Translate this page into:
Time to Revisit the Use of Nontunneled Dialysis Vascular Catheters Even in Cost-Limited Setting
Address for correspondence: Dr. K. L. Gupta, Department of Nephrology, PGIMER, Sector 12, Chandigarh - 160 012, India. E-mail: klgupta@hotmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Despite the high rates of infection and mortality in the developing and underdeveloped world, nontunneled central venous catheters remain an irreplaceable tool for the majority of the end-stage renal disease (ESRD) patients at the time of initiation of hemodialysis (HD) because of their cost and convenience of insertion. We evaluated the spectrum of central venous catheter-related infections in our HD unit. The study included ESRD and acute kidney injury patients, with the diagnosis of HD catheter-related bloodstream infections (CRBSI) over a period of 2 months from August 2017 to September 2017. We aimed to study the spectrum of infection in patients with nontunneled vascular catheters in our HD center.
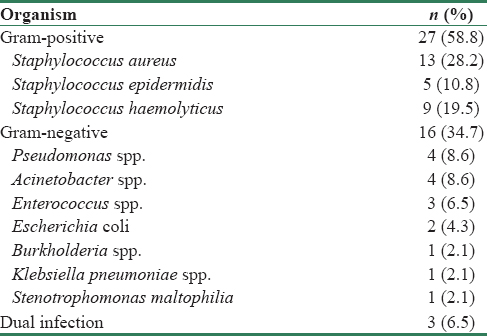
During the study period, a total of 74 (61.67%) cases of CRBSI were documented, of which 46 (62.2%) were definitive/probable[1] and 28 (37.8%) were culture-negative possible CRBSI. Gram-positive infections accounted for 58.8% of total culture-positive cases with Staphylococcus aureus being most commonly isolated organism in 13 patients (28.2% of culture-positive cases). One patient of S. aureus-related CRBSI developed tricuspid valve endocarditis and another patient of Stenotrophomonas maltophilia-related CRBSI expired due to worsening sepsis and septic shock. Apart from these two patients, rest were managed with intravenous antibiotics on an outpatient basis. Gram-negative infections accounted for 34.7% of total culture-positive cases and three patients (6.5%) had a dual infection with the simultaneous isolation of both Gram-positive and negative organism. Two patients required catheter exchange twice over 2-month period. Rest were managed with single time catheter exchange till the follow-up.Table 1 shows the microbiological spectrum of CRBSI in our HD unit.
Our study is consistent with the published literature that shows Gram-positive infections are responsible in the majority of the cases.[2] However, the high prevalence of Gram-negative infections in our study should be taken into account and empirical Gram-negative antibiotic should also be started along with Gram-positive coverage for suspected CRBSI. Another Indian study by Gupta et al.[3] showed Gram-negative infections in the majority, with Pseudomonas being the most commonly isolated organism. The data on infection rate with nontunneled catheters are limited.[4]
In the developing and underdeveloped world, the use of tunneled vascular catheters is limited by economic constraints where tunneled catheters cost approximately five times that of nontunneled catheters (15,000 and 3000 Indian rupees, respectively). However, considering the high infection rate with the use of nontunneled catheter and successive antibiotic administration, it would be prudent to use tunneled vascular catheters even in the developing world and would aptly fit the idiom “penny wise pound foolish.”
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- National Kidney Foundation KDOQI Clinical Practice Guidelines and Clinical Practice Recommendations for 2006 Updates. Hemodialysis adequacy, peritoneal dialysis adequacy and vascular access. Am J Kidney Dis. 2006;48(Suppl 1):S1-322.
- [Google Scholar]
- The spectrum of infections in catheter-dependent hemodialysis patients. Clin J Am Soc Nephrol. 2011;6:2247-52.
- [Google Scholar]
- Microbiology of non-tunnelled catheter-related infections. J Clin Diagn Res. 2016;10:DC24-8.
- [Google Scholar]
- Extranasal Staphylococcus aureus colonization predisposes to bloodstream infections in patients on hemodialysis with noncuffed internal jugular vein catheters. Hemodial Int. 2017;21:35-40.
- [Google Scholar]






