Translate this page into:
A comparative study of the effect of icodextrin based peritoneal dialysis and hemodialysis on lipid metabolism
Address for correspondence: Dr. Ali Kemal Kadiroğlu, Department of Nephrology, Medicine Faculty in Dicle University, Diyarbakir, Turkey. E-mail: akkadiroglu63@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
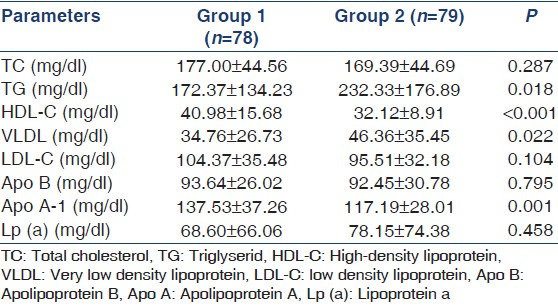
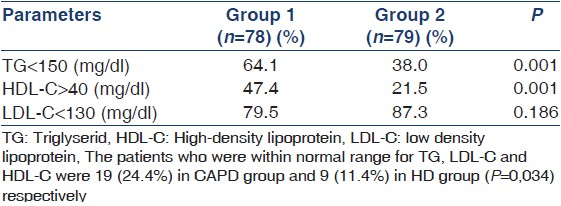
Dyslipidemia is frequent in patients with end stage renal disease. Excessive peritoneal glucose absorption from high glucose-containing peritoneal dialysis solutions may enhance disturbances on the lipid metabolism of patients on peritoneal dialysis. We compared the effect of icodextrin-based peritoneal dialysis therapy with hemodialysis (HD) therapy on lipid metabolism. A total of 157 non-diabetic patients on dialysis at least for 3 months; 78 patients on Icodextrin-based continuous ambulatory peritoneal dialysis (CAPD) (44 M, 34 F) and 79 patients in HD group (47M, 32F) were included into the study. After 12 h of fasting and before the dialysis session, serum urea, creatinin, glucose, Sodium, potasium, and albumin, total cholesterol (TC), triglycerides (TG), very low density lipoprotein (VLDL), low density lipoprotein (LDL)-C, high-density lipoprotein (HDL)-C, apolipoprotein A (Apo A), apolipoprotein B, and lipoprotein a were measured. TG (P = 0018) and VLDL (P = 0.022) were lower in CAPD group than HD group, HDL-C (P < 0.001) and Apo A (P = 0.001) were higher in CAPD group than in HD group. A total of 24.4% in CAPD group and 11.4% in HD group (P < 0.034) had normal serum levels of TG, LDL-C, and HDL-C. More patients in CAPD group (47.4%) had high serum Apo A levels than in HD group (21.5%) (P = 0.001). We suggest that patients receiving icodextrin-based CAPD may have better TG, HDL-C, and Apo A levels than patients on HD.
Keywords
Continuous ambulatory peritoneal dialysis
dislipidemia
hemodialysis
icodextrin
lipoprotein abnormalities
Introduction
Dyslipidemia can develop a result of changes in the lipoprotein metabolism of patients with end stage renal disease (ESRD). Uremic dyslipidemia is caused by a decreased catabolism of apoprotein-Bcontaining lipoproteins due to decreased activity of lipolytic enzymes and altered lipoprotein composition. Additionally, the excessive peritoneal glucose absorption from high glucose-containing peritoneal dialysis solutions may enhance disturbances on the lipid metabolism in patients on continuous ambulatory peritoneal dialysis (CAPD).
Some data about the consequences for lipid metabolism related to a reduced peritoneal glucose uptake in CAPD patients are available. However, there are no avaliable data that compare the lipid parameters between icodextrin-based peritoneal dialysis therapy and hemodialysis (HD) therapy, so we compared the effect of icodextrin-based peritoneal dialysis therapy with HD therapy on lipid metabolism in dialysis patients.
Materials and Methods
A total of 157 non-diabetic ESRD (78 CAPD, 79 HD) patients who were followed up for at least 3 months in Dialysis Unit of Dicle and Trakya Universities, Medical Faculty Hospitals in 2008, were included in this cross-sectional study. The study was approved by local ethical committee and informed consent form was taken from patients.
Subjects were 18-65 years old, non-diabetic ESRD patients treated with dialysis (HD or CAPD) regularly, over 50% ejection fraction, did not have hypothyroidism, chronic liver disease, ischemic heart disease (defined as ST segment depression on ECG), and obesity (defined as body mass ύndex [BMI] (kg/m2> 30), and also not on antilipidemic drug.
