Translate this page into:
Using eGFR and Albumin Creatinine Ratio as an Initial Screening Tool in Trinidadian Primary Care to Identify High-risk Population for CKD: A Cross-Sectional Study
Corresponding author: Shivananda B. Nayak, Department of Preclinical Sciences, Faculty of Medical Sciences, The University of the West Indies, Trinidad and Tobago. E-mail: shiv25@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mahadevappa K, Nayak SB, Maharaj RG, Bhaktha G. Using eGFR and Albumin Creatinine Ratio as an Initial Screening Tool in Trinidadian Primary Care to Identify High-risk Population for CKD: A Cross-Sectional Study. Indian J Nephrol. 2024;34:332-7. doi: 10.25259/ijn_451_23
Abstract
Background:
Chronic kidney disease (CKD) is a major public health burden and is often undiagnosed in the primary care setting. Untested and untreated, this often leads to renal failure and dialysis.
Materials and Methods:
This was a cross-sectional study of adults aged 20 years and over, diagnosed with type 2 diabetes mellitus and/or hypertension, with no previous history or record of CKD, and attending three chronic disease clinics in the Eastern Regional Health Authority (ERHA). Patients were screened for risk of CKD by using the albumin creatinine ratio. The eGFR was calculated based on serum creatinine by using the CKD Epidemiology Collaboration (EPI) 2009 equation.
Results:
In total, 430 patients agreed to participate with 61.2% of response rate. Of the 385 with complete data, 357 (92%) were detected as having a high risk for CKD; older patients (>66 years) and those with both diabetes and hypertension had high proportions of risk for CKD. There were significant associations between age, systolic hypertension, and the severity of risk for CKD.
Conclusion:
CKD is common at the primary care level among adults with NCDs in Trinidad, with many patients having been left out without being tested for CKD. Primary care physicians must take this into consideration in caring for NCD patients.
Keywords
Albumin creatinine ratio (ACR)
Chronic kidney disease (CKD)
Estimated glomerular filtration rate (eGFR)
Non communicable diseases (NCDs)
Trinidad
Introduction
Among patients with non-communicable diseases (NCDs), the silent development of impaired renal function is referred to as chronic kidney disease (CKD).1 Globally, CKD has emerged as a major cause of morbidity and mortality,2,3 and at the general population level, CKD prevalence is 13.4% in stages 1–5 and 10.6% in stages 3–5.4 Among patients with hypertension, the prevalence of CKD is 46.9% in Ghana5 and 37.5% in Thailand.6 Among general practice patients in the Netherlands, the prevalence of CKD is 28% among diabetics and 21% in hypertensives.7
In the Caribbean, there have been several published reports on the prevalence of CKD. Reports have originated at the population level (Jamaica, St. Kitts),8,9 hospital level (Haiti),10 primary care level (Trinidad),11,12 and specialist diabetes clinics (Jamaica)13,14 These studies have used several methods for determining CKD, including a review of results in files,13 eGFR (estimated glomerular filtration rate) only,11,12 and eGFR and urine dipstick9,10,14 (for protein). Although current recommendations use both eGFR and albuminuria concentrations to determine CKD,15 none of these Caribbean studies have used a quantitative assessment of albuminuria. See Supplementary Table 1 for a tabular summary of these studies.
Globally and in the Caribbean region, the most common causes of CKD and ESRD are lifestyle-related NCDs.16-19 In 2011, it was reported that among countries in the English-speaking Caribbean, “Trinidad and Tobago ranks highest in the number of patients (n = 436 patients or 335/patients per million population) with ESRD receiving hemodialysis in comparison with Jamaica (n = 366), Bahamas (n = 211), Barbados (n = 185), Cayman Islands (n = 41), and the British Virgin Islands (n = 27).”17 Currently, in Trinidad and Tobago, the state provides a monthly grant of $5000.00 (TT$) to support patients whose dialysis needs cannot be met in the public healthcare system.20
Using eGFR and albumin creatinine ratio (ACR) as an initial screening tool in the targeted population at the primary care level is useful in determining the associated factors at the local community level as well as in understanding the burden on the healthcare system. This, in turn, would be useful in creating appropriate policies and strategies to identify, prevent, and reduce the burden of CKD.21 Our objective was to determine high-risk populations at the primary care level who may need further assessment to diagnose CKD by using a combination of eGFR (calculated by the CKD EPI 2009 equation) and quantitative assessment of albuminuria and to determine the factors predisposing to CKD among this population.
