Translate this page into:
A 2-year follow-up study of patients on automated peritoneal dialysis
Address for correspondence: Dr. R. Ram, Department of Nephrology, Sri Venkateswara Institute of Medical Sciences, Tirupati, Andhra Pradesh, India. E-mail: ram_5_1999@yahoo.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Automated peritoneal dialysis (APD) is increasingly being used for the treatment of end stage renal disease. We present our experience of APD at a government run tertiary care institute. APD was initiated for 22 patients between 2002 and 2010. On comparing APD and continuous ambulatory peritoneal dialysis (CAPD) patients, no difference in patient survival and technique survival was observed. CAPD patients had higher number of peritonitis episodes, greater decline in the serum albumin and a greater number of patients failed to achieve adequacy targets compared to APD.
Keywords
Adequacy
automated peritoneal dialysis
continuous ambulatory peritoneal dialysis
high transporter status
peritonitis
Introduction
Automated peritoneal dialysis (APD) is increasingly being used for the treatment of end stage renal disease. APD has potential disadvantages compared with continuous ambulatory peritoneal dialysis (CAPD) such as possible faster decline in residual renal function,[1–3] less sodium removal,[3–6] and higher peritoneal protein loss.[6] Better overall and technique survival on APD was reported in two studies.[78] However, other studies could not demonstrate a benefit for APD in terms of survival.[59] No significant differences in survival were found in three randomized controlled trials comparing APD to CAPD.[10–12] However, the largest study comprised only 50 patients.[11] In addition, APD is more expensive than CAPD[13] and that was the reason for only a few institutes in India to be able to regularly practice APD. We present our experience of APD in this paper.
Materials and Methods
This study was performed at a state government run tertiary care institute. CAPD was started at this institute in 1998. APD was started in 2002.
For all CAPD patients, the peritoneal equilibration test (PET) was performed between 1st month and 3rd month after initiation of peritoneal dialysis (PD). It was the standard PET performed according to the procedure described by Twardowski.[14] Patients with high and high average transport status were explained about APD. Patients who could afford the expenses of APD were changed to APD. For every patient initiated on APD, a well-matched CAPD patient was considered for the cohort. The patients of both groups were matched in age, gender, etiology of end stage renal disease (ESRD), residual urine volume at the time of initiation of dialysis, duration of chronic renal failure before initiation of dialysis, and peritoneal transporter status and education.
Patients of both cohorts were trained by the same PD nurse. APD patients used APD cycler (Home Choice) of Baxter India Pvt. Ltd, New Delhi. They were prescribed 2 night exchanges of 5.0 l bags of either 1.5% or 2.5% dextrose Dianeal solution as per the clinical condition. CAPD patients were prescribed three exchanges per day of 2.0 l bags of 1.5% or 2.5% dextrose Dianeal solution. A fourth exchange was added only when the patient failed to achieve adequacy and/or edema Free State. Icodextrin was not used in either group.
The patients were monitored at monthly intervals in the CAPD unit. At monthly consultations, patients were monitored with biochemical parameters, residual renal function, blood pressure, and the number of anti-hypertensive used, need of day time exchange in APD patients and additional exchange(s) in CAPD patients, infectious and mechanical complications and uremic complications.
Adequacy of PD was examined after 1st month and later after every 6 months. The International Society of Peritoneal Dialysis guidelines of 2006 were followed.[15] For small solute removal, it was recommended that the total (renal and peritoneal) weekly Kt/V urea should be greater than 1.7. For patients on APD, the recommendation was a weekly minimum clearance of 45 l/1.73 M2 should be reached.
The primary end point was patients completing 2 years follow-up or discontinuation of PD due to a complication. “As per protocol” analysis was performed and the patients who dropped due to complication were not considered for final analysis.
Clinical and biochemical data were evaluated statistically using the Student’s t-test or Chi-square test for paired or unpaired data as appropriate. P < 0.05 was considered significant. Graph Pad program, version 3 software was used.
Results
Between 2002 and 2010, APD was initiated for 22 patients. The demographic and clinical characteristics of patients at the initiation of APD were given in Table 1. APD was started after 88 ± 12 days of CAPD. There was no difference in mean age of patients, gender distribution, etiology of ESRD, urine volume, transporter status, blood pressure control, serum creatinine, and albumin between APD and CAPD cohorts.

