Translate this page into:
A study of Factors Affecting Dialysis Recovery Time in Haemodialysis Patients in India
Address for correspondence: Dr. B Karthikeyan, Department of Nephrology, Saveetha Medical College Hospital, Thandalam, Chennai, Tamil Nadu, India. E-mail: karthiprakash1986@gmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Patients on maintenance haemodialysis (MHD) often complain of fatigue and tiredness following haemodialysis sessions leading to poor compliance with the dialysis schedule. There is limited Indian data on dialysis recovery time (DRT). The present study was designed to assess the factors affecting DRT in our haemodialysis population.
Methods:
We recorded self-reported patient recovery times of 120 patients who satisfied the inclusion criteria, over three consecutive dialysis sessions by asking the question, 'How long does it take to recover from a dialysis session'? Data recorded included patient factors like age, sex, co-morbidities, Charlson comorbidity index score (CCI), dialysis vintage, duration of kidney disease, interdialytic weight gain (IDWG), treatment factors like ultrafiltration rate (UFR), SpKt/V, blood pump speed, dialysate sodium, session length, pre and post HD blood pressure and laboratory parameters. Health-related quality of life (HRQoL) was assessed with the KDQOL-SF v. 1.3 questionnaire. Results from the SF-36 score were summarised into the physical composite score (PCS), mental composite score (MCS) and kidney disease composite score (KDCS).
Results:
The mean age of the study population was 50.6 ± 12.6 years. Among the 120 patients, 77 (64.2%) were males. Thirty-nine patients (32.5%) were diabetic and 95 (79.1%) patients were hypertensive. The mean dialysis vintage of the study population was 26.1 ± 18.6 months, 41 (34.2%) patients reported DRT <2 h; 48 (40%) reported DRT between 2–6 h and 31 (25.8%) reported DRT >6 h. On multivariate regression analysis, higher IDWG, CCI score and UFR were associated with prolonged DRT. Reported DRT also inversely correlated with PCS (r = - 0.66), MCS (r = - 0.65) and KDCS (r = - 0.59) scores which was statistically significant.
Conclusion:
The present study showed that higher CCI scores, IDWG and UFR were associated with prolonged DRT in Indian haemodialysis patients and patients with longer recovery time had poor HRQoL. Interventions to reduce DRT need to be assessed in further trials in Indian MHD patients.
Keywords
Dialysis recovery time
haemodialysis
interdialytic weight gain
quality of life
ultrafiltration
Introduction
Patients who have end stage renal disease ESRD and are treated with haemodialysis (HD) face a stressful and disruptive chronic illness with a complex and demanding treatment regimen. ESRD patients on maintenance haemodialysis (MHD), after a session of HD, frequently complain of tiredness, weakness, exhaustion, weariness, a sensation of prostration or fatigue.[1] This condition is conventionally called post-dialysis fatigue (PDF).[2] PDF is an often incapacitating syndrome affecting patients undergoing HD that not only worsens patient quality of life[3] but is also associated with cardiovascular events and mortality.[4] Dialysis recovery time (DRT) has been accepted as a measure of PDF. DRT is measured by asking the question, 'How long does it take you to recover from dialysis'? This question is valid, easily interpreted, elicits a clear response, is responsive to change, as well as reliable at a variety of intervals. Besides, it was shown that there was a significant, moderate, positive association between 'time to recover from haemodialysis' (DRT) and several related parameters including mean fatigue, the dialysis stress questionnaire responses, total disease stress, total psychosocial stress and social-leisure activity.[5] Although PDF and DRT are not the same, DRT may be used as an indirect measure of PDF. A longer DRT impairs the quality of life and increases the risk of mortality.[6] Although some reports have suggested that dialysis factors are the most important in determining PDF,[78] others have suggested that patient factors, including age,[9] additional co-morbidities including cerebrovascular disease[10] contribute to PDF.[11] In our centre, PDF is the most common reason cited by patients for skipping their scheduled dialysis session. There is limited Indian data on the factors affecting the DRT. Hence, this study was designed to analyse the factors responsible for prolonged DRT in MHD patients and plan possible interventions accordingly. The effect of DRT on health-related quality of life (HRQoL) in MHD patients was also analysed in this study.
