Translate this page into:
Clinical Profile and Outcome in Long-term Hemodialysis: A Comparative Study of Hospital-based Versus Standalone Units
-
Received: ,
Accepted: ,
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Chronic hemodialysis (CHD) remains the most “resorted to“ renal-replacement option in India. Pursuit for accessible and affordable dialysis has resulted in setting up standalone centers (SACs). We need more Indian data on the profile of CHD population and outcome of SAC compared to hospital-based units (HBUs).
Material and Methods:
We analyzed the clinical profile of patients on CHD for >5 years, compared the outcome between HBU and SAC, and analyzed the factors associated with mortality. Patients initiated between January 1, 2006 and December 31, 2012 and who have survived 5 years on CHD at HBU or SAC were enrolled and followed up prospectively for 2 years. Their clinical and biochemical profile, comorbidities, long-term complications, and mortality were analyzed.
Results:
The study included 137 patients, 41 (30%) from HBU and 96 (70%) from SACs. In both groups, the patients were predominantly male, aged 51–70 yrs, diabetic, unplanned initiation through catheters, and had average-dialysis vintage between 83 and 85 months. SAC had more patients with hemoglobin (> 11 gm/dL) and hyperparathyroidism with elevated SAP levels (P < 0.05). Both groups had comparable iron stores, serum calcium, and phosphorus. Comparable between groups, infections, coronary artery disease, and access complications accounted for most hospitalizations and sudden cardiac death and sepsis accounted for most mortality. A trend of better survival was seen in SAC. Multivariate analysis showed anemia, DM and hospitalizations were associated with mortality.
Conclusion:
We conclude that the outcomes of long-term CHD at SACs are not inferior to HBUs. Anemia, diabetes, and hospitalizations were associated with overall mortality. Benefits of SACs in cost, QOL, and employment opportunities need to be studied in the Indian context.
Keywords
Clinical profile
hemodialysis
long term
outcome
stand-alone centers
Introduction
Hemodialysis programs started in India on an institutional basis since 1960s, but its expansion was static for subsequent four decades due to a multitude of reasons like lack of awareness, late referrals, shortage of expertise, and lack of accessible affordable facilities.[1] Despite advancements in recent couple of decades, as per recent data, still only 30% of ESRD population resort to some form of renal replacement therapy.[2] From a public health perspective, government subsidies and social support platforms have surfaced in last two decades to facilitate hemodialysis to the increasing number of needy population subjugating to a large extend the once formidable challenges like affordability and accessibility.[34] As an offshoot of aforementioned support systems, standalone dialysis centers (SAC) were started in the country over the last decade further expanding the hemodialysis pool.[5]
There is a dearth of outcome data on patients on long-term chronic hemodialysis (CHD) which is sorely needed to justify the amount of public money and effort being invested in the program. The available data, mostly from individual centers with short follow-ups underrepresents the important complications of CHD like mineral bone disease, long-term access issues, vascular calcification, calciphylaxis, and cardiovascular complications.
In India, the hemodialysis care delivery is increasingly being done by SACs. Dialysis outcome studies should include data from SACs for meaningful appraisal. There are concerns on safety and quality of dialysis at SAC not only in the society but also among the medical community.
We aim to study the clinical profile of patients who have completed five consecutive years on CHD, prospectively analyze their outcome over a 2-year follow-up period, and to compare the outcome between patients on HD from a hospital-based unit (HBU) and a SAC.
Methods
Consecutive patients with ESRD who were initiated on hemodialysis between January 1, 2006 and December 31, 2012 and who have survived consecutive 5 years on CHD either from our HBU or from attached SACs were enrolled and followed up prospectively for a period of 2 years. An informed consent was obtained from all the patients and the study was approved by the institutional ethics committee (IEC Reg No. ECR/301/inst/KL/2013). Patient and relatives were interviewed in person during scheduled visits and data were collected from hospital information system. Data was manually entered to EXCEL sheets created as per compatible proforma.