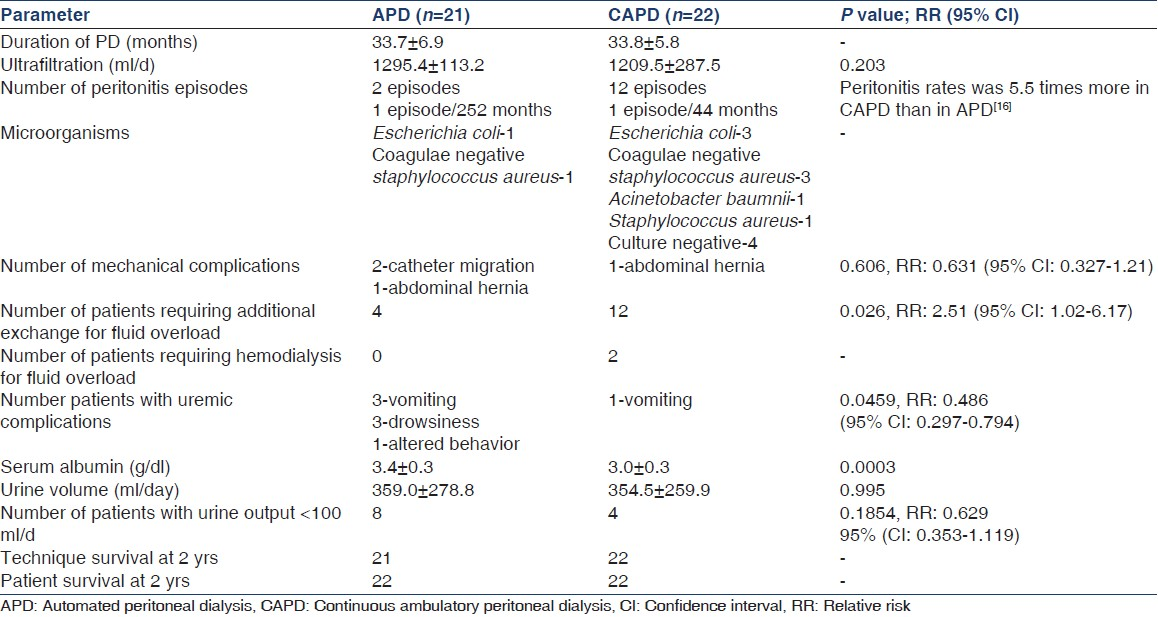
All 22 patients of CAPD group reached the end point of completion of 2 years of PD. The follow-up duration was 528 patient-months in CAPD group. In APD cohort, 1 patient was shifted to hemodialysis for the indication of altered behavior. He was shifted during 4th month of APD (see below). The duration of follow-up of APD cohort was 508 patient months. Peritonitis rate was 5.5 times more in CAPD than in APD. Significant number of patients in CAPD cohort required an additional exchange to maintain edema free condition. There was also a greater requirement of hemodialysis in CAPD patients to maintain edema free condition. There were six patients with uremic complications in APD group. Incessant vomiting was complained in three patients. The serum creatinine in these three was 6.8 ± 0.49 mg/dl, but serum sodium was high. There were another three patients with complaints of excessive drowsiness. They were also found to have hypernatremia. The serum sodium in these six patients was 149 ± 3.6 mEq/l. There was an improvement in serum albumin in APD patients after 2 years. However, it did not attain significance. However, owing to decline in serum albumin in CAPD patients, the difference of serum albumin at 2 years attained significance between the 2 groups. Characteristics of patients at the end of 2 years were given in Table 2.
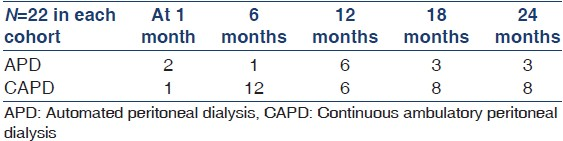
Adequacy
Adequacy of PD was examined at 6 month interval after 1st month. Patients who could not achieve the targets of weekly minimum clearance of 45 l/1.73 m2 for APD patients and total (renal and peritoneal) weekly Kt/V urea greater than 1.7 for CAPD patients was given in the Table 3. CAPD patients who could not achieve adequacy and/or maintain edema Free State with three exchanges an additional exchange was given. During 4th month of APD treatment, a patient developed altered behavior. He was shifted to hemodialysis. His weekly clearance was 35 l/1.73 M2 at 3rd month of APD. Other investigations were (mean ± SD of four values before the start of hemodialysis): Serum creatinine: 9.1 ± 0.3 mg/dl, blood urea: 210 ± 15 mg/dl, serum sodium: 131 ± 1.0 mEq/l, serum potassium: 4.3 ± 0.1 mEq/l, magnetic resonance imaging brain revealed only age related atrophy. He improved after three sessions of hemodialysis.