Materials and Methods
The study was performed in the HD unit of Saveetha Medical College hospital, Chennai between January 2020 and March 2020 (3 months). The study has been approved by the Institutional Ethics Committee (IEC), Saveetha Medical College (SMC/IEC/2019/11/005). All patients aged more than 18 years, who were able to respond appropriately to the question about time to recover from dialysis session and who were on MHD for at least 3 months were included in the study. The 141 patients undergoing MHD at our unit were screened for eligibility in the first 2 weeks of the study period. A total of 120 patients were identified and informed consent was obtained for participation in the study. Later, patient recruitment and data collection were completed for all patients over 2.5 months.
All patients were maintained on conventional in-centre HD at least twice per week either through the arteriovenous fistula (AVF) or internal jugular venous catheter (IJVC) and were dialysed using Fresenius 4008S machines with NIPRO-ELISIO 15 M polynephron dialyser with dialyser surface area of 1.5 m2. The dry weight was fixed for each patient every month. The blood flow rate was usually fixed at 300 mL/min for AVFs and 250–300 mL/min for IJVC with dialysate flow rate fixed at 800 mL/min. The endotoxin unit (EU) levels are tested every monthly and disinfection was done weekly to maintain EU levels in the acceptable range. Dialysate sodium was usually fixed at 140 mEq/L but in patients with intradialytic hypertension low dialysate sodium was used as per the decision of the treating nephrologist.
DRT was defined by the question asked to the patients, “How long does it take to recover from a dialysis session”? The question was administered by the first author in the local language (Tamil). The protocol prescribed by Lindsay et al.[5] was followed. Answers given in minutes and hours were recorded directly; variants of half-day and one day were recorded as 12 h (720 min) and 24 h (1440 min), respectively. The recovery time was noted for three consecutive dialysis sessions and the average DRT was noted in hours and converted to minutes as well. Reported DRT was re-classified as <2 h, 2–6 h and >6 h based on a previous study done by Rayner et al.[6]
Demographic and clinical data collected included age, gender, body mass index (BMI), employment status, co-morbidities, Charlson comorbidity index (CCI) (age unadjusted), dialysis vintage, duration of chronic kidney disease CKD, diuretic and erythropoietin use and number of antihypertensive medications. Pre-HD blood samples were collected before the 1st dialysis session and laboratory parameters like serum sodium, potassium, bicarbonate, calcium, phosphorus, haemoglobin and serum albumin were measured. Dialysis related parameters like ultrafiltration rate (UFR), blood flow rate, hypotension episodes, session length, interdialytic weight gain (IDWG), pre and post HD blood pressure were collected for three consecutive sessions and the average was recorded. The single pool Kt/V (6) and prescribed dialysate sodium was recorded for the first dialysis session.
All patients were asked to complete the Kidney Disease Quality of Life Short Form (KDQOL-SFTM) V. 1.3 questionnaire to assess the HRQoL. It is a validated questionnaire that combines the generic SF-36 with a kidney disease-specific instrument. The questionnaire has been validated in the Indian population[1213] and a study with a translated Tamil version[141516] has been published.
The first author verbally administered the survey instrument by an interview and recorded the responses considering the high rates of illiteracy in participants. The questionnaire was administered before HD (in any of the three consecutive sessions) when patients were waiting in the dialysis unit waiting room. Results from SF-36 and kidney disease-specific instruments were summarised into the physical component summary (PCS), mental component summary (MCS) and kidney disease component summary (KDCS). The detailed algorithm of the study is given in Figure 1.