Patients with diabetes mellitus, and congestive heart failure, and coronary artery disease, and obesity, and using antilipidemic drugs, patients who using high glucose containing peritoneal dialysis solutions, and known history of familial hyperlipidemia, and those who did not want to participate in the study were excluded.
Demographic information of the patients was recorded from the registry in the dialysis unit, and BMI was calculated with this formula (body weight [kg]/length [m]2).
CAPD patients (Group 1) were treated with low glucose containing peritoneal dialysis solution 2000 cc × 3/day and icodextrin-containg solution 2000 cc 1 × 1/day. HD patients (Group 2) were treated with low-flux polysulfone hollow-fibre dialyzer, three times a week, 5 h, with bicarbonate and unfractionated heparin.
After 12-h of fasting period before dialysis sessions, blood samples were used for biochemical analysis of serum urea, creatinine, glucose, sodium, potasium, Albumin, and measured by Aeroset/C8000 autoanalyzer apparatus (Abbott Diagnostics, USA), in the Central Laboratory of Medical School, Dicle University. After the blood samples were taken to EDTA tubes for lipids and apolipoproteins, they were immediately centrifuged and the plasma was frozen and stored at 70°C, then total cholesterol (TC), triglycerides (TG), low density lipoprotein (LDL), high-density lipoprotein (HDL), very low density lipoprotein (VLDL), and apolipoprotein A-1 (Apo A), apolipoprotein B (Apo B) and lipoprotein (a) were measured by the IMMAGE Beckman Coulter 800 (Beckman Instruments Inc., Brea, CA, USA) device using nephelometric method in the Central Laboratory of Medical School, Trakya University.
The statistical analysis was performed by SPSS 16.0 for Windows PC program. Dependent and independent variables of the groups were compared by Student’s t-test. Chi-squared tests were used to determine the relationship between the dependent variables. Data were shown as mean value ± SD Results were in 95% confidence interval and P < 0.05 was accepted as significant.
Results
Etiologic factors are shown in Table 1. The demographic and biochemical parameters were summarized in Table 2. The levels of lipids, lipoproteins, and apolipoproteins are summarized in Table 3.

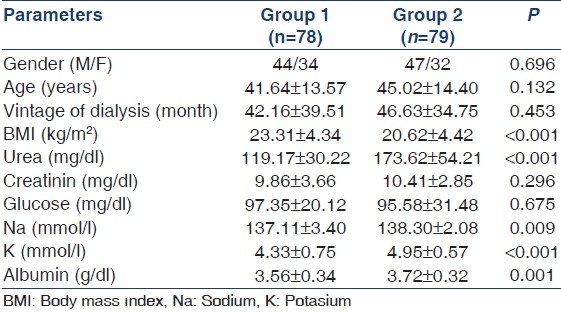
Patients who were on target for TG and HDL according to ATP III dyslipidemia in clinical practice guidelines are shown in Table 4.
The patients who had normal lipid levels are shown in Figure 1. The patients who had high Apo B, Apo AI, and Lipoprotein a (Lp [a]) levels are shown in Figure 2.
