Translate this page into:
An Abysmal Quadrad: A Rare Case of Ankylosing Spondylitis, Ulcerative Colitis, and Takayasu Aortoarteritis Complicated by Secondary Renal Amyloidosis
Corresponding author: Dr. Pallavi Prasad, MD, DNB (Nephrology), Assistant Professor, Vardhman Mahavir Medical College and Safdarjung Hospital, Ansari Nagar East, Near to AIIMS Metro Station, New Delhi - 110 029, Delhi, India. E-mail: pallaviprasad1986@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Banker H, Prasad P, Kumar A, Mahajan S, Kumar R, Batra V. An Abysmal Quadrad: A Rare Case of Ankylosing Spondylitis, Ulcerative Colitis, and Takayasu Aortoarteritis Complicated by Secondary Renal Amyloidosis. Indian J Nephrol. 2024;34:267–9. doi: 10.4103/ijn.ijn_294_23
Abstract
Ankylosing Spondylitis (AS) is a chronic inflammatory arthritis that typically manifests in young males and may present with extra-articular manifestations. Takayasu aortoarteritis (TA) is a large vessel vasculitis that predominantly affects young and middle-aged females. Despite the limited number of studies examining the potential association between these two diseases, we report a unique case of an individual with ankylosing spondylitis and ulcerative colitis who subsequently developed Takayasu aortoarteritis. This progression ultimately led to the development of secondary renal amyloidosis, attributed to a combination of inflammatory pathologies.
Keywords
Ankylosing spondylitis
amyloidosis
Takayasu
vasculitis
aortoarteritis
Introduction
Ankylosing spondylitis (AS) is a chronic inflammatory disorder primarily affecting the axial skeleton. It is strongly associated with human leukocyte antigen (HLA) B27 and related conditions such as inflammatory bowel disease (IBD), reactive arthritis, and uveitis. Takayasu aortoarteritis (TA) is a large vessel vasculitis that primarily affects the aorta and its major branches. In this report, we present a rare case of a young male with AS and ulcerative colitis (UC), who later developed TA, the combination of which culminated into renal amyloidosis (RA).
Case Report
An 18-year-old male patient presented with a chronic history of low back pain and stiffness in the hips. On examination, the dorsolumbar spine showed limited ante- and lateral flexion [see Table 1 for detailed investigations]. He was diagnosed with AS and initiated on nonsteroidal anti-inflammatory drugs (NSAIDs) and physiotherapy. After 3 months, he developed frequent episodes of loose stools and fever. Colonoscopy revealed ulcers in the sigmoid colon, along with loss of vascular pattern in the transverse and ascending colon, with colonic biopsy showing cryptitis, crypt abscess, and crypt loss, consistent with UC. Treatment with sulfasalazine and prednisolone (1 mg/kg/d) was initiated, which was tapered after achieving disease remission.