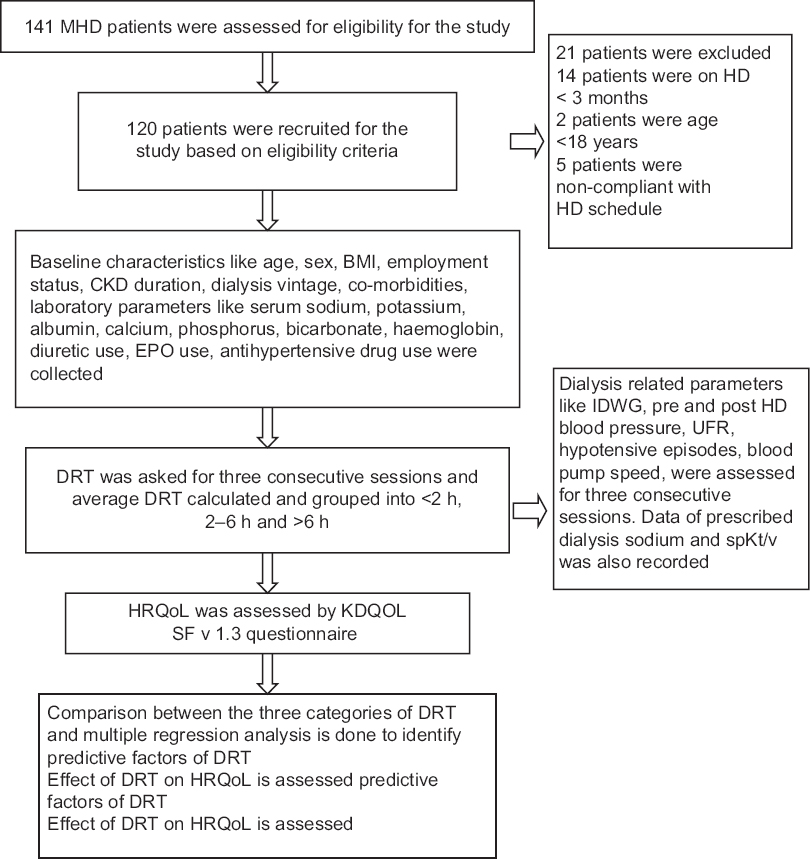
- Algorithm of the study
Statistical analysis
Descriptive statistics was used to determine the means, standard deviation for continuous variables and frequencies/percentages for categorical variables. A comparison of the three categories of DRT was performed using comparing the means for continuous variables and Pearson's Chi-square test for categorical variables. To determine the relationship between DRT and various characteristics, univariate and bivariate analysis was done using a t-test for continuous and Chi-square test for categorical variables, respectively. Multivariate linear regression analysis was performed with DRT as a dependent variable to determine the predictive factors and a P value less than 0.05 was considered significant. Besides, the correlation between DRT at each of the HD sessions was obtained as a measure of test-retest consistency for the question 'how long does it take to recover from the dialysis session'. Spearman's correlation test was used to assess the correlation between DRT and HRQoL. All statistical analysis was done using SPSS software version 20.0.
Results
This study included 120 patients who were on MHD at least twice weekly in the Saveetha Medical College HD unit. The basic demographic details are shown in Table 1.