Discussion
This article presented 2 years follow-up of 22 incident patients on APD. APD patients were compared to well-matched CAPD patients. Limitation of the study was that patients on APD were economically stronger and could afford the treatment. It is possible that better economic status might have led to better hygienic practices, diet, and results in APD group.
A systematic review of controlled trials comparing APD and CAPD and studies of four databases had been recently published and the results of these studies were tabulated in Table 4.
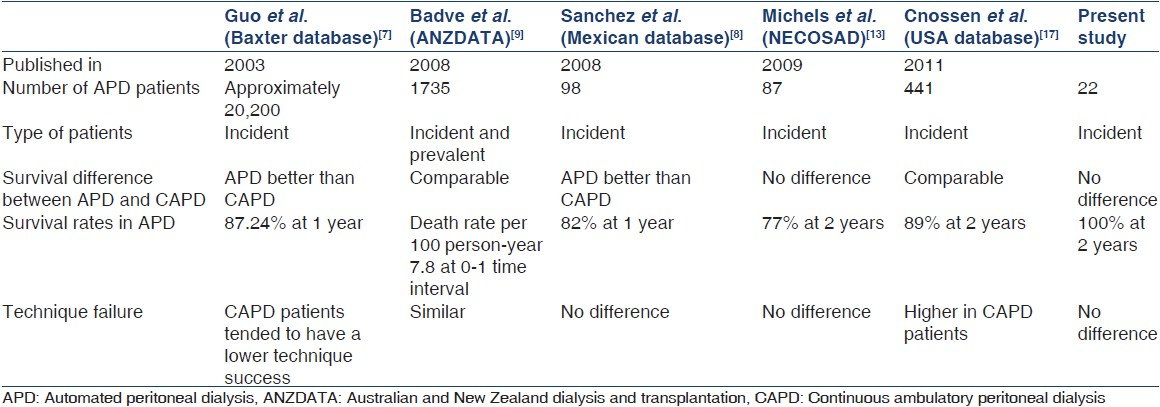
The systematic review of controlled trials,[18] and the survival data observed in the Netherlands Cooperative Study on the Adequacy of Dialysis (NECOSAD) database,[13] the Australian and New Zealand Dialysis and Transplantation (ANZDATA) registry,[9] and the USA database did not show a difference in patient survival between APD and CAPD. In the present study, survival in incident patients was comparable for APD and CAPD. in contrast, survival was better in incident APD patients in a Mexican database.[8] In a large cohort of more than 30,000 incident patients in the USA Baxter database,[7] mortality during the first 6 months of therapy was lower in APD compared to CAPD patients, although survival differences were restricted to this time period.
There was no difference in the technique survival between APD and CAPD patients in the present study, even though, the factors that contribute to technique failure such as the peritonitis and fluid overload were significantly higher in CAPD group. All episodes of peritonitis were successfully treated and patients of fluid overload were successfully managed. It is interesting that differences in technique failure between APD and CAPD were apparent only in the USA studies.[717] the results of the ANZDATA[9] and NECOSAD [13] results were different [Table 4].
Peritonitis rates, which could be an important cause of technique failure, had been differently reported in various studies; higher in CAPD,[19] and lower in APD.[2021] In a systematic review of three randomized studies, it was shown that APD patients had significantly lower peritonitis rates.[18] There was no difference in rates of peritonitis in USA data base.[17] In a recent study the outcomes of peritonitis in APD and CAPD was not reported to be different.[22]
In our study, peritonitis rates were higher in CAPD patients than in APD, but the Tenckhoff catheter was not removed any of the patients.
In the present study, serum albumin levels improved significantly in APD patients than in CAPD patients. More episodes of peritonitis and frequent fluid overload states might explain the low serum albumin levels in CAPD. In USA data base study[17] also the time-averaged albumin levels were lower in CAPD patients. A recent study suggested that peritoneal albumin loss might even be somewhat higher in APD compared to CAPD patients,[6] although no differences in protein loss or serum albumin levels were observed when patients were changed from CAPD to APD.[23]
A faster decline in urine volume per day was observed in APD compared to CAPD patients in the past.[23] The reason for the faster decline in urine volume per day in APD patients might be the more intensive ultrafiltration during shorter dwell times in APD compared to the more gradual fluid removal during CAPD.[2] In our study, the urine volume was comparable between the cohorts at the end of 2 years. However, in more number of APD patients urine volume declined to less than 100 mL/day than CAPD patients. However, it did not attain statistical significance. This happened despite more number of peritonitis episodes in CAPD group. Similar to our study the study of the USA data base[17] also found no difference in urine volume per day between APD and CAPD patients. The other data bases were silent on urine volumes.
