocytes [Figure 3].

- Histological findings of the lymph node (a) Hematoxylin–eosin (H and E) ×200, (b) H and E × 400, (c) Kappa × 400, and bone marrow (d) Lambda × 400. A field of the bone marrow showed hypercellular bone marrow with slightly increased angiogenesis. There was no infiltration of atypical lymphoid cells
Based on these findings, lymphoma, CD, or systemic lupus erythematosus was considered in the preliminary diagnosis, and an inguinal lymph node biopsy was performed. After the lymph node biopsy, corticosteroid therapy with 250 mg of IV prednisolone for 3 days was started, followed by 40 mg daily. Anasarca, ascites, pleural effusion, fever, shortness of breath, and superficial lymphadenopathy showed immediate improvement, and creatinine, CRP, and ESR were decreased to within normal range. On the chest X-ray 2 weeks after the initiation of steroid therapy, the costo-diaphragmatic sinuses were open [Figure 1b]. Immunohistochemically, a few small dendritic reticular cell clusters are observed with CD23. Besides, CD138, kappa light chain (κ), and lambda light chain (λ) were scattered with many positive cells. Vascular proliferation, atrophic follicles, enlarged interfollicular area, and the presence of many polyclonal plasma cells were consistent with the findings described in TAFRO syndrome. The patient was discharged and followed up by the internal medicine department.
Discussion
TAFRO syndrome is a rare systemic inflammatory disease that has been recently identified with features such as thrombocytopenia (T), anasarca (A), fever (F), renal dysfunction (R), and organomegaly (O), and challenging to diagnose. Whether TAFRO syndrome is an independent entity or a subvariant of iMCD is still controversial. Immunosuppressive therapy is very effective, so we can suggest that it can be an immunologic disorder. Differential diagnoses of TAFRO syndrome include viral/bacterial infections and rheumatological diseases such as systemic lupus erythematosus (SLE) [Table 2]. SLE often presents with systemic symptoms such as fatigue, fever and is associated with lymphadenopathy, pleural and pericardial effusion, and immune thrombocytopenia. SLE was ruled out in this case because specific autoantibodies were negative and the classification criteria were not satisfied. We also considered hematopoietic malignancies, including Hodgkin's and non-Hodgkin's lymphoma. The patient underwent a bone marrow biopsy, and the result was reported as a hypercellular bone marrow biopsy with dysmegakaryopoiesis. The size of the lymph nodes in TAFRO syndrome is generally below 1.5 cm in diameter. Large lymphadenopathy may indicate lymphoma. In our case, the mild enlargement (<10 mm) of axillary and inguinal lymph nodes was also detected in PET/CT. Although we diagnosed inguinal lymph node excision with low FDG involvement, we detected it in PET/CT. There are no sufficient data about FDG PET-CT in the diagnosis of TAFRO syndrome. The most appropriate treatment for TAFRO syndrome is not yet known.[37]
| Differential diagnoses | Multiple mild lymphade nopathies | Constitutional symptoms | Organomegaly | Fluid accumulation (anasarca) | Interstitial pneumonitis | Renal dysfunction | HHV-8 PCR | Viral serology | Autoimmune markers (ANA) |
|---|---|---|---|---|---|---|---|---|---|
| TAFRO syndrome | + | + | + | + | + | + | − | − | − |
| Lymphoma | + | + | + | − | − | − | − | +/− | − |
| Tuberculosis | + | + | − | − | + | − | − | − | − |
| HHV-8 | + | + | + | − | − | − | + | − | − |
| EBV/CMV/TOXO/HIV | + | + | + | − | − | − | − | + | − |
| SLE | − | + | +/− | + | − | + | − | − | + |
TAFRO=thrombocytopenia, anasarca, fever, renal dysfunction, and organomegaly; HHV-8=Human herpesvirus 8; PCR=polymerase chain reaction; ANA=antinuclear antibody; EBV=Epstein-Barr virus; CMV=cytomegalovirus; TOXO=toxoplasma, HIV=human immunodeficiency virus; SLE=systemic lupus erythematosus
The first case in Japan responded to steroid treatment; however, a successful response to thrombocytopenia and anasarca was not achieved.[368] Patients with TAFRO syndrome have been treated with steroids alone, steroid and immunosuppressant therapy combinations, or interleukin 6 antagonists.[37] Despite the treatment, some patients died because of the disease. Middle-aged patients benefit more from steroid therapy. In one series, a single corticosteroid was able to control the disease in 47.8% of patients.[3] In the present case, our patient, showed immediate improvement to steroid treatment; her general condition improved, and laboratory values returned to normal limits.
For more successful treatments, the pathophysiology of TAFRO syndrome should be fully clarified. We believe that new treatment protocols related to this disease will be developed as we see new cases and follow-up times of the patients increase.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Castleman disease: An update on classification and the spectrum of associated lesions. Adv Anat Pathol. 2009;16:236-46.
- [Google Scholar]
- Recurrence in unicentric castleman's disease postoperatively: A case report and literature review. BMC Surg. 2018;18:1.
- [Google Scholar]
- Clinicopathologic analysis of TAFRO syndrome demonstrates a distinct subtype of HHV-8-negative multicentric Castleman disease. Am J Hematol. 2016;1:220-6.
- [Google Scholar]
- Tafro syndrome: A case report from turkey and review of the literature. Int J Hematol Stem Cell Res. 2018;12:252-8.
- [Google Scholar]
- Thrombocytopenia with mild bone marrow fibrosis accompanied by fever, pleural effusion, ascites and hepatosplenomegaly. Rinsho Ketsueki. 2010;51:320-5.
- [Google Scholar]
- Castleman-Kojima disease (TAFRO syndrome): A novel systemic inflammatory disease characterized by a constellation of symptoms, namely, thrombocytopenia, ascites (anasarca), microcytic anemia, myelofibrosis, renal dysfunction, and organomegaly: A status. J Clin Exp Hematop. 2013;53:57-61.
- [Google Scholar]
- Proposed diagnostic criteria, disease severity classification and treatment strategy for TAFRO syndrome, 2015 version. Int J Hematol. 2016;103:686-92.
- [Google Scholar]
- Thrombocytopenia with reticulin fibrosis accompanied by fever, anasarca and hepatosplenomegaly : A clinical report of five cases. J Clin Exp Hematop. 2013;53:63-8.
- [Google Scholar]