| Characteristics | Values (mean±SD or n [%]) |
|---|---|
| Age | 50.67±12.94 |
| Male | 77 (64.2%) |
| BMI | 24.49±3.51 |
| Diabetes | 39 (32.5%) |
| Hypertension | 95 (79.1%) |
| CVA | 6 (5%) |
| CAD | 14 (11.6%) |
| Peripheral Neuropathy | 32 (26.7%) |
| Charlson comorbidity index (CCI) | 3.5±1.2 |
| CKD duration (months) | 40.6±30.3 |
| Dialysis Vintage (months) | 26.1±18.6 |
| Full-time employment | 8 (6.7%) |
| Number of the patient on diuretics | 18 (15%) |
| Number of patients using erythropoietin | 116 (96.6%) |
| Haemoglobin (g/dL) | 9.1±1.4 |
| S. Albumin (g/dL) | 3.9±0.5 |
| S. Sodium (mEq/dL) | 135.8±4.2 |
| S. Potassium mEq/dL) | 5.0±0.6 |
| S. Bicarbonate (mEq/dL) | 21.9±1.9 |
| S. Calcium (mg/dL) | 8.4±0.6 |
| S. phosphate (mg/dL) | 4.7±1.0 |
BMI: Body mass index, CAD: Coronary artery disease, CVA: Cerebrovascular accident, UFR: Ultrafiltration rate
The mean DRT of the study population was 7.7 ± 9.3 h (median 4 h, IQR: 2–6.7 h). Patients were categorised into three groups based on their mean DRT for three sessions): 41 (34.2%) patients reported a DRT <2 h; 48 (40%) reported a DRT between 2–6 h and 31 (25.8%) reported a DRT >6 h. There was a strong test retest correlation between sessions (for session 1 and 2, [Pearson's r = 0.97, P = 0.0001]; for session 2 and 3, [Pearson's r = 0.98, P = 0.0001]) On comparing the means and frequencies of various characteristics between different categories of DRT, there was no significant difference between the variables except UFR, IDWG and CCI score [Table 2]. UFR, IDWG and CCI scores were higher in the groups with prolonged DRT.
| Characteristics | DRT < 2 h (N = 41) | DRT 2-6 h (N = 48) | DRT>6 h (N = 31) | P-value |
|---|---|---|---|---|
| Age | 48.2±13.8 | 53.3±10.0 | 49.7±15.1 | 0.16 |
| Male sex | 26 (63.4%) | 27 (56.2%) | 24 (77.4%) | 0.15 |
| BMI (kg/m2) | 23.9±4.0 | 24.6±3.6 | 25.02±2.4 | 0.41 |
| Diabetes | 10 (24.4%) | 17 (34.4%) | 12 (38.7%) | 0.37 |
| Hypertension | 32 (78%) | 38 (79.2%) | 25 (80.6%) | 0.96 |
| CVA | 1 (2.4%) | 1 (2.1%) | 4 (12.9%) | 0.07 |
| CAD | 6 (14.6%) | 2 (4.2%) | 6 (14.6%) | 0.09 |
| Peripheral neuropathy | 10 (24.4%) | 10 (20.8%) | 12 (38.7%) | 0.19 |
| Age unadjusted CCI | 3.24±1.3 | 3.33±1.1 | 4.10±1.1 | 0.03 |
| Employment status | 8 (19.5%) | 4 (8.3%) | 1 (3.2%) | 0.07 |
| IJVC | 4 (9.8%) | 3 (6.2%) | 4 (12.9%) | 0.59 |
| AVF | 37 (90.2%) | 45 (93.7%) | 27 (87%) | 0.35 |
| HD frequencyTwice weeklyThrice weekly | 39 (95.1%)2 (4.9%) | 47 (97.9%)1 (2.1%) | 29 (93.5%)2 (6.5%) | 0.56 |
| Session length (hours) | 4.0±0.0 | 4.02±0.14 | 4.0±0.07 | 0.54 |
| Single pool Kt/V | 1.20±0.07 | 1.22±0.06 | 1.22±0.07 | 0.49 |