Patients who did not consent for enrolment, not on thrice a week HD, switched over to other forms of renal replacement therapy (RRT) like renal transplantation (RT) or CAPD at any time point and those lost to follow up were excluded. At baseline, demographic profile, details of native kidney disease, and comorbid conditions were collected. At baseline and at prefixed intervals through the study period, clinical data and investigations like hemoglobin, iron saturation, serum albumin, calcium, phosphorus, parathyroid hormone (iPTH), and serum alkaline phosphatase (ALP) were collected. Indication and details of OPD visits, hospitalization and death were also recorded as per the standard proforma. The patients were followed up for 2 years from the start of study or until death.
Overview of SAC and guidelines for transfer to SAC:
Our hospital has nine attached SACs with average machines strength of 10 per unit. The average staff pattern for a 10 bedded dialysis unit includes 10 dialysis nurse and technician together, 3 nursing assistants, 2 house-keeping staff, and one receptionist cum accountant. Clinical monitoring includes rounds by nephrologist in each unit at least twice a week and by senior supervisor technician once a week. The SACs are funded and managed by NGOs and some centers get financial support from government schemes and CSR programs. Minimum 2 weeks of uneventful HD from primary HBU, stable cardiac status, easy to access mature AV-fistula, no concerning comorbidity like liver failure, severe heart failure or bleeding diathesis, and proximity to the HBU were major criteria to be accepted to a SAC.
Serology and biochemistry testing protocols of dialysis units:
Six monthly checking of HbsAg and anti-HCV antibody. Avoiding reuse of dialyzer at other centers in case of travel. Obligatory segregation of tubings and dialyzers of serology positive patients was the rule. Monthly complete blood counts, serum potassium, serum calcium and serum phosphorus, and 3–6 monthly ALP, serum albumin, transferrin saturation, and parathyroid hormone levels.
Hemodialysis details: Standard bicarbonate hemodialysis was given for 4 h three times a week. Dialyzer by protocol was high flux (Fresenius Polysulfone – F60s); dialysate flow rate was 500 mL/min; and blood flow rates were targeted more than 350 mL/min. Dialyzer reuse was uniformly performed using manual methods as per “Standard operating procedure” (SOP). Details regarding the type of vascular access, hepatitis B vaccination, erythropoietin use, and the complications on hemodialysis including vascular access related ones were recorded. No formal dialysis adequacy determination was done (by Kt/V calculation).
Study outcomes: The outcomes of the study were (a) To analyze the baseline characteristics regarding demographics, native kidney disease, dialysis access and access history, comorbidities, past infections, mineral bone disorder, and anemia of chronic kidney disease in patients on MHD for more than 5 years. (b) Prospectively compare and analyze the biochemical profile and clinical outcomes like incidence of access complications, reasons for outpatient visits, incidence of new infections, hospitalizations, and death were documented and compared between the HBU and SAC groups. (c) To analyze the causes of overall mortality and potential factors associated with mortality
Statistics: Data was analyzed using GraphPad version 7. Continuous data, summarized as mean with SD was analyzed with t-test. Median was calculated instead of mean if values did not have normal distribution. One-way ANOVA was used for comparison of three sets of continuous variables. Categorized data was analyzed using Fisher's exact test. Patient survival was analyzed with Kaplan Meier plot with Gehan Breslow test. Multivariate logistic regression analysis was done using software Epi Info version 7. For all tests, P value less than 0.05 was considered as statistically significant.
Results
Four hundred and eighty-one patients were initiated on hemodialysis at our center from January 1, 2006 to December 31, 2012. Our study included 137 out of the 481 patients who survived 5 years on hemodialysis without an interruption with other modalities like CAPD and RT. Forty-one (30%) patients were on CHD from our HBU and 96 (70%) were from nine SACs attached to our nephrology service, as shown in Figure 1.

