Translate this page into:
Thrombotic Thrombocytopenic Purpura and Ulcerative Colitis – A Potential Link Revisited
Address for correspondence: Dr. Lovy Gaur, Max Superspeciality Hospital, W-3, Sector-1, Vaishali, Ghaziabad - 201 012, Uttar Pradesh, India. E-mail: drlovygaur@gmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Inflammatory bowel disease is known to be associated with several extraintestinal manifestations including haematological abnormalities. The association between ulcerative colitis and thrombotic thrombocytopenic purpura is largely anecdotal, described in only two case reports so far. While the existence of association remains a matter of research, what is clear is the need for prompt recognition of this complication and expedient treatment which may be life-saving. Here, we describe a patient with ulcerative colitis who developed thrombotic thrombocytopenic purpura.
Keywords
Thrombotic thrombocytopenic purpura
Thrombotic thrombocytopenic purpura
ulcerative colitis
Introduction
Thrombotic thrombocytopenic purpura (TTP) is an acquired disease due to autoantibodies against ADAMTS13 (a disintegrin and metalloprotease with thrombospondin type 1 repeats, member 13).[1] While its association with connective tissue disorders is well described, there are only two case reports describing its possible association with ulcerative colitis.[23] We describe a patient who developed TTP two weeks following flare of ulcerative colitis.
Case Report
A 31-year-old man, was admitted to intensive care unit in view of status epilepticus. His past history was significant for ulcerative colitis diagnosed 2 years ago – with pseudopolyps seen throughout the colon and proctosigmoiditis. Rectal biopsy revealed features of ulcerated mucosal fragments, cryptitis and crypt abscesses. He was initiated on oral prednisolone along with local and systemic mesalazine. The gastrointestinal symptoms abated but he discontinued this treatment on his own after 6 months and remained asymptomatic for the next year and a half.
About a month prior to this admission, the patient experienced a flare of ulcerative colitis– with loose stools, bleeding per rectum and fatigue. He was reinitiated on mesalazine and prednisolone (0.5 mg/kg/day) on outpatient basis by a gastroenterologist. He developed thrombosis of right common femoral vein about 10 days after starting this treatment, for which he was prescribed unfractionated heparin with rivaroxaban. He developed hematochezia again, which persisted despite withdrawal of anticoagulants.
The patient developed generalized tonic clonic seizures after 2 weeks and was admitted to ICU in our hospital. Persistent convulsive activity and concern for airway protection necessitated intubation and sedation with midazolam. On physical examination, the patient was normotensive (blood pressure –130/60 mmHg) and pale. Examination of cardiovascular and respiratory systems was unremarkable and there was no organomegaly on abdominal palpation. Serum electrolytes, calcium and magnesium were within the normal limits. Magnetic resonance imaging of brain including arteriography and venography were unremarkable. Laboratory investigations done on the first day were notable for anemia (Hb- 8.3 gm/dl), thrombocytopenia (platelet count 1.1 lakh/mm3) and deranged kidney function (serum creatinine - 3.25 mg/dl). The very next day, his hemoglobin dropped to 5.5 gm/dl and platelets to 65,000/mm3. Peripheral smear [Figure 1] revealed crenated red blood cells and schistocytes (15%); lactate dehydrogenase (LDH) was elevated (827 IU/L) and serum haptoglobin levels were suppressed (1.3 mg/dl). Direct and indirect Coombs tests were negative. Activated partial thromboplastin time, prothrombin time and fibrinogen levels were within normal limits. In view of constellation of features of microangiopathic hemolytic anemia, thrombocytopenia, seizures and renal dysfunction a presumptive diagnosis of thrombotic thrombocytopenic purpura was made. He was initiated on plasmapheresis; dose of prednisolone was escalated to 1.0 mg/kg/day. Meanwhile, the laboratory work up to rule out other causes of microangiopathic hemolytic anemia revealed normal serum B12 levels (349 pg/ml), negative serologies for antinuclear antibodies (ANA) and antiphospholipid antibodies (APLA) and stool test negative for Shiga toxin. ADAMTS13 activity was 57% (normal - 68-163%) as tested by chromogenic enzyme linked immunoassay, however the levels were measured after the patient had received two sessions of plasmapheresis. Patient improved with this treatment. He was extubated on day 3 of admission. After 10 plasmapheresis sessions laboratory investigations revealed Hb –6.2 gm/dl, platelets –1,65,000/mm3 and creatinine –1.2 mg/dl. Trends with respect to these parameters and plasmapheresis therapy have been highlighted in Figure 2.