In our study, we identified the populations who are at risk of CKD and who may have gone unnoticed without any further monitoring or tests for diagnosis of CKD in primary care practice. In our clinical practice, we use eGFR and albuminuria as initial screening tools in identifying high-risk populations for CKD.
Materials and Methods
This was a cross-sectional study. The Eastern Regional Health Authority (ERHA) in Trinidad has two counties: St. Andrew/St. David’s (STAD) and Nariva/Mayaro (NAMA). The total adult population (>20 years) within these counties in 2011 was 76,974.22 STAD has seven and NAMA has five primary health centers, respectively. The study was conducted at the three major health centers in these counties, located in Sangre Grande, Rio Claro, and Mayaro. The patients attending chronic disease clinics (CDCs) at these centers need to be registered with an appointment date and are usually followed up every 3–4 months. The study was approved by the Campus Ethics Committee, The University of the West Indies, number CEC009/09/16.
Every day of the study, 30 patients were randomly selected from those registered to attend. The first 10 of these, who fulfilled the inclusion and exclusion criteria and signed the consent form were enrolled. The study was conducted from January 3, 2017 to April 28, 2017.
We included patients who already had a diagnosis of hypertension or type 2 diabetes, and were on prescribed medication for the same. Patients were excluded if they had previously known kidney diseases (CKD, SLE and polycystic kidney, renal calculi); benign prostatic hypertrophy; a family history of kidney disease; known malignant disease; known inflammatory arthritis; known cardiovascular diseases such as ischemic heart disease (IHD); those who were on treatment with statins, beta blockers, and nitrates (all three medications together); congestive cardiac failure; coronary artery stent placement; status post CABG; who had an angiogram done in last 6 months; those who were pregnant; those who were on non-steroidal anti-inflammatory drug (NSAIDs) for 1 week or more prior to enrollment; any acute illness; and persons younger than 20 years.
A meeting was held before the initiation of the study with the medical (phlebotomists, nurses, nursing assistants, and PCPs) and clerical staff the ERHA laboratory personnel to inform and identify any of the challenges involved in the study. All patients attending the CDC were triaged routinely by the nurse. During triaging the blood pressure, random blood sugar, urine dipstick, and weight and height (BMI) of all the patients were recorded.
The co-investigator, KM, provided the physician consultation service for the randomly selected patients. During consultation, the study was described and informed consent was obtained from the patients who were willing to participate. Once the consent was obtained, the details from the patient medical record were extracted. These included demographics (age, sex, ethnicity (self-declared)), current lifestyle (smoking in pack years, an interviewer-administered Cut, Annoyed, Guilty, and Eye (CAGE) questionnaire for patients who drink alcohol), BMI, average systolic pressure and diastolic pressure readings from the last three visits (which includes the current visit), medication use (angiotensin receptor blocker (ARB), angiotensin-converting enzyme (ACE) inhibitor, statins, and NSAIDs), and past medical history. Then, the laboratory tests, namely serum creatinine, haemoglobinA1c (HbA1c), urine microalbumin, and urine albumin creatinine ratio (UACR), were requested.
All the study participants were given 8-am appointments to return for laboratory testing. They were instructed to fast overnight for about 10–12 hours and to avoid heavy exercise on the day of the test. Female patients were advised to postpone their appointment if they were menstruating. On the day of the appointment, the phlebotomist drew the venous blood sample, and a random spot morning urine sample was collected in an empty sterile cup by using the clean catch technique. All samples were transported at 2°C–8°C to the Sangre Grande Hospital (SGH) laboratory and processed on the same day. Patients who had a urine dipstick test result positive for blood or albumin during the visit were further tested for urine microscopy, culture, and sensitivity analysis.
Serum creatinine and UACR was determined using Mindray BS800 by the modified kinetic Jaffé method with an autoanalyzer.23 HbA1c was determined using Mindray BS800. Urine microalbumin was determined using the immunometric method, and a value of >20 mg/dL was considered positive as per the ERHA laboratory reference range. The eGFR was calculated for each patient using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) 2009 equation.24
Statistical analysis
All the patients were stratified into different stages of CKD based on the classification proposed by Kidney Disease: Improving Global Outcomes (KDIGO) clinical practice guidelines for CKD.15 In addition to descriptive statistics, chi-square analysis was carried out to test the associations between factors and severity of CKD adverse outcomes. The analyses are performed using the IBM SPSS statistical software package.