| Dialysate Sodium (<140 mEq/L) | 3 (7.3%) | 4 (8.3%) | 6 (19.3%) | 0.20 |
| Blood pump speed (mL/min) | 266.8±36.3 | 269.3±23.9 | 278.7±23.9 | 0.20 |
| Number of patients with hypotension episodes | 5 (35.7%) | 4 (28.5%) | 5 (35.7%) | 0.56 |
| CKD duration (months) | 37.4±22.0 | 42.4±37.5 | 42.0±27.6 | 0.70 |
| Dialysis vintage (months) | 27.7±19.5 | 23.5±19.7 | 28±15.6 | 0.46 |
| IDWG | 2.8±0.6 | 3.4±0.4 | 3.9±0.7 | <0.001 |
| Hb | 9.0±1.4 | 9.2±1.2 | 9.0±1.7 | 0.80 |
| Albumin | 3.9±0.4 | 3.9±0.5 | 3.9±0.4 | 0.65 |
| Sodium | 136.1±4.2 | 134.9±3.7 | 136.9±4.7 | 0.09 |
| Potassium | 5.1±0.7 | 4.9±0.5 | 5.0±0.6 | 0.10 |
| Calcium | 8.4±0.5 | 8.4±0.6 | 8.5±0.8 | 0.81 |
| Phosphorus | 4.8±1.0 | 4.5±1.0 | 5.0±1.0 | 0.15 |
| Bicarbonate | 22.0±1.5 | 22.0±2.2 | 21.7±2.1 | 0.81 |
| UFR (mL/kg/h) | 10.92±1.86 | 11.51±2.27 | 13.23±2.92 | <0.001 |
| Diuretic use | 4 (9.7%) | 8 (16.6%) | 6 (19.3%) | 0.48 |
| EPO use | 40 (97.5%) | 47 (97.9%) | 29 (93.5%) | 0.53 |
| Pre HD systolic BP (mmHg) | 152.72±13.36 | 157.61±16.45 | 154.46±13.39 | 0.35 |
| Pre HD diastolic BP (mmHg) | 84±7.33 | 83.16±6.98 | 83.69±8.28 | 0.88 |
| Post HD systolic BP (mmHg) | 149.52±26.97 | 156.83±16.18 | 151.51±12.7 | 0.22 |
| Post HD diastolic BP (mmHg) | 81.6±7.8 | 81.51±8.9 | 81.8±9.0 | 0.87 |
| Number of antihypertensive medications0 | 6 (14.6%) | 10 (20.8%) | 3 (9.6%) | 0.47 |
| 1 | 15 (36.5%) | 19 (39.5%) | 11 (35.4%) | |
| 2 | 13 (31.7%) | 14 (29.1%) | 8 (25.8%) | |
| ≥3 | 7 (17.1%) | 5 (10.4%) | 9 (29%) |
BMI: Body mass index, CAD: Coronary artery disease, CVA: Cerebrovascular accident, UFR: Ultrafiltration rate, Hb: Haemoglobin, IJVC: Internal jugular vein catheter, AVF: Arteriovenous fistula, CCI: Charlson comorbidity index
In the multivariate regression analysis, increase in UFR (P = 0.04), IDWG (P < 0.001) and CCI score (P = 0.03) is significantly associated with prolonged DRT [Table 3]. Other variables like age, gender, individual co-morbidities, dialysis vintage, blood pump speed, SpKt/V, dialysis session length, hypotensive episodes, pre and post HD blood pressure, haemoglobin, s. albumin, serum sodium, serum potassium, serum calcium and serum phosphorus were not significantly associated with DRT. HRQoL was assessed in 117 patients with the KDQOL-SF v. 1.3 questionnaire. There was a significant difference in all the scores (PCS, MCS and KDCS) between the groups. The mean scores were lower in the category having DRT >6 h [Table 4]. Reported DRT was inversely correlated with PCS (r = - 0.66), MCS (r = - 0.65) and KDCS (r = -0.59) scores which was statistically significant.