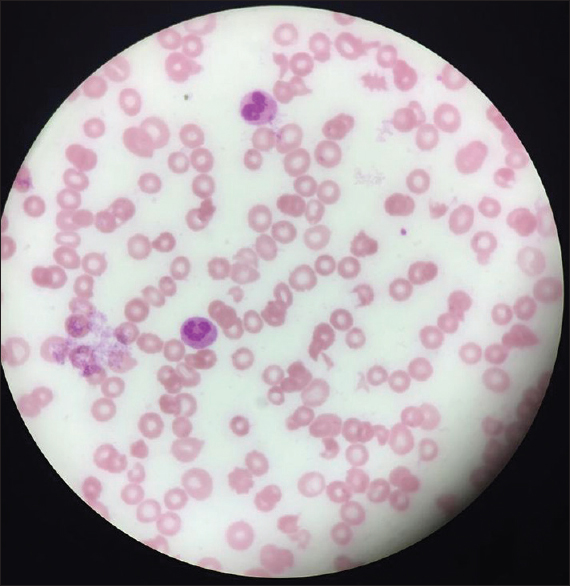
- Peripheral smear showing schistocytes
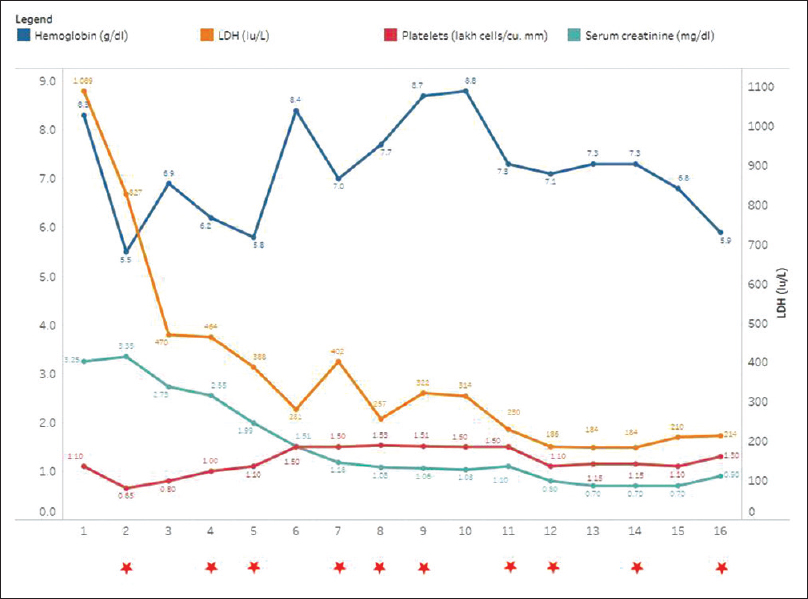
- Trends of laboratory parameters (Hemoglobin (g/dl), lactate dehydrogenase levels (IU/L), platelets (lakh cells/cumm) and serum creatinine (mg/dl) - pre-plasmapheresis values). Stars marked against the days on which plasmapheresis was done
Till his last outpatient visit, almost 6 months after the initial presentation, patient continued to be in gastrointestinal as well as hematological remission with oral mesalazine 3.6 gm/day and prednisolone at a dose of 5 mg/day.