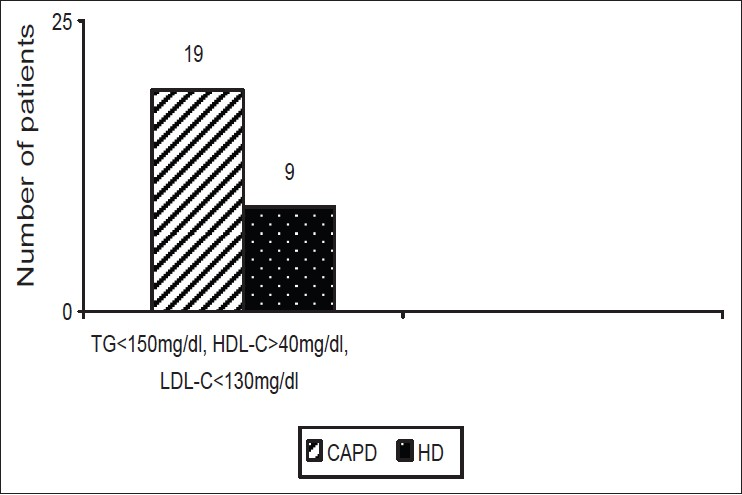
- The patients whose lipid levels were in normal range
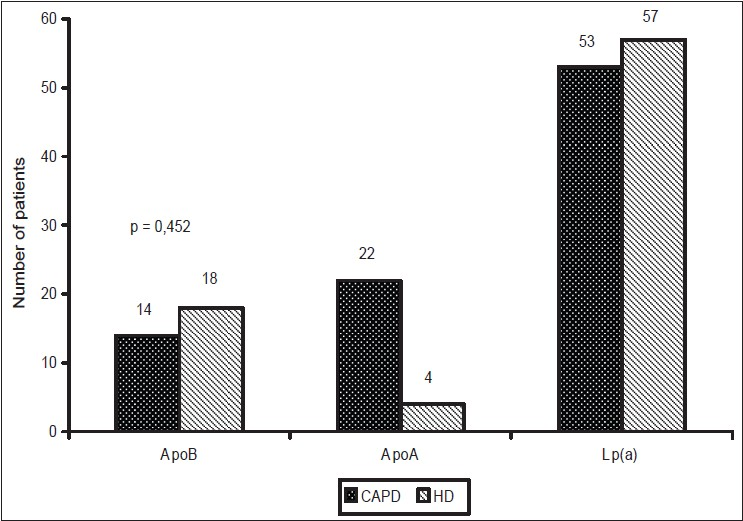
- The patients who have high Apolipoprotein B, Apolipoprotein A and Lipoprotein a levels
Discussion
Today, dyslipidemia is a well-known and traditional risk factor for adult society but also poses a risk for ESRD patients with significant changes in lipoprotein metabolism.[1]
The most significant changes in lipids and lipoprotein metabolism in ESRD patients are elevation in TG and accumulation of atherogenic VLDL remnants and triglyceride-rich apoB -containing lipoproteins, and a decrease in cholesterol ester-rich cardioprotective HDL-2, in apo A-I, apo A-II and apo E concentrations whereas that of Apolipoprotein C (apoC)-III is elevated and the apoC-II-to-apoC-III concentration ratio is diminished.[2]
The typical disorder is high TG and low HDL levels observed in patients treated with HD and/or peritoneal dialysis. High TG and low HDL levels ranged at 30-50% ratio in this population.[34] Attman et al.,[56] reported that the lipid profiles of the patients mainly remained unchanged in a long-term HD program, reflecting the lipid and apolipoprotein profiles of the pre-dialysis period of these patients. Based on these knowledge, the triglyceride-rich lipoproteins and Lp (a) levels were observed to increase and the levels of HDL-C decreased.
Furthermore, it has been reported that lipid profile of CAPD patients is more atherogenic than age and sex-matched healthy individuals, so that TC, LDL-C, apo B, Lp (a), and TG increase and HDL-C decrease.[78]
However, the pathophysiological mechanism of dyslipidemia in CAPD patients has not been very well defined. It has been said that in the clinical studies there is a multi-factorial mechanism affecting this condition.[9]
It has also been suggested that increased levels of LDL-C and Lp (a)[1011] by hepatic production of albumin and cholesterol-rich lipoprotein induced by protein loss into the peritoneal dialysate elevate the hepatic synthesis and secretion of VLDL and Lp (a)[12] by increases at insulin levels due to increased absorption of dialysate glucose, and especially the loss of significant amounts of HDL-C[1314] and apolipoproteins into the dialysate may play a role in dyslipidemia of CAPD patients.
However, recent clinical trials using PD solutions containing icodextrin rather than glucose have shown favorable effects on serum levels of TC and LDL-C beside TG.[1516]
These studies show that the icodextrin reduces the rate of glucose absorption, and lipid profile would not be atherogenic.
In the current study, we established that the number of the patients with high TG levels were 62% in Group 2 and 35.9% in Group 1 (P = 0.001), and the patients who had low HDL levels were 78.5% in Group 2 and 52.6% in Group 1 (P = 0.001).
When we compare the serum levels of apolipoproteins, there was no difference between the two groups in terms of Apo B but Apo A levels were statistically higher in Group 1 than Group 2. In addition, we found that the patients who had high Apo A levels were much more in Group 1 than Group 2 but there was no significant difference for Apo B and Lp (a) in both groups respectively.
In contrast to knowledge about this subject, our results suggest that icodextrinbased CAPD does not have a negative effect on lipid profile of the ESRD patients.