- Flowchart of patient selection
Demographic data as depicted in Table 1 do not show any significant difference in mean age, gender, etiology of CKD, or co morbidities between the two groups. More than 50% of the patients in both groups were of age between 51 and 70 years. The mean hemodialysis duration was comparable with 85.1 ± 8.5 months in HBU and 83.7 ± 4.5 months in the SAC group. About 75% in HBU and 50% in SAC had third party finance support like private insurance, Employees’ State Insurance Corporation (ESI) or Ex-servicemen Contributory Health Scheme (ECHS).
| Hospital-based unit (HBU) n=41 | Standalone center (SAC) n=96 | |
|---|---|---|
| Gender:Male n (%) | 31 (75.6) | 65 (67.7) |
| Age (in years) | 56.6±11.8 | 53.6±12.6 |
| Age groups - n (%) | ||
| <30 yrs | 2 (4.8) | 4 (4.2) |
| 31-50 yrs | 11 (26.8) | 37 (38.5) |
| 51-70 yrs | 23 (56) | 50 (52) |
| >70 yrs | 5 (12.2) | 5 (5.2) |
| Mean dialysis duration (in months) | 85.1±8.5 | 83.7±4.5 |
| Dialysis vintage in months - n (%) | ||
| 60-90 months | 29 (70.7) | 73 (76) |
| 91-120 months | 9 (22) | 17 (17.7) |
| >120 months | 3 (7.3) | 6 (6.3) |
| Native kidney disease - n (%) | ||
| Diabetes Mellitus | 22 (53.6) | 40 (41.7) |
| Chronic GN | 6 (14.6) | 25 (26) |
| CTID | 4 (9.6) | 8 (8.2) |
| Others | 9 (22) | 23 (24) |
| Co-morbidities - n (%) | ||
| HTN on medications | 29 (70.7) | 78 (81.2) |
| CAD | 15 (36.5) | 37 (38.5) |
| CVA | 5 (12.2) | 7 (7.3) |
| Peripheral artery disease | 4 (9.8) | 12 (12.5) |
| Tuberculosis | 5 (12.2) | 12 (12.5) |
| Hepatitis B and C | 3 (7.3) | 13 (13.5) |
| First AV access - n (%) | ||
| Vascular catheter | 30 (73.2) | 71 (74) |
| AV fistula | 11 (26.8) | 25 (26) |
| Secondary AVF failure - n (%) | 14 (34.2) | 24 (25) |
| 3rd party finance support- n (%) | 31 (75.7)* | 54 (56) |
| Enlisted in deceased donor WL - n (%) | 7 (17) | 10 (10.4) |
*Indicates P<0.05
Basic demographic details are shown in Table 1 and biochemistry and laboratory tests are shown in Table 2. The trend of calcium, phosphorus, and ALP levels over the 24 month study period did not show any significant variation from that of enrolment among patients in each group. iPTH levels in SAC group were significantly lower at 12 and 24 months compared to the corresponding level on enrolment; this trend was not appreciable in the HBU group (Supplementary Table 1). Twenty-five (61%) patients of HBU group had anemia compared to 32 (33%) in SAC. In the SAC group, 65.6% had Hb >11 gm/dL, whereas in HBU, 60% had hemoglobin of <11 gm/dL. The proportion of patients with Hb >11 g/dL improved over the 24 month study period, from 40 to 64% in HBU and from 67 to 75% in SAC. Complications during the 24 months of follow-up study are summarized in Table 3. As shown in Figure 2, outpatient clinic visits were most common to cardiology and orthopedic services. Significantly more patients from HBU (43.9%) had sought OP clinic visits to cardiology department compared to SAC (15.6%).
