Translate this page into:
A Rare Clinical Confluence: Metachromatic Leukodystrophy and Distal Renal Tubular Acidosis
Corresponding author: Nitish Kumar, Department of Pediatrics, Institute of Medical Sciences, Banaras Hindu University, Varanasi, India. E-mail: doctornitishkumar@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kumar N, Panda S, Shanker A. A Rare Clinical Confluence: Metachromatic Leukodystrophy and Distal Renal Tubular Acidosis. Indian J Nephrol. 2025;35:115. doi: 10.25259/IJN_336_2024
Dear Editor,
We present a case of a four-year-old female diagnosed with metachromatic leukodystrophy (MLD) who also exhibited distal renal tubular acidosis (RTA). She experienced loose stool, polyuria, and polydipsia for one year, along with regression of developmental milestones after her second year of life. Physical examination revealed rachitic rosary and wrist widening, while anthropometry indicated severe acute malnutrition (SAM) with severe stunting. Upper motor neuron signs were present on central nervous system examination. Blood gas analysis revealed severe normal anion gap metabolic acidosis. Additional tests revealed severe anemia with macro-ovalocytes, hyponatremia, hypokalemia, low serum calcium, high serum phosphate with normal serum creatinine. The urinary calcium creatinine ratio was elevated and the abdominal sonogram revealed medullary nephrocalcinosis. These findings were suggestive of distal RTA with renal rickets. Magnetic resonance imaging (MRI) brain findings were suggestive of MLD [Figure 1]. Auditory and ophthalmologic evaluation did not reveal any abnormality. Family screening was normal. Following clinical improvement, she was discharged on sodium bicarbonate, potassium, calcium, Vitamin D, and other multivitamin supplements, showing progress in weight and height on follow-up.
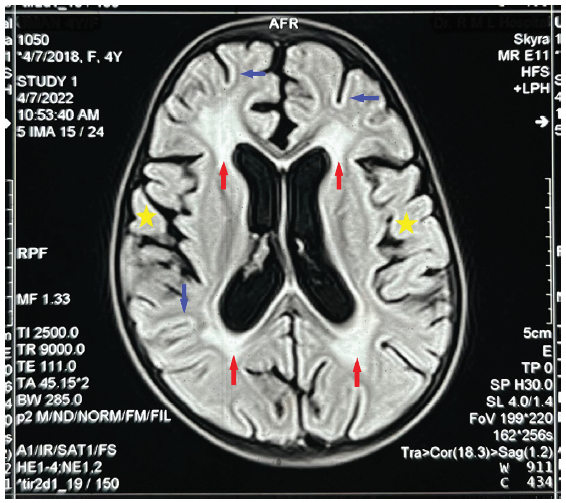
- MRI of the brain showing confluent areas of FLAIR hyperintensities in periventricular white matter, in particular around the posterior periventricular area and frontal horns (red arrows) with sparing of subcortical U-fibers (blue arrows) with mild brain atrophy (yellow stars), AFR: Apparent focal restriction.
Patients with MLD can exhibit kidney involvement due to the systemic nature of the sulfatide accumulation.1 There is a significant paucity of data in the literature on this topic. A two-year-old girl with MLD with proximal RTA was reported in 1978, who demonstrated metachromatic inclusions in the nephron.2 This case underscores the need for further research into the pathophysiological mechanisms linking MLD and renal dysfunction. Management entails correcting electrolyte imbalances, providing supportive care, and addressing complications, emphasizing the importance of a holistic approach in managing such complex cases.
Acknowledgment
The index patient case was from Atal Bihari Vajpayee Institute of Medical Sciences and Dr. Ram Manohar Lohia Hospital, New Delhi, during the corresponding author's senior residency. We thank all personnel involved in the patient's care. The manuscript was developed and edited by the residents of the Department of Pediatrics, Institute of Medical Sciences, BHU, in collaboration with the corresponding author during his pediatric nephrology fellowship. We also appreciate the guidance and assistance of the Department of Pediatrics, IMS-BHU, in preparing and editing this manuscript.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
References
- Arylsulphatase a pseudodeficiency (ARSA-PD), hypertension and chronic renal disease in aboriginal Australians. Sci Rep. 2018;8:10912.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Proximal renal tubular acidosis in metachromatic leukodystrophy. Helv Paediatr Acta. 1978;33:45-52.
- [PubMed] [Google Scholar]