| Variables | Beta | P-value | Confidence interval (95% CI) |
|---|---|---|---|
| Age | -0.05 | 0.36 | (-0.17 --- 0.06) |
| Gender (Male) | 0.765 | 0.62 | (-2.295 --- 3.824) |
| Dialysis vintage | -0.022 | 0.61 | (-0.106---0.063) |
| CCI | 1.377 | 0.03 | (0.125 – 2.628) |
| UFR | 0.696 | 0.04 | (0.006---1.386) |
| Dialysate sodium | -4.215 | 0.07 | (-8.915 ---0.485) |
| IDWG | 4.877 | <0.001 | (2.70--- 7.055) |
| S. Albumin | 1.447 | 0.36 | (-1.67--- 4.57) |
CCI: Charlson comorbidity index, UFR: Ultrafiltration rate (mL/kg/h), IDWG- Interdialytic weight gain
| Variables | Overall | DRT < 2 hours | DRT 2-6 hours | DRT > 6 hours | P-value |
|---|---|---|---|---|---|
| PCS | 26.77±7.89 | 33.52±4.64 | 25.46±6.09 | 20.07±7.12 | <0.001 |
| MCS | 47.99±13.05 | 59.38±7.81 | 45.41±10.52 | 37.32±10.93 | <0.001 |
| KDCS | 58.17±11.23 | 65.43±7.47 | 58.66±7.85 | 47.94±12.32 | <0.001 |
PCS – Physical composite summary, MCS- Mental composite summary, KDCS – Kidney disease component score
Discussion
The present study was aimed at identifying the various factors associated with prolonged DRT in Indian patients on MHD. There is limited data on DRT in Indian HD patients. The present study looks at 120 patients maintained on conventional in-centre HD in our dialysis unit. In our MHD population, 79 (65.8%) patients reported DRT of more than 2 h and 31 (25.8%) patients had reported more than 6 h to recover from dialysis sessions. There was a high test-retest correlation between the DRT and the question 'how long does it take to recover from a dialysis session'. CCI score, IDWG and UFR were found to be significantly associated with prolonged DRT.
Charlson comorbidity score and DRT
The mean CCI score in our study population was 3.5 ± 1.2. Patients with prolonged DRT were found to have higher co-morbidity scores. This indicates that patients with multiple co-morbid conditions are more prone to have prolonged DRT. The study done by Rayner et al.[6] showed co-morbid conditions like diabetes and psychiatric disorders were associated with longer recovery time. Other similar studies done by Awuah et al.[17] and Bossola[18] et al. did not find any association between the co-morbid conditions and DRT. However, in these studies, the presence or absence of co-morbidities was noted rather than scoring based on severity. The exact pathophysiology behind how the presence of multiple co-morbidities prolongs DRT is not well understood. In our study, most patients with high CCI scores had diabetes (which can increase fatigue)[19] with associated co-morbid conditions like CVA, peripheral neuropathy and CAD. The number and severity of co-morbidities may be associated with anorexia, stress, depression, tiredness, weakness and exhaustion[20] which may be the cause for prolonged DRT in patients with high CCI scores.[21]
IDWG, UFR and DRT
In this study, the mean IDWG and UFR of the study population were 3.3 ± 0.7 kg and 11.75 ± 2.49 mL/kg/h, respectively. Higher IDWG and UFR were associated with prolonged DRT [Table 3]. The study done by Hussein et al.[22] also noted that rapid fluid removal was associated with prolonged DRT. The study by Rayner et al.[6] showed that both fast (>15 mL/min) and slow ultrafiltration (<5 mL/min) were associated with shorter DRT. However, the study done by Awuah et al.[17] did not find any association between UFR and DRT. Patients with higher IDWG were usually subjected to more ultrafiltration and when UFR is higher it prolong the DRT. Most of our patients were non-compliant to fluid restriction and were doing twice-weekly HD which leads to high IDWG and so high UFR. Reducing the IDWG by compliance with fluid restriction and reducing UFR by more frequent dialysis would help shorten the DRT.
The DRT was not associated with age, sex, BMI, employment status, dialysis vintage, session length, blood flow rate, SpKt/V, pre and post HD blood pressure, number of antihypertensive drug use, diuretic use, erythropoietin use, prescribed dialysate sodium, serum electrolytes levels and intradialytic hypotensive episodes. These findings were in contrast to the study done by Rayner et al.[6] where elderly age, dialysis vintage, BMI, diabetes and psychiatric disorder were associated with longer recovery time. However, the study done by Awuah et al.[17] had not found any significant association between recovery time and other variables. Another study done by Yoowannakul[23] et al. showed that younger patients had prolong recovery time than elderly patients. Most of the studies gave conflicting results regarding the associated factors with DRT.[1822232425] Multicentric studies including a larger sample size in Indian HD patients may be needed to find out the other significant variables that predict DRT.