| Hospital-based unit (HBU); n=41 | Standalone center (SAC); n=96 | |
|---|---|---|
| Calcium (Ca) mg/dl^ | 8.9 | 8.9 |
| Phosphorus (P) mg/dl^ | 4.2 | 4.4 |
| Ca X P product^ | 36 | 39 |
| Intact PTH pg/mL | 493±12.9 | 697±15.6* |
| Alkaline phosphatase IU/L | 180.8±13 | 223.5±15.6* |
| Phosphate binder - n (%) | ||
| Calcium Based | 17 (41.5) | 49 (51) |
| Non calcium based | 17 (41.5)* | 15 (15.6) |
| None | 7 (17) | 32 (33.3) |
| Vitamin D3 supplements - n (%) | 18 (43.9) | 40 (41.6) |
| Parathyroidectomy - n (%) | 1 (2.4) | 2 (2.1) |
| Hemoglobin, n (%) | ||
| > 11 gm/dL | 16 (39.1) | 63 (65.6) * |
| 9-11 gm/dL | 24 (58.5)* | 29 (30.2) |
| <9 gm/dL | 1 (2.4) | 3 (3.2) |
| Iron saturation - n (%) | ||
| >20% | 35 (85.3) | 86 (89.6) |
| <20% | 6 (14.7) | 10 (10.4) |
| EPO - n (%) | ||
| >10000 IU per week | 9 (22) * | 5 (5.2) |
| <10000 IU per week | 21 (51.2) | 63 (65.6) |
| None | 11 (26.8) | 28 (29.2) |
*Indicates P<0.05. ^Expressed in median, *Indicates P<0.05
| Hospital-based unit (HBU) n=41 | Standalone center (SAC) n=96 | |
|---|---|---|
| Calcium (Ca) mg/dL | ||
| On enrolment | 9±0.4 | 8.9±0.6 |
| At 12 months | 8.9±0.23 | 8.9±0.4 |
| At 24 months | 8.8±0.76 | 8.9±0.6 |
| Phosphorus (P) mg/dL | ||
| On enrolment | 4.2±1.06 | 4.3±1.15 |
| At 12 months | 4.2±0.96 | 4.4±1.40 |
| At 24 months | 4.6±1.18 | 4.4±1.23 |
| Intact PTHpg/mL | ||
| On enrollment | 493±12.9 | 697±15.6* |
| At 12 months | 427±34.79 | 498±14.6* |
| At 24 months | 642±17.5 | 401±10.4* |
| Alkaline phosphatase IU/L | ||
| On enrollment | 180.8±13 | 223.5±15.6 |
| At 12 months | 175±23 | 232.8±14.5 |
| At 24 months | 176±17 | 204.8±13.3 |
| Hospital-based unit (HBU) n=41 | Standalone center (SAC) n=96 | |
|---|---|---|
| Coronary artery disease -n (%) | 6 (14.6) | 4 (4.2) |
| Infection-n (%) | 7 (17) | 11 (11.4) |
| Volume overload-n (%) | 0 | 2 (2.1) |
| Fractures-n (%) | 2 (4.9) | 3 (3.1) |
| CVA -n (%) | 1 (2.4) | 0 |
| Access-related complications n (%) | 2 (4.9) | 7 (7.3) |
| Total hospitalization -n (%) | 18 (44) * | 20 (28) |
*Indicates P<0.05
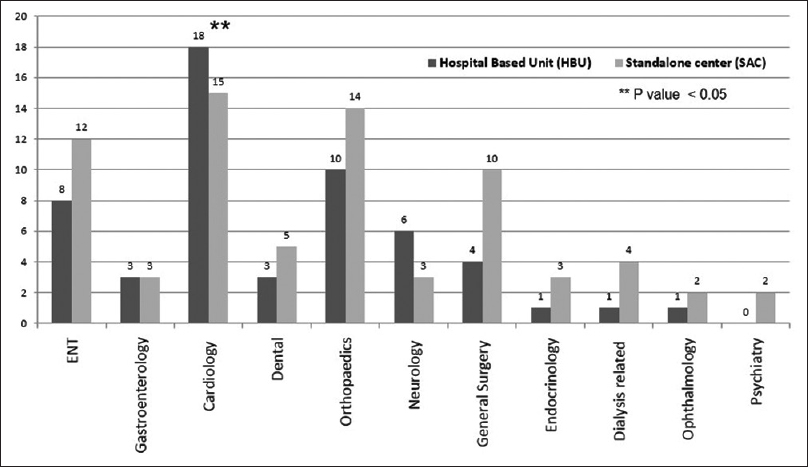
- Outpatient visits during 24 months follow-up
As shown in Figure 3, eight (19.5%) from HBU group and eight (8.3%) from SAC group died during the 24 months follow-up study. Sudden cardiac death and sepsis were the most important reasons for death in both groups. Acute coronary syndrome was the third important cause for mortality. Though the death was comparable in both groups for those patients who already have a survival benefit for having survived 5 years on maintenance dialysis, the Kaplan Meier plot shows a trend for better survival in patients in SAC (P = 0.08), as shown in Figure 4. We analyzed the association of certain factors with mortality proven in prior studies like age, gender, diabetes mellitus, anemia, dialysis vintage, predialysis care, access complications, coronary artery disease, diastolic dysfunction, abnormal bone mineral disorder, hyperparathyroidism, and hospitalization.[67] Age, diabetes mellitus, anemia, coronary artery disease, and hospitalization were found to be significantly associated in univariate analysis [Table 4]. In multivariate analysis, only anemia, diabetes mellitus, and need for hospitalization were found to be significantly associated with mortality [Table 4].
