Translate this page into:
Teriparatide Improves Bone Formation Markers and Bone Mineral Density in Adynamic Bone Disease Associated with Chronic Kidney Disease
Corresponding author: Vijoy Kumar Jha, Department of Nephrology, Base Hospital, Delhi Cantt, India. E-mail: vkjhamd@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Jha VK, Abhisheka K, Akal RS, Mahapatra D, Rai SK. Teriparatide Improves Bone Formation Markers and Bone Mineral Density in Adynamic Bone Disease Associated with Chronic Kidney Disease. Indian J Nephrol. 2024;34:254–6. doi: 10.25259/ijn_555_23
Dear Editor,
Adynamic bone disease (ABD), a low bone turnover disease without osteoid accumulation with a faulty rate of collagen synthesis and mineralization has emerged as the most common mineral bone disorder (MBD) associated with chronic kidney disease (CKD).1,2 Relatively low/normal parathyroid hormone (PTH) is considered a surrogate marker of low bone turnover and identifies increased fracture risk in ABD. It has been hypothesized that teriparatide (PTH 1-34) would be effective for ABD based on its ability to promote both osteoblast and osteoclast activity.
This was a single-center prospective cohort study conducted on CKD patients with ABD (serum PTH 150 pg/ml in those on dialysis and <65 pg/ml in those not on dialysis). The study was approved by the Institutional Ethics Committee at Command Hospital Air Force Bangalore, India, number IEC/01/2020/24, dated 26th June 2020. Individuals with no contraindication were given teriparatide. Bone mineral density (BMD) and serologic markers of bone turnover were assessed at baseline, 3 months, and after 6 months. Serum calcium, phosphate, 25(OH) vitamin D, and other routine biochemical parameters were also assessed.
A total of 71 patients were included, out of which 55 patients completed the study; 42 patients (76.4%) were male, and 13 (23.6%) were female. The mean age was 48.64 ± 13.91 years. The mean BMI was 21.73 ± 4.11 kg/m2. The number of patients with diabetes was 36 (65.5%). Of those on dialysis, 72.7% were on HD. Dialysis vintage was 22.96 ± 21.63 months (mean ± SD). The history of fracture was in only eight patients (14.5%). With inj. teriparatide treatment after stopping vitamin D analogs, serum calcium level decreased significantly after 6 months (p = 0.036). Change in intact PTH was significant after 6 months (p < 0.0001). By using analysis of variance, changes in bone-specific alkaline phosphatase (BSAP), Procollagen type 1 amino-terminal propeptide (P1NP), and BMD (both neck of the left femur and lumbar spine) were significant (p < 0.0001) after 6 months [Figure 1a-d]. There were significant changes in intact PTH, BSAP, and BMD (both neck of femur and lumbar spine) from baseline and after 3 months [Table 1] and from 3 months and after 6 months. Similar changes were not observed in the P1NP level. In the diabetic population, the observed change in BSAP, and BMD neck of femur was less as compared to nondiabetics, but it was not statistically significant [change in BSAP − mean (SD) 9.42 (4.90) vs 10.71 (3.63), p = 0.28 and change in BMD neck of femur − mean (SD) 0.27 (0.10) vs 0.30 (0.10), p = 0.35]. In the female population, there was less change in BSAP [9.65(4.03) vs 10.46(4.17)], p = 0.54. Similarly, there was no significant difference in the change of BMD in males and females. No significant differences in BSAP and BMD changes were observed in the fracture group and nonfracture group. There were no significant effects observed on other biochemical parameters like serum albumin, serum ferritin, serum transaminases, and serum electrolytes (sodium/potassium). Hemoglobin improvement with less requirement of erythropoietin was observed but it was statistically insignificant.
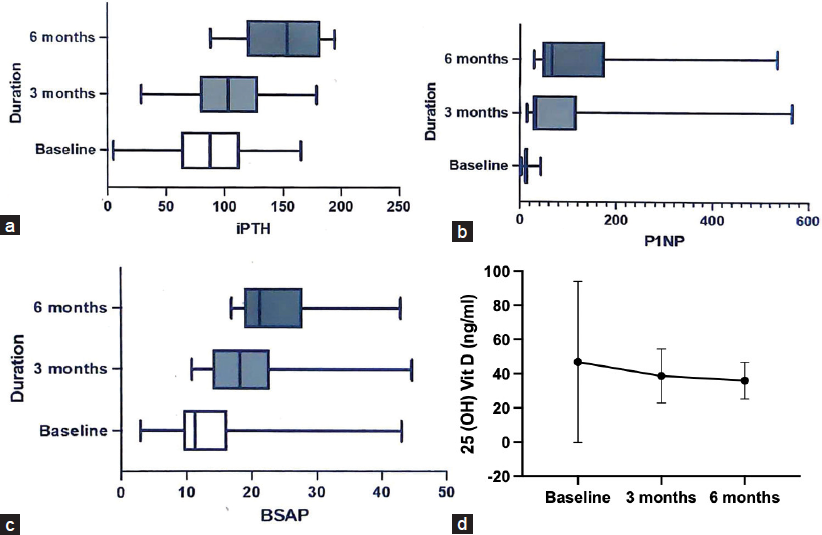
- Changes in (a) intact PTH (b) P1NP (c) BSAP (d) 25(0H) Vit D at baseline, 3, and 6 months after inj teriperatide administration. iPTH: intant parathyroid hormone, P1NP: procollagen type 1 N-terminal propeptide, BSAP: bone-specific alkaline phosphatase, 25(OH) Vit D: 25-hydroxy vitamin D
| Parameters | Baseline mean | After 3 months mean | Difference between baseline and 3 months (mean ± SEM) | p | After 6 months mean | Difference between 3 months and 6 months (mean ± SEM) | p |
|---|---|---|---|---|---|---|---|
| Intact PTH (CLIA) pg/ml | 85.85 | 103 | 17.17 ± 6.513 | 0.0095 | 149.9 | 46.85 ± 6.185 | 0.0001 |
| Serum bone-specific alkaline phosphatase (immunoassay) µg/l | 13.37 | 19.96 | 5.782 ± 1.275 | <0.0001 | 23.64 | 4.484 ± 1.276 | 0.0006 |
| Serum Procollagen type 1 aminoterminal propeptide (ECLIA) ng/ml | 70.01 | 87.94 | 17.92 ± 18.68 | 0.3396 | 114.4 | 26.49 ± 20.61 | 0.2014 |
| Bone mineral density—neck of left femur gm/cm2 | 0.5795 | 0.698 | 0.1203 ± 0.033 | 0.0005 | 0.8696 | 0.1698 ± 0.03295 | <0.0001 |
| Bone mineral density—Lumbar spine gm/cm2 | 0.7632 | 0.9055 | 0.1422 ± 0.03697 | 0.0002 | 1.019 | 0.1132 ± 0.03830 | 0.0038 |
PTH: parathyroid hormone, CLIA: Chemiluminescent immunoassay, ECLIA: Electrochemiluminescence, SEM: Standard error mean.