There is no individualised prescription of dialysate sodium in our unit which led to most of our patients (90%) being dialysed with prescribed dialysate sodium of 140 mEq/L during the study period. Around 10% of patients were dialysed with low sodium dialysate (<140 mEq/L). These patients had a history of intradialytic hypertension episodes for which low dialysate sodium had been prescribed by the treating nephrologist. In the multivariate analysis, patients dialysed with dialysate sodium < 140 mEq/L were associated with longer recovery time but this did not reach statistical significance. Lower dialysate sodium has been associated with longer recovery time in the study done by Rayner et al.[6] The effect of dialysate sodium on DRT needs to be assessed in future intervention trials in Indian MHD patients.
Many patients feel fatigued and they require rest or sleep following the dialysis session which affects the quality of life. The pathophysiology behind the delayed DRT is incompletely understood. HD causes rapid shift of electrolytes and water between the cell membranes that can lead to delay in recovery time.[6] These changes may be increased after a stressful dialysis session leading to prolonged recovery time. In our study, patients with high IDWG leading to high UFR (rapid fluid shift) during the dialysis session can be the reason for the delay in recovery time.
DRT and HRQoL
In this study, the QoL in dialysis patients was assessed by the KDQoL SFv1.3 questionnaire. After informed consent, nearly 98% of patients were able to respond to the HRQoL questionnaire to calculate PCS, MCS and KDCS. Our study showed that patients with prolonged DRT had poor QoL compared to those with shorter recovery time. The study by Rayner et al. showed that patients with longer recovery time had lower PCS and MCS scores and had a poor QoL.[6] Our study showed similar results wherein patients who had DRT more than 6 h had low PCS and MCS scores [Table 4]. There was a significant inverse correlation between the QoL and the PCS (r = -0.69), MCS (r = -0.68) and KDCS (r = -0.55) scores. A study by Lindsay et al.[5] in MHD patients also noted the association of prolonged recovery time with poor QoL. In the DOPPS study,[6] patients with longer recovery time were at increased risk of hospitalisation and mortality. There is little evidence on the pathophysiology of how prolonged recovery time affects the QoL. Excessive fatigue, sleepiness, the sense of feeling low and having less energy following HD may be the possible reason for poor HRQoL scores in patients with prolonged DRT.
There is limited Indian data regarding how DRT affects the QoL in MHD patients. This is probably one of the first Indian studies regarding DRT in MHD patients to our knowledge. There is high test-retest consistency showing that the interpretation of the question by patients was fairly constant.
The limitations of the study are its small sample size and that this was a single-centre, observational study. Answers to the question were subjective and there is no supportive objective measurement of the recovery time. Other laboratory parameters like serum magnesium, iron profile and intact PTH levels were not recorded for these patients. Outcomes like hospitalisation and mortality were not assessed in this study as our main aim was to find the factors predicting DRT. Although this was a simple study, it can pave the way for future multicentre and interventional studies in DRT, especially in Indian MHD patients.
Conclusion
The present study concludes that DRT is associated with poor QoL in Indian HD patients. CCI score, IDWG and UFR are significantly associated with prolonged recovery time. Other parameters like age, sex, serum albumin, haemoglobin and dialysis vintage were not associated with DRT. Hence, interventions to reduce DRT such as reducing the UFR by more frequent dialysis, reducing IDWG by patient education and adjustment in dialysate sodium need to be assessed in further trials in Indian HD patients.
Financial support and sponsorship
Nil
Conflicts of interest
Nil
References
- Postdialysis fatigue: A frequent and debilitating symptom. Semin Dial. 2016;29:222–7.
- [Google Scholar]
- Health-related quality of life among dialysis patients on three continents: The dialysis outcomes and practice patterns study. Kidney Int. 2003;64:1903–10.