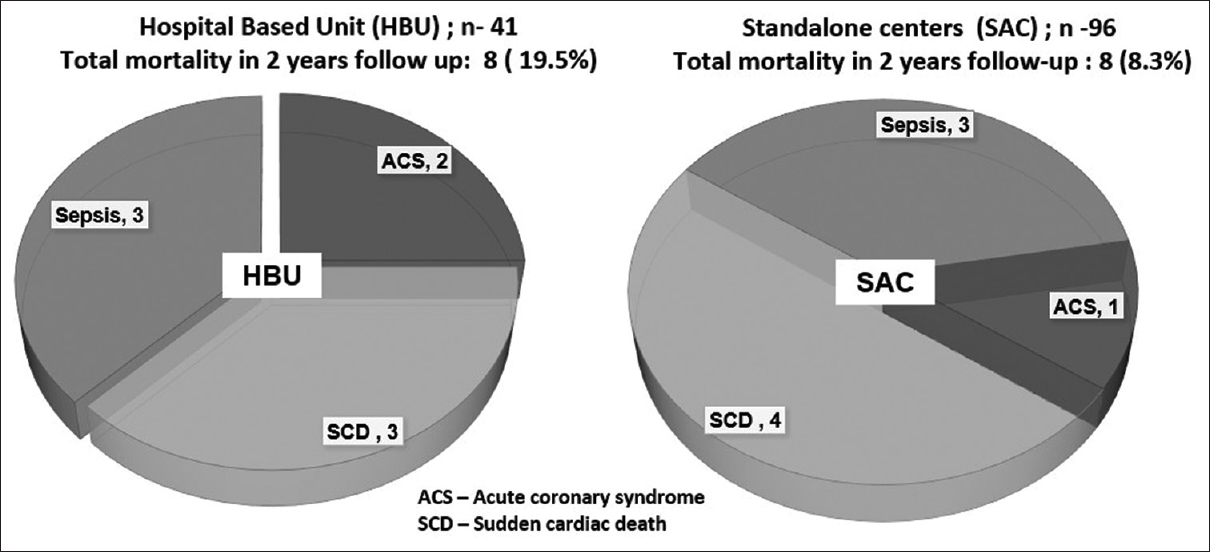
- Causes of mortality between HBU and SAC
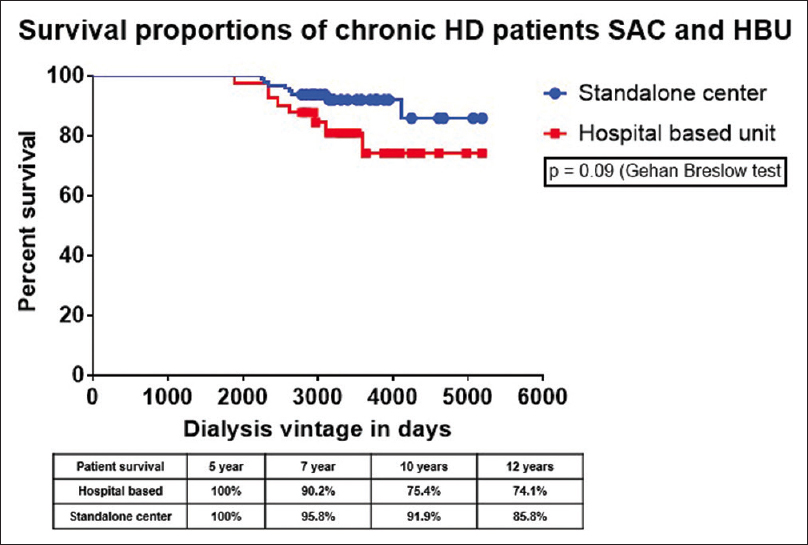
- Comparison of survival curves between HBUs and SACs
| Expired group n=16 (%) | Surviving group n=121 (%) | Significance P | Multivariate analysis | |||
|---|---|---|---|---|---|---|
| Adjusted OR | 95% CI | P | ||||
| Age | 62.75±2.84 | 53.48±1.10 | 0.0046®® | 1.0704 | 0.998-1.148 | 0.566 |
| Gender M: F | 11:5 | 85:36 | NS | |||
| DM: Non-DM | 13:3 | 49:72 | 0.0027** | 5.3360 | 1.183-24.058 | 0.0293ªª |
| Dialysis vintage (months) | 79.5±4.67 | 82.31±2.28 | NS | |||
| Elective: unplanned | 5:11 | 24:95 | NS | |||
| None or <1:>1 access failures | 4:12 | 21 :98 | NS | |||
| CAD: Non-CAD | 11 : 5 | 41:78 | 0.0125** | 2.3329 | 0.630-8.636 | 0.2046 |
| Diastolic dysfunction | 8: 8 | 39:80 | NS | |||
| Hyperparathyroidism | 5:11 | 48:71 | NS | |||
| Serum calcium level | 8.9 | 9.0 | NS | |||
| Serum phosphorus | 4.3 | 4.3 | NS | |||
| Calcium X phosphorus product | 38 | 39 | NS | |||
| Hb <11: >11 g/dL | 11:05 (68.7%) | 46:75 (38.0%) | 0.0290** | 4.2295 | 1.186-15.073 | 0.0261ªª |
| Hospitalization unrelated to HD | 6 | 13 | 0.0107** | 5.8166 | 1.283-26.361 | 0.0224ªª |
DM - Diabetes mellitus; CAD - Coronary artery disease; iPTH - intact parathormone; HPTH pts - hyperparathyroid patients ; Hb - hemoglobin; ®®Unpaired t-test;** - Fisher’s exact test; OR - Odd’s ratio; CI - Confidence interval; ªªLogistic regression
Discussion
India like many other developing countries lacks registries to capture chronic dialysis data handicapping the nephrology community in strategizing dialysis care to improve long-term outcome. Hemodialysis still remains the most resorted to chronic RRT option in India followed by RT pushing CAPD to the last option resorted by only <1% of ESRD patients. Lack of data regarding prevalence of CKD makes it difficult to ascertain the number of stage 5 CKD group, which needs RRT. Only around 15–20% of patients initiated on dialysis undergo RT in India.[26]
Published studies on CHD population from India are primarily single-center studies whose follow up is within 3 years of initiation and have shown high early dropout rates with mortality around 9–20%.[678] The first population-based multicenter study from south India that analyzed outcomes of a publicly funded state model of hemodialysis showed very high dropout rate of 50%, which presumably resulted in patient mortality despite financial support.[9] Our study, first of its kind from India tries to identify the clinical profile and outcome of patients with survival advantage of having crossed first five years of hemodialysis supervised by nephrology service. This subgroup of hemodialysis population has its own unique set of complications like hyperparathyroidism, AV access complications, vascular calcification, cardiovascular complications, and acquired cystic kidney disease, and our study provides an opportunity to study its prevalence along with outcome in Indian population.