No significant side effects were observed during these 6 months of study. No instances of symptomatic hypotension were observed. Increased age, diabetes, high calcium load, vitamin D excess, aggressive treatment of hyperparathyroidism, low PTH levels, parathyroidectomy, systemic inflammation, calcimimetics, and bisphosphonates are commonly implicated in ABD pathogenesis.3,4 Kidney Disease Improving Global Outcome suggests maintaining intact PTH levels in the range of approximately two to nine times the upper limit normal for the assay.5 Although bone biopsy remains the gold standard for diagnosis of high vs normal vs low turnover bone disease, the patient’s acceptability and availability of bone biopsies are often issues in patients with CKD. Therefore, there is a need to develop noninvasive markers of bone turnover. Intact PTH < 150 pg/ml and BSAP < 25 µg/l were taken as cut-off values for inclusion in our study for dialysis-dependent patients. The value of intact PTH and BSAP has increased with inj. teriparatide therapy significantly after 3 months and 6 months of therapy. Although ideally intact P1NP should be used, due to unavailability we have used total P1NP and have followed its trend while on therapy. The change in P1NP was not significant after 3 months of therapy from baseline and after 6 months of therapy from 3 months. Therefore, it may be presumed that P1NP should not be considered as a suitable marker for treatment response in the early part of therapy. Intermittent administration of exogenous PTH stimulates bone formation in association with an increase in bone remodeling rate. Although BMD changes will be more evident after 12–24 months of therapy, there are studies where significant BMD changes are evident with teriparatide injection even with 3–6 months of treatment.6 As the study duration was only 6 months, BMD measurements were proposed to be done at baseline, 3, and 6 months of teriparatide injection. In the present study, BMD had shown marked improvement both at the neck of the femur and lumbar spine as early as 3 months and the improvement continued up to 6 months of therapy. Further studies will be needed to substantiate the long-term effect of BMD on the continuation of inj. teriparatide.
PTH therapy as one might expect to increase serum calcium level but the present study did not reveal any significant changes in the serum calcium level. 25 (OH) Vit D value has also not changed significantly. This may be because only vitamin D deficient patients (<20 ng/ml) were administered vitamin D supplements and all those patients with low intact PTH stopped taking vitamin D analogs. PTH therapy was continued for a minimum 6-month period and was planned to continue till intact PTH rises to a maximum nine times the upper limit normal or a total of two years duration, whichever is earlier.
The study was limited by its short duration and small number of patients. The objective was only to measure improvement in biochemical parameters and BMD and not any patient or clinical-related outcomes.
In conclusion, inj. teriparatide is an effective therapy to improve bone formation markers and BMD in the setting of adynamic bone disease in dialysis-dependent populations. Further studies along with bone biopsy through bone histomorphometry are needed to know the long-term effects of this therapy.
Financial support and sponsorship
Received through Armed Forces Medical Research Committee (AFMRC) project no. 5472/2021 by O/o DGAFMS, MoD.
Conflicts of interest
There are no conflicts of interest.
References
- Spectrum of renal bone disease in end-stage renal failure patients not yet on dialysis. Nephrol Dial Transplant. 2003;18:1159-66.
- [CrossRef] [PubMed] [Google Scholar]
- Renal bone disease in 76 patients with varying degrees of predialysis chronic renal failure: A cross-sectional study. Nephrol Dial Transplant. 1996;11:813-9.
- [CrossRef] [PubMed] [Google Scholar]
- Evidence for abnormal calcium homeostasis in patients with adynamic bone disease. Kidney Int. 1994;46:855-61.
- [CrossRef] [PubMed] [Google Scholar]
- Renal osteodystrophy in predialysis and hemodialysis patients: Comparison of histologic patterns and diagnostic predictivity of intact PTH. Nephron. 2002;91:103-11.
- [CrossRef] [PubMed] [Google Scholar]
- KDIGO 2017 clinical practice guideline update for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease-mineral and bone disorder (CKD-MBD) Kidney Int Suppl (2011). 2017;7:1-59.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The effect of teriparatide therapy on bone density in men with osteoporosis. J Bone Miner Res. 2003;18:9-17.
- [CrossRef] [PubMed] [Google Scholar]