Results
A total of 2516 patients with either diabetes or hypertension or both attended CDCs during this study period from January 3, 2017 to April 28, 2017. A random sample of 703 patients who fit the inclusion and exclusion criteria attending CDCs at the primary health centers was approached. From these, 430 patients agreed to participate (61.2%) and were enrolled. Thirty-seven patients were lost due to dropout, leaked samples, or lost reports. Out of 393 patients with lab reports, eight patients were excluded as they had urinary tract infections (UTIs) confirmed by urine culture and sensitivity testing. Therefore, the total sample finally analyzed was 385.
The majority (64.1%) were more than 56 years old. Most were female (71.4%) and East Indian (64%). Furthermore, 80.5% were overweight or obese, and 53% had both hypertension and diabetes. Approximately 60% of the patients were prescribed an ACE inhibitor or ARB, and 58% were on statins. The youngest participant with CKD was aged 25 years. About one-tenth of the HbA1cs done showed very poor control, with levels over 9%; 24% had systolic BP > 160 mmHg [Table 1].
| Variable | N (%) | Moderate risk N (%) | High risk N (%) | Very high risk N (%) | p value |
|---|---|---|---|---|---|
| Age | 357 (100) | 0.001 | |||
| <55 years | 128 (35.8) | 33 (9.2) | 89 (24.9) | 6 (1.7) | |
| 56-65 years | 131 (36.6) | 38 (10.6) | 84 (23.5) | 9 (2.5) | |
| 66 years or greater | 98 (27.5) | 12 (3.4) | 65 (8.2) | 21 (5.9) | |
| Gender | 357 (100) | 0.573 | |||
| Female | 255 (71.4) | 60 (16.8) | 172 (48.2) | 23 (6.4) | |
| Male | 102 (28.5) | 23 (6.4) | 66 (18.5) | 13 (3.6) | |
| Ethnicity | 357 (100) | 0.143 | |||
| African | 84 (23.5) | 18 (5) | 60 (16.8) | 6 (1.7) | |
| East Indian | 229 (64) | 51 (14.3) | 149 (41.7) | 29 (8.1) | |
| Mixed ethnicity | 44 (12.3) | 14 (3.9) | 29 (8.1) | 1 (0.3) | |
| BMI | (n = 355) | ||||
| ≤24.9 | (n = 69) 19.5% | (10) 2.8% | (51) 14.4% | (8) 2.3% | 0.082 |
| 25–29.9 | (n = 133) 37.5% | (28) 7.9% | (88) 24.8% | (17) 4.8% | |
| ≥30 | (n = 153) 43% | (44) 12.4% | (99) 27.9% | (10) 2.8% | |
| Alcohol CAGE | (n = 348) | **** | |||
| 0–1 | (n = 339) 97% | (80) 23% | (226) 64.9% | (33) 9.5% | |
| 2–4 | (n = 9) 3% | 0 | (8) 2.3% | (1) 0.3% | |
| Smoking | (n = 34) | **** | |||
| 0.1–10 | (n = 18) 53% | (3) 8.8% | (14) 41.2% | (1) 2.9% | |
| >10.1 | (n = 16) 47% | (1) 2.9% | (14) 41.2% | (1) 2.9% | |
| Systolic BP | (n = 357) | 0.043 | |||
| ≤139 | (n = 152) 42.6% | (34) 9.5% | (108) 30.3% | (10) 2.8% | |
| 140–159 | (n = 119) 33.3% | (29) 8.1% | (80) 22.4% | (10) 2.8% | |
| ≥160 | (n = 86) 24.1% | (20) 5.6% | (50) 14% | (16) 4.5% | |
| Diastolic BP | (n = 357) | 0.715 | |||
| ≤89 | (n = 274) 76.8% | (65) 18.2% | (182) 51% | (27) 7.6% | |
| 90–99 | (n = 61) 17% | (13) 3.6% | (43) 12% | (5) 1.4% | |
| ≥100 | (n = 22) 6.1% | (5) 1.4% | (13) 3.6% | (4) 1.1% | |
| DM and HTN | (n = 357) | 0.219 | |||
| DM | (n = 43) 12.1% | (10) 2.8% | (32) 9% | (1) 0.3% | |
| HTN | (n = 123) 34.5% | (25) 7% | (87) 24.4% | (11) 3.1% | |
| Both DM and HTN | (n = 191) 53.4% | (48) 13.4% | (119) 33.3% | (24) 6.7% | |
| Investigations | |||||
| HbA1c | (n = 270) | 0.768 | |||
| ≤6 | (n = 169) 62.5% | (33) 12.2% | (120) 44.4% | (16) 5.9% | |
| 6.1–9 | (n = 71) 26.4% | (18) 6.7% | (45) 16.7% | (8) 3% | |
| ≥9.1 | (n = 30) 11.1% | (7) 2.6% | (19) 7% | (4) 1.5% |
****Several cells with too few numbers for analysis. GFR: Glomerular filtration rate; CKD-EPI: Chronic Kidney Disease Epidemiology Collaboration; BMI: Body mass index; BP: Blood pressure; DM: Diabetes mellitus; HTN: Hypertension; HbA1c: Glycated hemoglobin; CAGE: Cut, Annoyed, Guilty, and Eye.