Discussion
TTP was first described by Elli Moschowitz as a disease caused due to “some powerful toxin” with agglutinative and hemolytic properties.[4] This toxin was eventually identified to be an antibody directed against ADAMTS13.[1] Extraintestinal manifestations are well known in inflammatory bowel disease, reported with frequencies ranging from 6% to 47%.[5] Hematological complications are frequently seen and may involve any hematopoietic cell line, the commonest being anemia, reported in 5% of patients with ulcerative colitis.[6] Leukocytosis and thrombocytopenia may also be seen and are usually due to immunosuppressant treatments or sulfasalazine.[6]
Thrombotic thrombocytopenic purpura is not traditionally considered an extraintestinal manifestation of ulcerative colitis. There are only two case reports described in literature, which suggest a possible association between the two.[23] These reports have described 3 patients presenting with TTP following exacerbation of ulcerative colitis. In the very first case reported by Almogy et al.,[2] the patient developed TTP after undergoing colectomy for massive gastrointestinal bleeding. She failed to respond to plasma exchanges, high dose steroids and vincristine eventually requiring splenectomy to achieve hematological remission.
Baron et al. also described two women with ulcerative colitis who developed TTP. Both the patients responded favourably to steroids and plasma exchanges, but one of them was also administered vincristine.[3] In a presentation similar to the ones described above, our patient too developed TTP following a flare of ulcerative colitis. Our patient responded favorably to plasma exchanges and steroids, and additional immunosuppressant therapy was not required.
We hypothesize that the flare may lead to intestinal mucosal inflammation and edema which increase translocation of intestinal bacteria. It is possible that the shared epitopes of intestinal organisms and ADAMTS13 trigger an autoimmune response. Similar mechanism has been postulated to lead to other classical extraintestinal manifestations reported in inflammatory bowel disease.[5]
As a differential, the possibility of drug induced thrombotic microangiopathy (DITMA) was also explored. DITMA occurs either as an acute immune mediated reaction or as a result of dose dependent toxicity, and resolves following discontinuation of the offending drug.[7] In this case, the patient had not received any drug which is known to cause DITMA. Rivaroxaban is a relatively novel drug and has not been described to be associated with TMA in the literature available so far. Also, the occurrence of TMA 2 weeks after discontinuation of the drug makes the attribution to rivaroxaban less likely.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conclusion
Most cases of thrombotic thrombocytopenic purpura are idiopathic; however, some clinical conditions, autoimmune disorders and certain drugs are known to increase the risk of TTP. Although the anecdotal case reports suggest a possible association, more research is needed to understand the potential link between ulcerative colitis and thrombotic thrombocytopenic purpura.
It must be recognized that untreated TTP follows a progressive course leading to irreversible kidney damage, neurological catastrophe and death. Introduction of therapeutic plasma exchange has had an enormous impact on altering the natural course of this illness, with reduction of TTP related mortality from 94% to 13%, which reiterates the importance of early identification and timely treatment.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Ulcerative colitis and thrombotic thrombocytopenic purpura. J Clin Gastroenterol. 2001;32:248-50.
- [Google Scholar]
- First two patients with Ulcerative colitis who developed classical thrombotic thrombocytopenic purpura successfully treated with medical therapy and plasma exchange. J Clin Apher. 2002;17:204-6.
- [Google Scholar]
- An acute febrile pleiochromic anemia with hyaline thrombosis of the terminal arterioles and capillaries. Arch Intern Med. 1925;36:89-93.
- [Google Scholar]
- Extraintestinal manifestations of inflammatory bowel disease. Inflamm Bowel Dis. 2015;21:1982-92.
- [Google Scholar]
- Extraintestinal manifestations of inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2008;46:124-33.
- [Google Scholar]
- Drug induced thrombotic microangiopathy: A systematic review of published reports. Blood. 2015;125:616-8.
- [Google Scholar]