Accessibility and affordability still remains the formidable hurdles in dialysis delivery in India, where more than 60% of needy patients reside in rural India with proportionately much less facilities.[10] Since setting up the first standalone satellite dialysis center in North Kerala in 2009, more and more SACs have been started in the region with concept of giving dialysis closer to the rural communities. In north Kerala, currently about 75% of CHD is being done in SACs faraway from urban tertiary care centers.[11] Data from developed world have shown comparable outcomes like mortality and Quality of Life indices in SACs with respect to tertiary care HBU.[121314] Our study tries to compare the outcomes like comorbidities directly and indirectly related to CKD and hemodialysis, hospitalization rates, and mortality between SAC and HBU. The financial model of SAC supported by philanthropists and local administration has reduced the out-of-pocket expenses toward hemodialysis by 40–70% compared to expenses at HBUs which accounted about 40–80% of nonfood expenses of a dialysis patient.[515]
Of the 481 patients initiated on CHD between January 1, 2006 and December 31, 2012, 121 (25%) patients underwent RT. Of the 360 patients who continued on hemodialysis, 137 (38%) patients survived beyond 5 years on uninterrupted hemodialysis, which is almost comparable to 42% reported in USRDS data. Another center from Kerala had shown 21% 5-year survival in a tertiary care hospital dialysis facility. Our patient population was predominantly male at a proportion comparable with all other Indian studies where it ranged between 65 and 70%. Diabetes mellitus was the most common cause for ESRD like most of the studies from India. Similarly, with more than 80 months of vintage on dialysis, the age of initiation for majority of patients were of the age group between 40 and 50 years. History of tuberculosis was present in 12% of our patients which was similar to two other programs; Chronic hepatitis B and C together were seen in 10% of our patients which was higher than one study with reported 5.6% in their cohort.[67] No patient seroconverted in the 2-year follow-up period. We did not find any difference regarding aforementioned baseline characteristics between the patients getting dialyzed at HBU and SAC. Contrary to our expectation proportionately more patients (75%) in HBU compared to SAC (56%) were getting third-party financial support in the form of private insurance, ESI, or ECHS schemes.
First vascular access was venous catheters in 70% of our patients, which is similar to most of the Indian studies. In both HBU and SAC, more than 25% patients had secondary failure of working AV –access, which necessitated creation of alternate access at the time of enrolment. The active access on enrolment of the study was AVF in 93% of HBU and 99% of SAC patients. During the 24-month follow-up period, three patients from HBU and one patient from SAC had secondary AVF failure of which two of HBU group had to resort to AV-graft placement. During the 24-month study period, two patients from HBU and seven from SAC had to undergo hospitalization for access-related complications like infection, hematoma, and aneurysm needing repair. Around 35% patients from HBU and SAC had documented coronary artery disease warranting treatment.
There is a dearth of Indian data on biochemical and clinical parameters on long-term HD population. In our analysis, we found significantly elevated intact parathormone and SAP levels in patients from the SAC group despite having comparable serum calcium and phosphorus levels. HBU group was on more non-calcium-containing binders, probably due to difference in prescription pattern considering the allowance for expensive medications through their support schemes. Reasons remaining unclear, despite having comparable iron saturation levels and higher EPO administration, significantly more patients (60%) in HBU group had hemoglobin less than 11 g/dL compared to 33% in SAC group.
During the 2-year follow up, patients from HBU (44%) had relatively more hospitalization compared to SAC (28%), and the three most common reasons for seeking care were infection, coronary artery disease, and access complications, the incidence being same for all the three between the two groups. Outpatient clinic visits to cardiology were more in the HBU group probably due to easy accessibility from a hospital-based setting or might be harboring increased morbidity from cardiovascular standpoint.
In our study, the most common causes for mortality were acute coronary syndrome and sudden cardiac death which might be consubstantial, accounted for 60% of mortality. Other Indian studies have also shown more than 50% mortality due to aforementioned reasons. Around 35% in both HBU and SAC succumbed to sepsis due to various causes. The survival curves [Figure 4] though comparable, there is a trend of improved survival in SAC groups. Increasing age, coronary artery disease, anemia, diabetes mellitus, and hospitalizations for reasons not associated with hemodialysis were shown to be significantly associated with overall mortality, but on multivariate analysis, the former two were not of significance. Coronary artery disease which was found to be associated with prior two Indian studies got excluded in our study after the multivariate analysis.[67]
Our study provides an opportunity to compare the long-term outcome of SACs run on nonprofit basis with HBUs run for profit and has shown that outcomes from monitored SACs with regard to hospitalization, infection, access-related complication, and mortality are not inferior to a tertiary care HBU despite catering to a population with the same set of medical complications. Previous studies from the United States, probably due to different reasons which need to be studied, have shown a trend toward lesser mortality in nonprofit centers compared to for-profit dialysis units.[16] Transitioning dialysis care to an attached SAC after initial optimization at a HBU provides an opportunity for continuous care with very little dropout as evident in our study with only 5% dropout compared to 40% in other multicenter study.[9] With expanding role of SACs across the country, such outcome studies are critical for assessment and quality improvement. At this point, initiation of dialysis care from a tertiary care HBU and its turnout dynamics mark an identifiable starting point to plan and mobilize resources of dialysis infrastructure in a society. Regular nephrologist visits to unit covering all shifts and trained staff as per SOP with periodic audit is the backbone of the program. Like in our setting, nephrologists irrespective of their primary hospital affiliation can be pooled for coverage of SACs and could be advanced further to provide care breaking the public–private sector barriers. We hope more SACs come up attached with HBUs and work with standard SOPs with periodical outcome data.