Around 8% of participants fell into the category of G1A1 and G2A1 (normal to mildly decreased eGFR and albuminuria) based on eGFR and ACR. Furthermore, 357 (92%) patients were detected as having CKD; 20.8% of participants were at moderate risk (G1 or G2 and A2), 61.8% at high risk (G1 or G2 and A3 or G3a and A2), and 9.3% at a very high-risk (G3a and A3 or G3b or G4 and A2 or A3) of having an adverse outcome related to their CKD [Table 2].
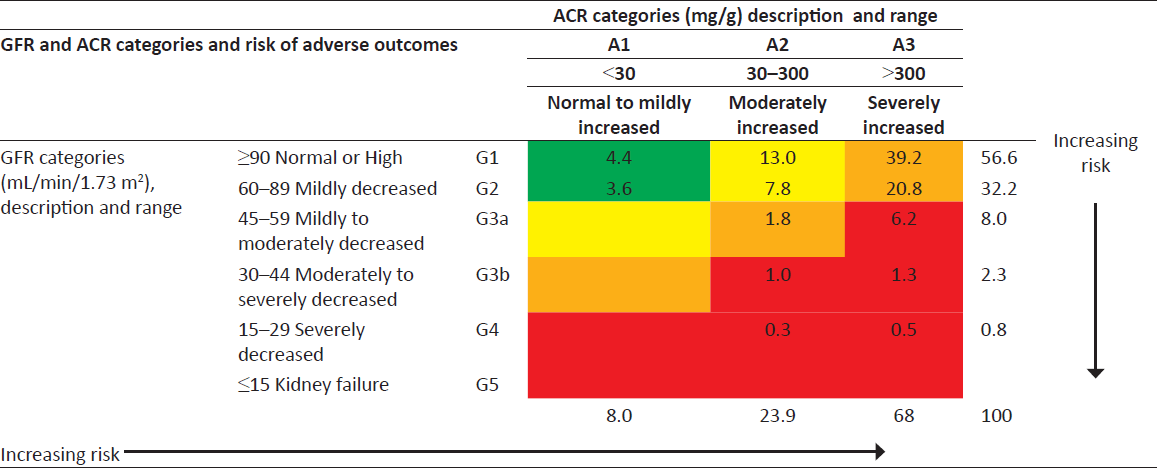
ACR: albumin creatinine ratio; CKD: chronic kidney disease; GFR: glomerular filtration rate. Green: Normal eGFR and ACR (if no other markers of kidney disease, no CKD). Yellow: Moderately increased risk of complications of CKD. Orange: High risk of complications of CKD.
Red: Very high risk of complications of CKD.
Test of association
There was a significant association between age and severity of adverse outcomes of risk of CKD. Although a high percentage of older adults >66 years had a high risk of CKD, it was noticed that the participants in the age group of <55 years and between 55 to 65 years were in high percentage with risk of CKD of moderate to high risk of adverse outcomes. There was no association noted between the severity of risk of CKD and other factors such as smoking, BMI, and HbA1c [Table 1].
