Translate this page into:
Unveiling Complexity: Nesidioblastosis in the Nexus of Diabetes and Chronic Kidney Disease
Corresponding author: Muralinath Vukkadala, Department of Nephrology, Asian Institute of Gastroenterology (AIG) (Mayo clinic care network), Hospitals, Hyderabad, Telangana, India. E-mail: dr.muralinath@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Paladugu NR, Vukkadala M, Das A, Sekaran A, Merugu C. Unveiling Complexity: Nesidioblastosis in the Nexus of Diabetes and Chronic Kidney Disease. Indian J Nephrol. 2025;35:433-4. doi: 10.25259/IJN_90_2024
Abstract
We report a rare and intricate case of nesidioblastosis, marked by hyperinsulinemic hypoglycemia, in a patient with diabetes and chronic kidney disease (CKD). PET-CT imaging and histopathology confirmed the condition, culminating in a comprehensive treatment strategy comprising subtotal pancreatectomy and pharmacotherapy. This case marks the first documented occurrence of nesidioblastosis in a patient with CKD and diabetes. The presence of CKD further complicated the clinical picture, influencing hypoglycemic risk, drug efficacy, insulin clearance, and counter-regulatory mechanisms.
Keywords
Chronic kidney disease
Diabetes mellitus
Nesidioblastosis
Subtotal pancreatectomy
Introduction
Adult nesidioblastosis is a rare disorder that causes hyperinsulinemic hypoglycemia. It is extremely rare for patients with diabetes to develop this disorder. The diagnostic challenge becomes more complex when a patient with chronic kidney disease (CKD) presents with hypoglycemia due to this rare combination.
Case Report
A 55-year-old woman with diabetes for past 15 years, hypertension, and a 1-year history of CKD with a baseline serum creatinine value of 2.3 mg/dL was admitted with altered sensorium. She had low blood glucose levels that improved with dextrose infusion. She had recurrent episodes of hypoglycemia despite treatment.
Following an infusion of 10% dextrose, a new episode of symptomatic hypoglycemia occurred. As a result, a comprehensive investigation was conducted. Labs showed glomerular filtration rate (eGFR) of 33 mL/min/1.73m2, 2+ albuminuria 2 and urine protein-creatinine ratio of 1.1 g/g. Fundus examination showed proliferative retinopathy. Additional tests [Table 1] revealed low levels of fasting glucose and elevated C-peptide levels. Anti-insulin antibody test was negative.
| Test | Patient | Reference |
|---|---|---|
| Glucose | 20 | <55 mg/dl |
| Insulin | 21.4 | >3 μIU/ml |
| C-peptide | 10 | 1.1–4.4 ng/mL |
| β-hydroxybutyrate | 0.01 | <0.4 mmol/L |
| Insulin antibodies | 1.88 | <12 U/mL |
Reference values from the Endocrine Society Clinical Practice Guidelines for the evaluation and management of adult hypoglycemic disorders.
Table 1 shows patient test results including glucose, insulin, C-peptide, β-hydroxybutyrate, and insulin antibodies levels, comparing them against reference values.
Based on the findings, the patient was diagnosed with endogenous hyperinsulinemic hypoglycemia, which could have been triggered by insulinoma or nesidioblastosis.
An endoscopic ultrasound (EUS) revealed a hypoechoic pancreatic lesion which was inconclusive. PET-CT imaging [Figure 1] showed increased Ga-68 EXENDIN tracer uptake throughout the pancreas, indicating nesidioblastosis.

- Bright red uptake shown by the Ga-68 EXENDIN tracer throughout the pancreas. The mouse pointer is at the vertebra Axial section showing bright red uptake of the contrast in Positron Emission Tomography-Computed Tomography.
The patient’s diet was modified to more frequent meals and reduced carbohydrate intake. In addition, acarbose 50 mg, octreotide 50 mcg subcutaneously twice daily, and verapamil 80 mg twice daily was prescribed. However, she still had hypoglycemic episodes.
A subtotal pancreatectomy was decided after multidisciplinary team discussion. The histopathology confirmed the presence of ductulo-insular complexes in benign pancreatic parenchyma, suggestive of nesidioblastosis [Figure 2]. After surgery, the frequency of hypoglycemia episodes decreased. Treatment initiated included acarbose (25 mg) and octreotide (50 mcg s/c OD). In addition, fineronone 10 mg OD was prescribed with regular potassium monitoring for DKD. She was discharged on octreotide s/c depot injection of 20 mg. A follow-up after 3 months revealed no further hypoglycemia episodes.
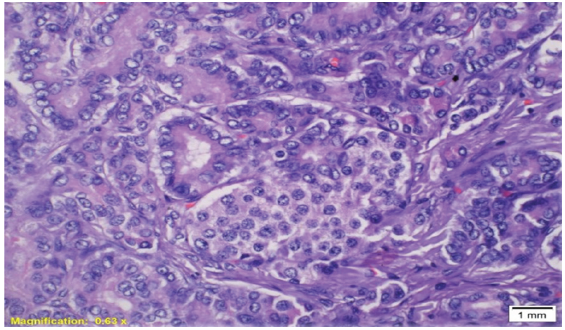
- Close proximity of ducts and islet cell cluster forming ductulo–insular complex H&E stain with 40x. H&E: Hematoxylin and Eosin.
Discussion
This is the first documented case that presents a unique intersection of adult nesidioblastosis, diabetes, and CKD. While kidneys typically aid in insulin clearance, advanced renal failure can elevate insulin levels and enhance insulin uptake. This compensatory mechanism aims to offset declining insulin degradation.
She was negative for anti-insulin antibodies, which was not done in previously reported cases.1 She had postprandial hypoglycemia, which is typical in Noninsulinoma Pancreatogenous Hypoglycemia Syndrome (NIPHS).
The use of positron emission tomography–computed tomography with Ga-68 EXENDIN, a radiolabeled analog of glucagon-like peptide-1, is an emerging technique for identifying insulin-secreting lesions.2 In this case, the pancreas showed diffuse increased Ga-68 EXENDIN tracer suggestive of Nesidioblastosis.
The treatment is customized based on severity. Approaches involve dietary adjustments, consuming smaller spaced meals, and avoiding quickly digestible carbs. Medications like diazoxide, octreotide, and acarbose may be used.
Surgical treatment usually involves resecting the insulin-secreting tumor through either enucleation or partial pancreatectomy.3 The decision regarding the extent of pancreatectomy depends on factors such as size and location of lesion, potential postoperative complications like diabetes mellitus and pancreatic fistula. In instances where diffuse nesidioblastosis is present, subtotal pancreatectomy (80–95%) is typically performed to ensure better management of hypoglycemia compared to conservative pancreatectomy.
Diagnosing adult nesidioblastosis presents unique challenges when coexisting with CKD and diabetes mellitus. The presence of CKD complicates the diagnostic process. Effective management necessitates a comprehensive, multidisciplinary approach, encompassing medical interventions, surgical procedures, or a combination.
Conflicts of interest
There are no conflicts of interest.
References
- Adult nesidioblastosis in chronic kidney disease. Case Rep Endocrinol 2019:7640384.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Localization of hidden insulinomas with 68Ga-DOTA-Exendin-4 PET/CT: A Pilot Study. J Nucl Med. 2015;56:1075-8.
- [CrossRef] [PubMed] [Google Scholar]
- Adult-onset nesidioblastosis causing hypoglycemia: An important clinical entity and continuing treatment dilemma. Arch Surg. 2001;136:656-63.
- [CrossRef] [PubMed] [Google Scholar]