One limitation of our study is the relatively short duration of prospective follow up of 2 years in a population on CHD for more than 5 years, but we are continually collecting data and can prospectively follow up further. Another limitation is lack of objective data like Kt/V to measure adequacy, clinical indicators like interdialytic weight gain for sudden cardiac deaths, residual renal function, and quality of life assessment for patient well-being and cost analysis for efficient fund utilization. Limitations inherent to retrospective data collection regarding baseline characteristics should also be factored in.
In conclusion, our study is the first study from India that has compared long-term outcome between SACs and HBUs, and our study shows that the outcomes are not inferior in monitored SACs compared to HBUs. The proven benefits of satellite SACs like lesser cost, better QOL, and employment opportunities should also hold for Indian scenario, but applicability across the country needs to be proven by studies and proper data collection (3). We need more cooperation between hospitals and nephrologists to come with a model network of SACs for proper utilization of resources as lot of public money is being spent on dialysis care.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Haemodialysis for end-stage renal disease in Southern India - A perspective from a tertiary referral care centre. Nephrol Dial Transplant. 1998;13:2494-500.
- [Google Scholar]
- ESRD burden in South Asia : The challenges we are facing. Clin Nephrol. 2015;83:7-10.
- [Google Scholar]
- The economic benefits of community-based stand-alone hemodialysis units (SAUs) in Kerala. Kidney Int Rep. 2019;4:898.
- [Google Scholar]
- End-stage renal disease patients on hemodialysis: A study from a tertiary care center in a developing country. Hemdial Int. 2011;15:312-9.
- [Google Scholar]
- Hemodialysis outcomes and practice patterns in end-stage renal disease: Experience from a Tertiary Care Hospital in Kerala. Indian J Nephrol. 2017;27:51-7.
- [Google Scholar]
- Survival analysis of patients on maintenance hemodialysis. Indian J Nephrol. 2014;24:206-13.
- [Google Scholar]
- Utilization, costs, and outcomes for patients receiving publicly funded hemodialysis in India. Kidney Int. 2018;94:440-5.
- [Google Scholar]
- Access to CKD care in rural communities of India: A qualitative study exploring the barriers and potential facilitators. BMC Nephrol. 2020;21:1-12.
- [Google Scholar]
- The expanding role of “Stand-Alone“ hemodialysis units in chronic renal replacement therapy: A descriptive study from North Kerala. Indian J Public Health. 2019;63:157-9.
- [Google Scholar]
- Hemodialysis in a satellite unit: Clinical performance target attainment and health-related quality of life. Clin J Am Soc Nephrol. 2011;6:1692-9.
- [Google Scholar]
- Model for equitable care and outcomes for remote full care hemodialysis units. Clin J Am Soc Nephrol. 2010;5:645-51.
- [Google Scholar]
- An evaluation of the costs, effectiveness and quality of renal replacement therapy provision in renal satellite units in England and Wales? Health Technol Assess. 2005;9(24):1-178. doi: 10.3310/hta9240. PMID: 15985188.15
- [Google Scholar]
- The expanding role of “Stand-Alone” hemodialysis units in chronic renal replacement therapy: A descriptive study from North Kerala. Indian J Public Health. 2019;63:157-9.
- [Google Scholar]
- Comparison of mortality between private for-profit and private not-for-profit hemodialysis centers: A systematic review and meta-analysis [published correction appears in JAMA 2004 Jan 14;291 (2):186] JAMA. 2002;288:2449-57.
- [Google Scholar]