Discussion
This study estimated that the risk of undiagnosed CKD among patients with NCD at the primary care level is 92%. There was a significant association between age and severity of adverse outcomes of risk of CKD. With an increase in age, there was a greater prevalence of moderate and severe stages of risk of CKD. A high percentage of older adults >66 years were in the very-high-risk category for CKD. The gender-based analysis did not show any significant difference between different categories within gender. The proportion of males was higher when compared to females with risk of CKD, but in the category of risk of CKD with moderate to high risk, females were in a higher proportion than males. Ethnicity was not significantly associated with the severity of risk of CKD. The risk of CKD with very-high-risk adverse outcomes was slightly higher in the East Indian population than in African or Mixed populations.
There was a significant association between systolic blood pressure and the risk for severity of CKD. An increase in systolic blood pressure may also adversely affect the rate of progression of CKD. However, there was no significant association noted with diastolic blood pressure. Patients who had both type 2 diabetes and hypertension were in a high proportion in the category of very-high-risk adverse outcomes of CKD. Patients who had either type 2 diabetes or hypertension were in high percentage in the category of moderate to high-risk adverse outcomes of CKD. There was a significant negative correlation between BMI and the severity of risk of CKD.
In this study, we targeted the undiagnosed high-risk population with diabetes mellitus and/or hypertension to stress the importance of screening in this high-risk population for further evaluation to diagnose undetected CKD at the primary care level.
The findings in this study emphasize that the ACR should be used as a screening tool by PCPs in addition to measuring e-GFR for identifying the high-risk population who need further monitoring to unmask the hidden diagnosis of CKD in the high-risk population.
Due to the limitations in logistics, the renal function test and ACR were done only once. We acknowledge that just conducting these only once, CKD cannot be diagnosed or confirmed. To diagnose CKD, these tests should be repeated at 3 months, and a persistent decline in eGFR with albuminuria or only albuminuria will help in confirming a diagnosis of CKD. Our main aim was to draw the attention of PCPs in their practice to further test and monitor these high-risk populations with diabetes mellitus and/or hypertension for identifying CKD in their clinical practice.
This study was conducted in 2017 but it is relevant even at present as NCDs such as diabetes and hypertension are still highly prevalent in our communities.
The KDIGO guidelines make the point that the diagnosis of CKD is based on both the GFR and albuminuria,15 and this current paper addressed this gap. A previous study in Trinidad estimated a prevalence rate of about 36% for different stages of CKD among NCD patients.11 In that study, patients were classified into different stages based only on eGFR of <89 mL/min/1.73 m2. The UACR was not considered.11 Ezenwaka et al.11 included patients with heart disease but did not exclude patients who were already diagnosed with CKD, whereas in our study, we excluded patients with heart disease and patients who were already diagnosed with CKD. Similarly, another previous study conducted in the ERHA in Trinidad using eGFR only concluded that the prevalence of CKD was 53.7%.12 In the present study, if eGFR alone is used, the prevalence of CKD is 43.3%.
This study for the first time in the Caribbean used a quantitative assessment of albuminuria by using ACR to diagnose the variety of stages of CKD. The high prevalence of NCDs such as diabetes and hypertension in the Caribbean necessitates careful screening of CKD in high-risk individuals.
There are several limitations of this study. First, in conducting the survey, endpoints were measured only once. This raises the possibility of false-positive and false-negative errors. This survey was limited only to one regional health authority; therefore, it cannot be generalized to the entire country. Poor documentation in medical records may have resulted in the alteration of inclusion and exclusion criteria. There is no local validation of the CKD-EPI Creatinine (2009) equation.25 The serum creatinine measured in ERHA is not Isotope Dilution Mass Spectrometry (IDMS)-standardized; it is known that standardized measurement of serum creatinine values may differ by 5%–20% when compared to non-standardized values.26 This study did not consider the duration of hypertension or diabetes disease in the study participants.
Conclusion
CKD as determined using eGFR and ACR is very common among patients with NCDs in Trinidad. This study recommends that estimated GFR should be reported directly from laboratories whenever serum creatinine is requested. Screening for CKD by using eGFR and UACR of all patients with diabetes and hypertension should be done at CDCs in health centers. These should be repeated after the initial screening.
Acknowledgements
The authors would like to thank the patients and staff of the ERHA who facilitated this project. This project was carried out in partial fulfillment of KM’s Doctor of Medicine (DM) in Family Medicine degree.
Availability of data and materials
The data set and survey instrument are available on reasonable request from the first author, KM.