| Investigations | At the time of AS diagnosis | At the time of UC diagnosis | At the time of TA diagnosis | At the time of AKI diagnosis | At the time of RA diagnosis | On treatment (current) |
|---|---|---|---|---|---|---|
| Hb (g/dl) | 10.4 | 10.4 | 12.4 | 9.8 | 8.3 | 9.5 |
| WBC (per mm3) | 11,860 | 18,500 | 12,900 | 13,420 | 14,300 | 8900 |
| CRP (mg/dl) | 181.9 | 7 | 95.6 | 63.9 | 17.7 | s |
| ESR (mm/h) | 95 | 70 | 76 | 56 | 55 | |
| S. ALP (IU/l) | 174 | 106 | 157 | 94 | ||
| Rheumatoid factor | Negative | |||||
| Anti-CCP (IU/ml) | Negative (<25) | |||||
| HLA B27 | Positive | |||||
| ANA | Negative | Negative | ||||
| C3, C4 | Negative | |||||
| PR3-ELISA | Negative | |||||
| MPO-ELISA | Negative | |||||
| Anti-ds-DNA | Negative | |||||
| Creatinine (mg/dl) | 0.8 | 0.78 | 0.6 | 9.8 | 2.6 | 1.6 |
| Urea (mg/dl) | 25 | 14 | 154 | 57 | 43 | |
| Serum albumin (g/dl) | 4.2 | 4.4 | 3.7 | 2.2 | 2.6 | 2.9 |
| Urine albumin | Nil | Nil | Nil | 3+ | 3+ | 3+ |
| Urine RBC | Nil | Nil | Nil | Nil | Nil | Nil |
| Urine WBC | Nil | Nil | Nil | Nil | Nil | Nil |
| 24-h urine protein (g/24 h) | 2.6 | 1.2 | ||||
| Radiologic investigations |
X ray bilateral hip uniform reduction of bilateral hip joint space with subchondral sclerosis. MRI both hips Reduced joint space along bilateral hip joint with mild join effusion, synovitis, and subchondral marrow edema along bilateral femoral head and acetabulum (L>>R). AKI=acute kidney injury, S.ALP=serum alkaline phosphatase, MPO- myeloperoxidase, ANA=anti-nuclear antigen, Anti-CCP=anti-cyclic citrullinated peptide, anti-ds-DNA=anti-double-stranded DNA antibody, AS=ankylosing spondylitis, C3, C4=complement factor 3, complement factor 4, CRP=C-reactive protein, ELISA=enzyme-linked immunosorbent assay, ESR=erythrocyte sedimentation rate, Hb=hemoglobin, HLA=human leukocyte antigen, RA=renal amyloidosis, RA factor=rheumatoid arthritis factor, RBC=red blood cells, TA=Takayasu arteritis, UC=ulcerative colitis, WBC=white blood cells
Two years later, the patient presented with sudden-onset transient blurring of vision in the left eye with headache. Investigations showed raised inflammatory markers. Eye examination showed no signs of uveitis. A thorough physical examination revealed a blood pressure (BP) difference between the left arm (124/78 mmHg) and the right arm (150/90 mmHg), with low pulse volume in the left arm and a bruit over the left common carotid artery (CCA). Magnetic resonance (MR) aortography [Figure 1] showed wall thickening and enhancement in the aortic arch (AoA), descending thoracic aorta (DTA), and upper abdominal aorta (AA), with nearly complete occlusion of left CCA and luminal narrowing of bilateral proximal subclavian (L > R) and vertebral arteries. A diagnosis of TA was made in light of these findings [Table 1] and prednisolone (1 mg/kg/d) was started, which led to a symptomatic improvement. However, a follow-up positron emission tomography (PET) scan at 6 months revealed increased metabolic uptake along the walls of ascending aorta, AoA, DTA, left CCA, and left subclavian arteries, despite therapy. He was advised infliximab, but he could not afford the same and was lost to follow-up.
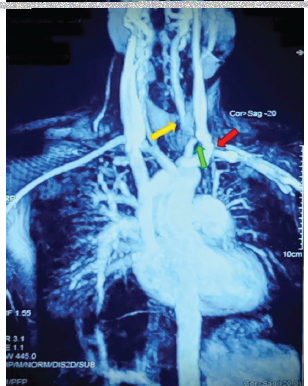
- MR angiography of aorta and its branches shows wall thickening with enhancement of AoA, DTA, and upper AA with nearly complete occlusion of left common carotid artery (green arrow) and luminal narrowing of proximal subclavian (red arrow) and vertebral arteries (yellow arrow). AA = abdominal aorta, AoA = aortic arch, DTA = descending thoracic aorta, MR = magnetic resonance, NCCT: non contrast computerised tomographic scan.
Six months later, he presented with acute gastroenteritis and oliguria. Investigations showed elevated blood urea, serum creatinine, and albuminuria. With fluids and antibiotics, stool consistency and urine output improved. However, a follow-up after 3 weeks revealed persistent hypoalbuminemia, proteinuria, and increased serum creatinine compared to baseline [Table 1]. A kidney biopsy was done, which was suggestive of AA amyloidosis [Figure 2]. The patient was diagnosed with AS-associated UC and TA with secondary RA. Telmisartan and dapagliflozin were started, after which proteinuria improved. The necessity of biologic therapy was discussed with the patient, with infliximab planned once his financial constraints are resolved.
