Translate this page into:
A Rare Case of Tuberculosis Masquerading as Collapsing Glomerulopathy
Corresponding author: Vijay Chander B, Department of Nephrology, Nizam’s Institute of Medical Sciences, Hyderabad, Telangana, India. E-mail: vijaychander.bukka@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kotha VK, Bukka VC, Niranjan M, Tiwari A, Herur S, Swarnalatha G. A Rare Case of Tuberculosis Masquerading as Collapsing Glomerulopathy. Indian J Nephrol. 2025;35:434-6. doi: 10.25259/ijn_443_23
Abstract
Collapsing glomerulopathy (CG), usually presents with renal dysfunction, hypertension and proteinuria. The etiology is uncertain, yet a number of associations, including many viral infections commonly have been reported. Tuberculosis (TB), one of the most common infections, is not known to cause CG. We report a case of severe renal dysfunction requiring dialysis who had collapsing glomerulopathy on biopsy and evidence of active pulmonary tuberculosis. Anti-tubercular therapy alone resulted in improvement in kidney function.
Keywords
Antitubercular therapy
Collapsing glomerulopathy
Immune dysregulation
Renal recovery
Tuberculosis
Introduction
Collapsing glomerulopathy (CG) is a clinicopathologic entity characterized by severe nephrotic syndrome and greater kidney function impairment than other histological variants of Focal segmental Glomerulosclerosis (FSGS) and carries a bad prognosis.1 HIV infection is a common cause of CG. In non-HIV population, most of the cases of CG are idiopathic, but a number of other disorders, including autoimmune, malignancy, genetic, and drug-induced collapsing glomerulopathies have been reported.2 Though tuberculosis is very commonly seen in India, there are only a few case reports suggesting tuberculosis as a secondary cause of CG. Here, we report a case of biopsy-proven CG with active pulmonary tuberculosis treated by anti-tubercular therapy.
Case Report
A 45-year-old male, presented with pedal edema and oliguria. He denied dysuria, hematuria, pyuria, fever, cough, SOB, weight and appetite changes. On examination, pallor was detected along with pedal edema, without lymphadenopathy; his blood pressure was 120/70 mmHg. Systemic examination revealed coarse rales bilaterally in lung bases. His investigations showed hemoglobin of 7.0 gm/dl, with leucocytosis and serum creatinine of 3.5 mg/dl with urinalysis showing proteins 4+, 18–20 Rbc, and plenty of pus cells. ANA and Anti ds DNA, ANCA were negative. He was started on dialysis. His chest X-ray showed left upper and middle lobe infiltrates. High resolution computed tomography (HRCT) chest showed patchy consolidation in the left upper lobe, fibrosis in both upper lobes with dilated pulmonary arteries.
On further probing, the patient gave a history of cough on and off which was not fully improving with antibiotics and antitussives. Meanwhile, kidney biopsy, was done and was reported as collapsing FSGS [Figures 1 and 2]. The other causes of FSGS (HIV, HBSAG and HCV, CMV and Parvoviral PCR) were negative. His mantoux was 15 mm; his induced sputum was negative for acid fast bacilli. Bronchoalveolar lavage samples after bronchoscopy were positive for acid fast bacilli. He was started on ATT. One week after starting ATT, his urine output increased to 1.5 liter, and he was discharged with creatinine of 5.0 mg/dl. One month after starting ATT, he had a serum creatinine of 3.2 mg/dl.
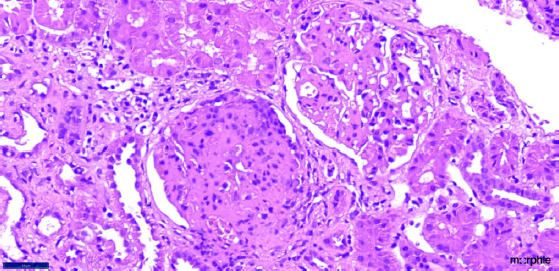
- Renal biopsy (40× magnification in H and E staining) depicting two glomeruli; the upper glomerulus is showing segmental sclerosis (9 to 12 o clock position) while the lower glomerulus is showing pseudocrescent with collapse of the glomerular tuft.
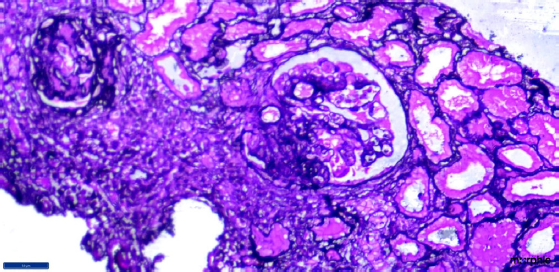
- Renal biopsy (40× magnification in silver stain) showing two glomeruli; the one on the right side of the field is showing segmental sclerosis from 6 to 9 o clock position with podocyte hyperplasia and collapsed glomerular tuft.
Discussion
CG is a recognized variant of FSGS, known to be associated with infections. However, only a few cases associated with pulmonary TB have been reported in the literature.3,4 Immune dysregulation due to infections in a genetically susceptible individual was causing changes in glomerulus consistent with CG.5,6 Coventry and Shoemaker reported steroid-resistant nephrotic syndrome in pulmonary TB. In view of absence of the usual associations, infection was the sole known risk factor.3 Another case of TB-related CG requiring dialysis for 5 months but with full renal recovery after TB treatment and corticosteroid therapy was reported by Rodrigues et al.4 Currently, there is no specific treatment for CG. However, steroids or immunosuppressive agents have been tried in idiopathic FSGS.5,6 Our patient responded to ATT, withimproved urine output and improvement in kidney function. However, long-term follow-up is needed to assess the progression of renal disease in this patient.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
References
- Clinical and pathologic characteristics of focal segmental glomerulosclerosis pathologic variants. Kidney Int. 2006;69:920-6.
- [CrossRef] [PubMed] [Google Scholar]
- Collapsing glomerulopathy: A 30-year perspective and single, large center experience. Clin Kidney J 2017:443-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Collapsing glomerulopathy in a 16-year-old girl with pulmonary tuberculosis: The role of systemic inflammatory mediators. Pediatr Dev Pathol. 2004;7:166-70.
- [CrossRef] [PubMed] [Google Scholar]
- Tuberculosis-associated collapsing glomerulopathy: Remission after treatment. Ren Fail. 2010;32:143-6.
- [CrossRef] [PubMed] [Google Scholar]
- Current views on collapsing glomerulopathy. J Am Soc Nephrol. 2008;19:1276-81.
- [CrossRef] [PubMed] [Google Scholar]