Financial support and sponsorship
Funding for this study was received from the Campus Research and Publications Grant of The University of the West Indies, St. Augustine: CRP.3.NOV16.28.
Conflicts of interest
There are no conflicts of interest.
References
- Prevalence of chronic kidney disease in population-based studies: Systematic review. BMC Public Health. 2008;8:117.
- [CrossRef] [PubMed] [Google Scholar]
- Prevention, detection and management of early chronic kidney disease: A systematic review of clinical practice guidelines. Nephrology (Carlton). 2013;18:592-604.
- [CrossRef] [PubMed] [Google Scholar]
- Barriers to the successful practice of chronic kidney diseases at the primary health care level; a systematic review. J Renal Inj Prev. 2014;3:61-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Global prevalence of chronic kidney disease – A systematic review and meta-analysis. PLoS One. 2016;11:e0158765.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prevalence of chronic kidney disease in hypertensive patients in Ghana. Ren Fail. 2011;33:388-92.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of chronic kidney disease associated with cardiac and vascular complications in hypertensive patients: A multicenter, nation-wide study in Thailand. BMC Nephrol. 2017;18:115.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Chronic kidney disease in patients with diabetes mellitus type 2 or hypertension in general practice. Br J Gen Pract. 2010;60:884-90.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A survey of chronic renal failure in Jamaica. West Indian Med J. 2004;53:81-4.
- [PubMed] [Google Scholar]
- Chronic kidney disease and risk factor prevalence in Saint Kitts and Nevis: A cross-sectional study. BMC Nephrol. 2017;18:7.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and risk factors for chronic kidney disease in a rural region of Haiti. Swiss Med Wkly. 2014;144:w14067.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of chronic kidney disease using estimated glomerular filtration rate in Caribbean patients with non-communicable diseases. J Dis Glob Health. 2016;7:40-6.
- [Google Scholar]
- Screening for chronic kidney disease in a small developing country using the National Kidney Foundation Guidelines. Int J Chronic Dis Ther. 2016;2:39-41.
- [Google Scholar]
- Prevalence of chronic renal failure in the diabetic population at the University Hospital of the West Indies. West Indian Med J. 2004;53:85-8.
- [PubMed] [Google Scholar]
- Prevalence of chronic kidney disease among patients attending a specialist diabetes clinic in Jamaica. West Indian Med J. 2015;64:201-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Clinical practice guidelines for management of chronic kidney disease. Kidney Int 2012(Suppl 3):1-150.
- [Google Scholar]
- Report from the Caribbean renal registry, 2006. West Indian Med J. 2007;56:355-63.
- [PubMed] [Google Scholar]
- The epidemiology of end stage renal disease at a centre in Trinidad. West Indian Med J. 2011;60:553-6.
- [PubMed] [Google Scholar]
- Prevalence of self-reported diabetes, hypertension and heart disease in individuals seeking State funding in Trinidad and Tobago, West Indies. J Epidemiol Glob Health. 2013;3:95-103.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Chronic kidney disease in the Caribbean. West Indian Med J. 2011;60:464-70.
- [PubMed] [Google Scholar]
- Is it time to replace 24-hour urinary albumin excretion (UAE) assessment in Trinidad and Tobago? Caribb Med J. 2012;74:5-7.
- [Google Scholar]
- Methodology used in studies reporting chronic kidney disease prevalence: A systematic literature review. Nephrol Dial Transplant. 2015;30(Suppl 4):iv6-16.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- 2011. Population And Housing Census Demographic Report. Available from: https://wwwguardiancott/sites/default/files/story/2011_DemographicReportpdf [Last accessed on 2018 Aug 19]
- Available from: http://www.mindray.com/en/product/BS-800.html [Last accessed on 2018 Aug 19]
- 2016. CKD-EPI Creatinine Equation. 2021. Available from: https://www.kidney.org/content/ckd-epi-creatinine-equation-2009 [Last accessed on 2023 Oct 01]
- The impact of CKD identification in large countries: The burden of illness. Nephrol Dial Transplant. 2012;27(Suppl 3):iii32-8.
- [CrossRef] [PubMed] [Google Scholar]
- Spot urine estimations are equivalent to 24-hour urine assessments of urine protein excretion for predicting clinical outcomes. Int J Nephrol. 2015;2015:156484.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]