When we look at the literature, we see that TC and LDL-C levels are normal or low especially in HD patients, but CAPD patients have different situations.[17] In CAPD patients, high LDL-C levels are more frequently encountered than HD patients.[18] In our study, we found that the mean LDL-C levels in both groups were within acceptable limits. In Group 2, LDL-C levels were normal in line with literature values, but those obtained for Group 1 did not confirm high levels of LDL-C as mentioned in the literature.
The kidneys are very active in participating in Lp (a) degradation. After CKD develops, the degradation of Lp (a) does not occur; therefore, the level of Lp (a) increases in ESRD patients.[1920] Haffner et al.,[21] reported that Lp (a) increases in early renal disease, and regular dialysis treatment has no significant effect on the level of Lp (a).
In conclusion, we suggest that patients receiving icodextrin-based CAPD therapy may have better TG, HDL-C, and Apo A levels than patients receiving HD treatment. Also we can say that lowest glucose containing regimes especially with icodextrin solution may have beneficial effect on lipid metabolism in the ESRD patients treated with CAPD. Nevertheless, large-scale prospective controlled clinical studies are needed on this subject.
Acknowledgment
We thank to Mr. Ibrahim Tunik to his contribution on language of this manuscript.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Blood cholesterol and vascular mortality by age, sex, and blood pressure: A meta-analysis of individual data from 61 prospective studies with 55,000 vascular deaths. Lancet. 2007;370:1829-39.
- [Google Scholar]
- Dyslipidemia of chronic renal failure: the nature, mechanisms, and potential consequences. Am J Physiol Renal Physiol. 2006;290:F262-72.
- [Google Scholar]
- Hyperlipidemia in patients with chronic renal disease. Am J Kidney Dis. 1998;32:S142-156.
- [Google Scholar]
- Cardiovascular disease determinants in chronic renal failure: Clinical approach and treatment. Nephrol Dial Transplant. 2001;16:459-68.
- [Google Scholar]
- Apolipoprotein B-containing lipoproteins in renal failure: The relation to mode of dialysis. Kidney Int. 1999;55:1536-42.
- [Google Scholar]
- Atherogenic lipoprotein phenotype in end-stage renal failure: Origin and extent of small dense low-density lipoprotein formation. Am J Kidney Dis. 2000;35:852-62.
- [Google Scholar]
- Prevalence of dyslipidemic risk factors in hemodialysis and CAPD patients. Kidney Int Suppl. 2003;84:S113-6.
- [Google Scholar]
- Abnormalities of lipoprotein metabolism in CAPD patients. Kidney Int Suppl. 1996;56:S41-6.
- [Google Scholar]
- Protein loss and genetic polymorphism of apolipoprotein (a) modulate serum lipoprotein (a) in CAPD patients. Nephrol Dial Transplant. 1995;10:75-81.
- [Google Scholar]
- Increased plasma lipoprotein (a) in continuous ambulatory peritoneal dialysis is related to peritoneal transport of proteins and glucose. Nephron. 1996;72:135-44.
- [Google Scholar]
- Dysl ipidemia in peritoneal dialysis relation to dialytic variables. Perit Dial Int. 2000;20:306-14.
- [Google Scholar]
- Kinetics of peritoneal protein loss during CAPD: II. Lipoprotein leakage and its impact on plasma lipid levels. Kidney Int. 1990;37:980-90.
- [Google Scholar]
- Apo AIV in plasma and dialysate fluid of CAPD patients: Comparison with other apolipoproteins. Nephrol Dial Transplant. 1992;7:1026-9.
- [Google Scholar]
- Dyslipidemia in peritoneal dialysis- Relation to dialytic variables. Perit Dial Int. 2000;20:306-14.
- [Google Scholar]
- Effects of peritoneal dialysis with an overnight icodextrin dwell on parameters of glucose and lipid metabolism. Perit Dial Int. 2001;21:275-81.
- [Google Scholar]
- Atherogenic lipoprotein phenotype in end-stage renal failure: Origin and extent of small dense low-density lipoprotein formation. Am J Kidney Dis. 2000;35:852-62.
- [Google Scholar]
- Decreased low-density lipoprotein receptor function and mRNA levels in lymphocytes from uremic patients. Kidney Int. 1992;42:1238-46.
- [Google Scholar]
- Increased plasma lipoprotein (a) in continuous ambulatory peritoneal dialysis is related to peritoneal transport of proteins and glucose. Nephron. 1996;72:135-44.
- [Google Scholar]
- Increased lipoprotein (a) concentrations in chronic renal failure. J Am Soc Nephrol. 1992;3:1156-62.
- [Google Scholar]