- [Google Scholar]
- Fatigue in patients receiving maintenance dialysis: A review of definitions, measures, and contributing factors. Am J Kidney Dis. 2008;52:353–65.
- [Google Scholar]
- Minutes to recovery after a hemodialysis session: A simple health-related quality of life question that is reliable, valid, and sensitive to change. Clin J Am Soc Nephrol. 2006;1:952–9.
- [Google Scholar]
- Recovery time, quality of life, and mortality in hemodialysis patients: The dialysis outcomes and practice patterns study (DOPPS) Am J Kidney Dis. 2014;64:86–94.
- [Google Scholar]
- Recovery time after hemodialysis is inversely associated with the ultrafiltration rate. Blood Purif. 2019;47:45–51.
- [Google Scholar]
- Patients receiving frequent hemodialysis have better health-related quality of life compared to patients receiving conventional hemodialysis. Kidney Int. 2017;91:746–54.
- [Google Scholar]
- Identification of factors responsible for postdialysis fatigue. Am J Kidney Dis. 1999;34:464–70.
- [Google Scholar]
- Patients' perspective of haemodialysis-associated symptoms. Nephrol Dial Transplant. 2011;26:2656–63.
- [Google Scholar]
- Patient's response to a simple question on recovery after hemodialysis session strongly associated with scores of comprehensive tools for quality of life and depression symptoms. Qual Life Res. 2014;23:2247–56.
- [Google Scholar]
- Assessment of quality of life in chronic renal failure patients in India. Quality issues and insights in the 21st century. 2012;1:9.
- [Google Scholar]
- Cross-cultural adaptation, validation and reliability of the South Indian (Kannada) version of the Kidney Disease and Quality of Life (KDQOL-36) instrument. Saudi J Kidney Dis Transplant. 2015;26:1246–52.
- [Google Scholar]
- Assessment of quality of life in chronic kidney disease patients using the kidney disease quality of life-short form questionnaire in indian population: A community based study. Asian J Pharm Clin Res. 2015;8:271–4.
- [Google Scholar]
- Assessment of health-related quality of life and its determinants in patients with chronic kidney disease. Indian J Nephrol. 2017;27:37-43.
- [Google Scholar]
- Quality of life of patients undergoing hemodialysis. Asian J Pharm Clin Res. 2018;11:219–23.
- [Google Scholar]
- Time to recovery after a hemodialysis session: Impact of selected variables. Clin Kidney J. 2013;6:595–8.
- [Google Scholar]
- Variables associated with time of recovery after hemodialysis. J Nephrol. 2013;26:787–92.
- [Google Scholar]
- Fatigue is associated with serum interleukin-6 levels and symptoms of depression in patients on chronic hemodialysis. J Pain Symptom Manage. 2015;49:578–85.
- [Google Scholar]
- Appetite is associated with the time of recovery after the dialytic session in patients on chronic hemodialysis. Nephron Clin Pract. 2013;123:129-33.
- [Google Scholar]
- Higher ultrafiltration rate is associated with longer dialysis recovery time in patients undergoing conventional hemodialysis. Am J Nephrol. 2017;46:3–10.
- [Google Scholar]
- Patient-reported intra-dialytic symptoms and post-dialysis recovery times are influenced by psychological distress rather than dialysis prescription. Ren Replace Ther. 2019;5:14.
- [Google Scholar]
- Effect of daily hemodialysis on depressive symptoms and postdialysis recovery time: Interim report from the FREEDOM (Following Rehabilitation, Economics and Everyday-Dialysis Outcome Measurements) Study. Am J Kidney Dis. 2010;56:531-9.
- [Google Scholar]
- The effect of blood flow rate on dialysis recovery time in patients undergoing maintenance hemodialysis: A prospective, parallel-group, randomized controlled trial. Hemodial Int. 2019;23:223-9.
- [Google Scholar]