More number of CAPD patients compared to APD could not achieve dialysis adequacy targets. The reasons could be the high average transport status and there were higher peritonitis rate in CAPD patients. These patients required additional exchanges to achieve the targets.
In conclusion, the present study compared APD and CAPD patients. The study should be read with a caveat that the APD patients were economically stronger than CAPD patients. There was no difference in the patient survival and technique survival between the two groups. CAPD patients had a higher number of peritonitis episodes, greater decline in the serum albumin and a greater number of patients failed to achieve adequacy targets compared to APD.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Rapid decline of residual renal function in patients on automated peritoneal dialysis. Perit Dial Int. 1996;16:307-15.
- [Google Scholar]
- The influence of automated peritoneal dialysis on the decrease in residual renal function. Nephrol Dial Transplant. 1999;14:1224-8.
- [Google Scholar]
- Sodium removal in patients undergoing CAPD and automated peritoneal dialysis. Perit Dial Int. 2002;22:705-13.
- [Google Scholar]
- Peritoneal sodium mass removal in continuous ambulatory peritoneal dialysis and automated peritoneal dialysis: Influence on blood pressure control. Am J Nephrol. 2001;21:189-93.
- [Google Scholar]
- Compared time profiles of ultrafiltration, sodium removal, and renal function in incident CAPD and automated peritoneal dialysis patients. Am J Kidney Dis. 2004;44:132-45.
- [Google Scholar]
- Dietary protein requirements and dialysate protein losses in chronic peritoneal dialysis patients. Perit Dial Int. 2007;27:192-5.
- [Google Scholar]
- Patient and technique survival on peritoneal dialysis in the United States: Evaluation in large incident cohorts. Kidney Int Suppl. 2003;64:S3-12.
- [Google Scholar]
- Improved patient/technique survival and peritonitis rates in patients treated with automated peritoneal dialysis when compared to continuous ambulatory peritoneal dialysis in a Mexican PD center. Kidney Int Suppl. 2008;73:S76-80.
- [Google Scholar]
- Automated and continuous ambulatory peritoneal dialysis have similar outcomes. Kidney Int. 2008;73:480-8.
- [Google Scholar]
- A prospective, randomized multicenter study comparing APD and CAPD treatment. Perit Dial Int. 1999;19:526-33.
- [Google Scholar]
- Clinical efficacy and morbidity associated with continuous cyclic compared with continuous ambulatory peritoneal dialysis. Ann Intern Med. 1994;120:264-71.
- [Google Scholar]
- Comparative evaluation of CAPD and PD-plus effectiveness. EDTNA ERCA J. 1999;25:27-9.
- [Google Scholar]
- Similar survival on automated peritoneal dialysis and continuous ambulatory peritoneal dialysis in a large prospective cohort. Clin J Am Soc Nephrol. 2009;4:943-9.
- [Google Scholar]
- Guideline on targets for solute and fluid removal in adult patients on chronic peritoneal dialysis. Perit Dial Int. 2006;26:520-2.
- [Google Scholar]
- Occurrence of peritonitis in APD versus CAPD: Methodologic problems. Nephrol Dial Transplant. 2008;23:1769-70.
- [Google Scholar]
- Comparison of outcomes on continuous ambulatory peritoneal dialysis versus automated peritoneal dialysis: Results from a USA database. Perit Dial Int. 2011;31:679-84.
- [Google Scholar]
- Automated vs continuous ambulatory peritoneal dialysis: A systematic review of randomized controlled trials. Nephrol Dial Transplant. 2007;22:2991-8.
- [Google Scholar]
- A comparative analysis on the incidence of peritonitis and exit-site infection in CAPD and automated peritoneal dialysis. Perit Dial Int. 1999;19:253-8.
- [Google Scholar]
- Continuous cycling peritoneal dialysis is associated with lower rates of catheter infections than continuous ambulatory peritoneal dialysis. Am J Kidney Dis. 1990;16:133-6.
- [Google Scholar]
- Comparison of infectious complications in peritoneal dialysis patients using either a twin-bag system or automated peritoneal dialysis. Nephrol Dial Transplant. 2001;16:604-7.
- [Google Scholar]
- Similar peritonitis outcome in CAPD and APD patients with dialysis modality continuation during peritonitis. Perit Dial Int. 2011;31:39-47.
- [Google Scholar]
- Automated peritoneal dialysis: A Spanish multicentre study. Nephrol Dial Transplant. 1998;13:2335-40.
- [Google Scholar]