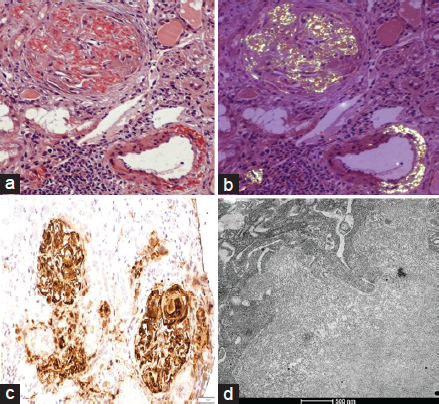
- Histopathologic examination of kidney biopsy. (a) Congo red stain 200× showing amyloid deposits in the mesangium and focally in peripheral capillaries. (b) Congo red stain 200× showing apple green birefringence on polarized light. (c) Serum amyloid A (SAA) stain 200× showing positive deposits of amyloid in the mesangium and focally in peripheral capillary walls. (d) Electron microscopy 17,500 × shows basement membrane showing randomly arranged fibrils with a mean cross diameter of 9.97 mm.
Discussion
AS often exhibits extra-articular manifestations. Cardiac manifestations include ascending aortitis, valvular regurgitation, and cardiac conduction abnormalities, but association with TA is rare.1 Our case showed arteritis involving the carotid arteries, DTA, and AoA, suggesting TA rather than spondyloarthropathy-related aortitis. The largest case series of TA with spondyloarthropathies (n = 14) primarily describes middle-aged women with a high rate of HLA B27 negativity. In most cases, spondyloarthropathy precedes TA, with a median time gap of 4.5 years between the two conditions.1 However, our patient was a young male, was HLA B27 positive, and had a short duration of 2 years between diagnosis of AS and TA (despite having previous exposure to steroids, which could have delayed the symptomatology of TA).
Renal involvement is often observed in both AS and TA. In AS, the most common cause of renal involvement is IgA nephropathy.2 The incidence of RA in AS has been reported as 6.1%.3 On the other hand, TA primarily involves renal vessels with resulting renovascular hypertension and ischemic nephropathy. RA is rare in TA.4,5 A single retrospective cohort from Russia reports amyloidosis in TA with an incidence of 3.9%, speculating genetic susceptibility versus other ethnicities.6
Our case presented with amyloidosis 6 years after AS diagnosis and 2 years after TA diagnosis. Previous studies have shown a median time gap of 12 years between AS and RA3 and 13 years between TA and RA.6 The coexistence of multiple inflammatory disorders likely contributed to accelerated development of secondary RA in this case. While infliximab was recommended, financial constraints prevented its initiation. Currently, the patient receives the best possible supportive care and is under monitoring to assess the response to therapy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
References
- Takayasu arteritis and spondyloarthritis: Coincidence or association? A study of 14 cases. J Rheumatol. 2017;44:1011-7.
- [CrossRef] [PubMed] [Google Scholar]
- Spectrums and prognosis of kidney disease in patients with ankylosing spondylitis. Kidney Dis (Basel). 2020;6:444-52.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Renal amyloidosis in ankylosing spondylitis: A monocentric study and review of literature. Saudi J Kidney Dis Transpl. 2018;29:386-91.
- [CrossRef] [PubMed] [Google Scholar]
- AA amyloidosis in Takayasu’s arteritis--long-term survival on maintenance haemodialysis. Nephrol Dial Transplant. 1999;14:2478-81.
- [CrossRef] [PubMed] [Google Scholar]
- Renal AA Amyloidosis leading to early diagnosis and treatment of takayasu arteritis: A case report and review of the literature. Clin Res Cardiol. 2020;109:1438-41.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- AA Amyloidosis in a cohort of 128 patients with Takayasu’s arteritis. J Vasc. 2017;3:120.
- [Google Scholar]







